Abstract
Case presentation
We report on a German leprosy patient originating from Pakistan who had a relapse more than 5 years after completion of multi-drug therapy (MDT) of his first episode of multibacillary (MB) leprosy. State-of-the-art laboratory techniques (histopathology, PGL-I serology, microscopy and DNA/RNA qPCR) were applied for laboratory confirmation and monitoring of treatment outcome. Serology indicated the relapse long before the presence of unambiguous clinical signs. At the time of diagnosis of the relapse the patient had a remarkably high bacterial load suggesting increased risk for a second relapse. Furthermore, unexpectedly prolonged excretion of viable bacilli through the upper respiratory tract for more than 3 months after onset of MDT was shown. Therefore, MDT was administered for 2 years.
Discussion and conclusions
The clinical course of the patient, as well as the prolonged excretion of viable bacilli, underlines the usefulness of laboratory assessment. Laboratory tools including up-to-date molecular assays facilitate rapid diagnosis, timely MDT, identification of individuals excreting viable bacilli and patients at risk for relapses, monitoring of treatment outcome and respective adaptation of treatment where appropriate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Leprosy caused by Mycobacterium leprae is a neglected, chronic infectious disease predominantly affecting skin and peripheral nerves. The disease is spectral and categorized according to the Ridley–Jopling classification based on type of lesions and bacterial load in correlation with the degree of cell-mediated immunity into tuberculoid, lepromatous and borderline forms. Alternatively a simplified, field-based classification considering the number of skin lesions introduced by the WHO distinguishes paucibacillary (PB, up to five skin lesions) and multibacillary (MB, more than five skin lesions) forms [1, 2].
Still more than 200,000 new cases are reported each year suggesting ongoing transmission, which is assumed to take place by aerosol spread through the upper respiratory tract. Although time spans ranging from months to 30 years have been reported, incubation periods are estimated at 2–12 years. The index of manifestation of M. leprae is considered low, but it is not known how many infected people actually proceed from subclinical infection to clinical disease. The risk of developing clinically manifest leprosy when infected by M. leprae has been associated with genetic factors, poverty and low socio-economic status. In particular household contacts of untreated leprosy patients are at high risk of disease which is estimated 5–10 times greater for contacts of MB patients compared to non-contacts, and 2–3 times greater for contacts of PB cases [1,2,3,4,5].
Whereas previously PB patients were treated for 6 months with rifampicin and dapsone and MB patients for 12 months with rifampicin, dapsone and clofazimine, current WHO recommendations valid since August 2018 envisage to treat PB patients for 6 months and MB patients for 12 months with rifampicin, dapsone and clofazimine (multi-drug therapy, MDT) [6]. Based on the results of mouse-footpad tests it is generally assumed that due to the potent bactericidal effect of rifampicin, infectiousness of patients becomes unlikely after start of treatment. On the other hand, it is known that MB patients can excrete up to 10,000,000 bacteria per day and it has also been demonstrated that inoculation of human biopsy material derived from MB patients after 12 months of MDT still results in mycobacterial multiplication in 15% of the cases [3, 4, 7]. Likewise, relapses are considered a rare event, treatable with a second course of MDT. However, a number of studies provided evidence that the risk of relapse is correlated with the bacterial load before treatment and in subsets of patients with a bacterial index (BI) ≥ 3 10–20% relapses have been observed. Therefore, treatment for more than 12 months may be advisable for those patients [1, 3, 8, 9].
As a result of increasing immigration a number of European countries where leprosy was considered eradicated or controlled have begun to give attention to imported cases, and e.g., England, Germany, Portugal and Spain regularly report to the WHO Global Health Observatory data repository. There are, however, no uniform criteria for case definitions, laboratory confirmation or reporting obligations. During the last decade Germany, for example reported up to five cases per year, a German case is however only notifiable if laboratory confirmed, preferably by nucleic acid detection [10,11,12].
Case presentation
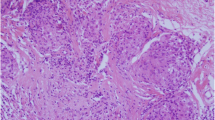
In March 2009, a 40-year-old patient of Pakistani origin who has been living in Germany for more than 20 years presented at our outpatient department with multiple, macular, hyperpigmented (reddish), painless lesions on trunk and extremities with moderate hyposensitivity. The lesions had occurred 1 year ago subsequent to a family visit in Pakistan in October 2008. The patient had erythematous swellings in the face and on the hands, and both earlobes were thickened and reddened. The clinical diagnosis of MB leprosy was laboratory confirmed by means of positive PCR as well as Ziehl–Neelsen microscopy of skin smears and nasal swabs (bacteriological index, BI 1+), a high titer of anti-PGL-I antibodies (> 100 antibody units [AU]) according to the method described by Sticht Groh in 1992 with minor modifications according to standardized procedures of our accredited laboratory and characteristic histopathological findings (foam cells, acid fast bacilli) of a skin biopsy of a macular lesion [13]. The patient was treated with 12 months MDT. Furthermore, the patient received prednisolone for 12 weeks due to a type I reverse reaction (indicated by numbness on the dorsum of both feet). The prednisone treatment started 4 weeks after initiation of MDT with a dosage of 40 mg (per day) and was reduced stepwise to 5 mg (per day) from week 6 onward. The numbness began to resolve after 2 weeks.
The clinical symptoms had completely receded in May 2010 and a significant decrease of anti-PGL-I antibodies (< 30 AU in September 2012) was noted. From then on clinical and laboratory follow-up of the patient including PGL-I serology was done in yearly intervals.
In October 2015, the patient presented at our outpatient department with painful swelling and morning stiffness of the middle finger joints without rubor and calor. A significant rise of the anti-PGL-I antibody level (> 100 AU) was noted, unambiguous clinical signs of a relapse were however absent. The diagnosis of rheumatoid arthritis was made elsewhere and the patient received methotrexate therapy over 6 weeks.
In February 2016, the patient presented again at our outpatient department with multiple, macular, erythematous lesions indicative for a relapse of MB leprosy. This time confirmed by histopathology of a skin biopsy of a macular lesion, Ziehl–Neelsen microscopy and RLEP qPCR (repetitive element RLEP of the M. leprae genome) of a skin biopsy and nasal swab samples, as well as an unaltered high anti-PGL-I antibody titer. The bacillary load of the patient as determined by microscopy (nasal swab: BI 4+) and quantification by RLEP qPCR (skin biopsy: ~ 300,000 bacteria in 100 µl extract, nasal swab: ~110,000 bacteria in 100 µl extract) was remarkably high [14]. Molecular drug resistance testing at the Global Health Institute of the Ecole Polytechnique Fédérale de Lausanne, Switzerland, was conducted according to standardized methods used by the WHO surveillance network for antimicrobial resistance in leprosy and revealed no resistance to rifampicin, dapsone or ofloxacin [15, 16]. Furthermore, the morphological index (MI, i.e., the proportion of solid stained bacilli) was > 30% per nasal swab sample. Based on the assumption that solid stained bacilli are viable, whereas non-solid stained bacilli are dead, the MI according to the method described by McRae and Shepard indicates whether leprosy is active and has been used for a long time to monitor treatment response. However, the reliability of the MI is limited as multiplication of M. leprae from non-solid organisms has been reported [17, 18]. A molecular viability assay (16S rRNA RT qPCR [14, 19]; supplementary material 1) proved the presence of viable M. leprae in nasal swab samples. Subsequently the patient was put on a second course of MDT (due to delay in delivery the medication started with two doses of rifampicin and MDT was given with 11 days delay). Furthermore, the patient received prednisolone for 16 weeks due to a type I reverse reaction (indicated by numbness in the toes and outer edge of the right foot). The prednisone treatment started 4 weeks after initiation of MDT with a dosage of 40 mg (per day) and was reduced to 30 mg from week 7 onward, to 20 mg from week 9 onward, to 10 mg from week 13 onward and to 5 mg from week 17 to week 20. The numbness began to resolve after 2 weeks.
In close collaboration with the treating physicians of the outpatient department, treatment monitoring was conducted by means of microscopy (BI, MI), quantification of bacillary load by RLEP qPCR (providing the total number of viable and dead bacilli), viability assessment by 16S rRNA RT qPCR of nasal swab samples and PGL-I serology. A tenfold decrease of bacillary load was noted 3 days after start of rifampicin treatment. However, the RNA assay detected viable bacilli in nasal swab samples until day 110 after start of treatment, and solid stained bacilli were seen until day 67 (BI 2 +; MI 10%). Within 6 months anti-PGL-I antibodies decreased again to low levels and have remained around 30 AU since then.
An overview of the case is given in Fig. 1.
A1–A3 February 2016: multiple, macular, erythematous lesions on trunk and extremities, earlobes thickened and reddened. B Anti-PGL-I titer over time: antibody units < 10: negative; 10–14: borderline; > 14: positive. C Bacterial load in nasal swab samples after initiation of relapse treatment: quantification with RLEP qPCR (bacilli per nasal swab sample [100 µl], blue curves) and microscopy (bacilli per 100 microscopy fields [× 100 oil immersion], green curves). In the background of the graph two methods for measuring viability are displayed: 16S rRNA RT qPCR (RNA detection from nasal swab samples, vertical dark grey lines if positive) and microscopy (morphological index > 1% [> 1% of the bacilli found solid stained], vertical red dotted lines if positive). D Microscopic images of nasal swab samples of the patient since initial dose of rifampicin (day 1): D1 26-Feb-2016 (day 1; BI 4 +; MI 50%); D2 27-Feb-2016 (day 2; BI 3 +; MI 37%); D3 2-May-2016 (day 67; BI 2 +; MI 10%); D4 23-Aug-2017 (day 545; BI 1 +; MI 0%)
Discussion and conclusions
Underlined by the consistent application of laboratory tools for long-term monitoring of treatment, our patient presents a number of noteworthy features from which one can derive valuable information for the management of leprosy, which are of particular importance in countries where the clinical knowledge of leprosy has disappeared.
Despite a low bacillary load and full treatment compliance during the first episode of illness, the patient had a relapse which was possibly boosted by anti-rheumatic therapy but would have occurred irrespectively of therapeutic immunosuppression. In accordance with data from Gelber et al., indicating the elapsed time between end of therapy and relapse with an average of 6 years, the relapse occurred more than 5 years after completion of MDT. If feasible, follow-up of MB patients should cover at least that time span, or better be extended up to 10 years to ensure identification of early relapses (assumedly due to insufficient treatment) as well as late relapses (assumedly due to persisting bacilli). In addition to clinical examination, laboratory assessment should be an integral component of follow-up, in particular monitoring of bacillary load and anti-PGL-I antibody titers, which are both powerful early indicators for relapses before the appearance of definite clinical signs. However, it must be noted that these diagnostic tools are only applicable for MB patients [5, 8, 9, 20]. Furthermore, the diagnostic tools described above may not be available in low-income settings and shipment of diagnostic samples to reference laboratories abroad may be required. Multiple relapses have been reported and the initially high bacillary load at the beginning of the second episode of illness clearly assigns our patient to the group of those at high risk for further relapse. Therefore, MDT was administered for 24 months, accompanied by continuous clinical and laboratory assessment [1, 3, 9].
In the case of the current relapse of our patient molecular assays not only facilitated exact quantification of the bacillary load in nasal swab samples before and under treatment, but also revealed the most unexpected, prolonged excretion of viable M. leprae through the upper respiratory tract. The infectious dose of M. leprae is only known for mice (14–140 AFB or 3.4–34 solid stained/viable AFB) and not for humans [21]. However, the exceedingly high number of bacilli initially detected in a single nasal swab of our patient (~ 110,000 AFB) suggests infectivity for contact persons during the presumably more than 6-monthly time interval between onset of relapse and start of treatment. Despite the tenfold decrease of bacterial load after onset of treatment, considering the prolonged detection of viable bacilli infectivity cannot be entirely dismissed for the more than 3-monthly timespan between onset of MDT and negativity of the RNA assay.
With increasing international migration cases of leprosy may occur more often in countries outside endemic areas such as Germany and other European countries where awareness and knowledge of this disease have become low or absent. In terms of crowding, poor hygienic standards and low socio-economic status living conditions in camps for first accommodation of newly arrived refugees and asylum seekers provide precisely the risk factors that may favor the transmission of M. leprae from untreated MB patients excreting large amounts of viable bacteria [10].
It can be concluded that laboratory-based assessment of suspected leprosy cases including up-to-date molecular tools facilitates rapid diagnosis and timely MDT, thus largely reducing the risk for transmission. Furthermore, laboratory-based follow-up of patients allows monitoring of treatment outcome, evaluation of infectivity and detection of individuals excreting viable bacilli over an extended period of time. In addition, it supports the use of preventive measures such as wearing of protective masks or sick leave where appropriate, as well as identification of patients prone to relapses and in need for extended MDT or alternative treatment regimens such as the probatory combination of MDT with bactericidal second line drugs, or MDT for 24 months or until smear negativity, which was shown to be beneficial for patients with high initial BIs [1, 22,23,24].
References
Britton WJ, Lockwood DN. Leprosy. Lancet. 2004;363:1209–19.
Rodrigues LC, Lockwood DNJ. Leprosy now: epidemiology, progress, challenges, and research gaps. Lancet Infect Dis. 2011;11:464–70.
WHO. WHO Expert Committee on Leprosy—Eighth report, vol. 68. Geneva: World Health Organ Tech Rep Ser; 2012. pp. 1–61.
Reibel F, Cambau E, Aubry A. Update on the epidemiology, diagnosis, and treatment of leprosy. Med Mal Infect. 2015;45:383–93.
Araujo S, Freitas LO, Goulart LR, Goulart IMB. Molecular evidence for the aerial route of infection of Mycobacterium leprae and the role of asymptomatic carriers in the persistence of leprosy. Clin Infect Dis. 2016;63:1412–20.
Guidelines for the diagnosis. Treatment and prevention of leprosy. New Delhi: World Health Organization, Regional Office for South-East Asia; 2018.
Shetty VP, Khambati FA, Ghate SD, Capadia GD, Pai VV, Ganapati R. The effect of corticosteroids usage on bacterial killing, clearance and nerve damage in leprosy; Part 3—study of two comparable groups of 100 multibacillary (MB) patients each, treated with MDT 1 steroids vs MDT alone, assessed at 6 months post—release from 12 months MDT. Lepr Rev. 2010;81:41–58.
Gelber RH, Balagon VF, Cellona RV. The relapse rate in MB leprosy patients treated with 2-years of WHO-MDT is not low. Int J Lepr Other Mycobact Dis. 2004;72:493–500.
Shetty VP, Wakade AV, Ghate SD, Pai VV. Clinical, bacteriological and histopathological study of 62 referral relapse cases between Jan 2004 and Dec 2009 at the Foundation for Medical Research, Mumbai. Lepr Rev. 2011;82:235–43.
Massone C, Brunasso AM, Noto S, Campbell TM, Clapasson A, Nunzi E. Imported leprosy in Italy. J Eur Acad Dermatol Venereol. 2012;26:999–1006.
Ramos JM, Romero D, Belinchón I. Epidemiology of leprosy in Spain: the role of the international migration. PLoS Negl Trop Dis. 2016;10:e0004321.
Robert-Koch-Institut, Berlin. Steckbriefe seltener und importierter Infektionskrankheiten. 2011. https://edoc.rki.de/bitstream/handle/176904/3724/steckbriefe.pdf. Accessed 01 Jul 2019.
Sticht Groh V, Alvarenga AE. Use of a different buffer system in the phenolic glycolipid-I ELISA. Int J Lepr. 1992;60:570–4.
Beissner M, Wöstemeier A, Saar M, Badziklou K, Maman I, Amedifou C et al. Development of a combined RLEP/16S rRNA (RT) qPCR assay for the detection of viable M. leprae from Nasal Swab samples. BMC Infect Dis. 2019 (accepted Jul 2019).
Benjak A, Avanzi C, Sigh P, Loiseau C, Girma S, Busso P, et al. Phylogenomics and antimicrobial resistance of the leprosy bacillus Mycobacterium leprae. Nat Commun. 2018;9:352–62.
Cambeau E, Saunderson P, Matsuoka M, Cole ST, Kai M, Suffys P, et al. Antimicrobial resistance in leprosy: results of the first prospective open survey conducted by a WHO surveillance network for the period 2009–15. Clin Microbiol Infect. 2018;24:1305–10.
Mc Rae DH, Shepard CC. Relationship between the staining quality of Mycobacterium leprae and infectivity for Mice. Infect Immun. 1971;3:116–20.
Katoch CM, Katoch K, Ramu GM, Sharma VD, Datta AK, Shivannavar CT, Desikan KV. In vitro methods for determination of viability of mycobacteria: comparison of ATP content, morphological index and FDA-EB fluorescent staining in Mycobacterium leprae. Lepr Rev. 1988;59:137–43.
Martinez AN, Lahiri R, Pittman TL, Scollard D, Truman R, Moraes MO, Williams DL. Molecular determination of Mycobacterium leprae viability by use of real-time PCR. J clin Microbiol. 2009;47:2124–30.
Chin-A-Lien RAM, Faber WR, van Rens MM, Leiker DL, Naafs B, Klatser PR. Follow-up of multibacillary leprosy patients using a phenolic glycolipid-I-based ELISA. Do increasing ELISA-values after discontinuation of treatment indicate relapse? Lepr Rev. 1992;63:21–7.
Shepard CC, McRae DH. Mycobacterium leprae in Mice: minimal infectious dose, relationship between staining quality and infectivity, and effect of cortisone. J Bacteriol. 1965;98:365–72.
Lockwood DN, Kumar B. Treatment of leprosy. BMJ. 2004;328:1447–8.
Ebenezer GJ, Daniel S, Norman G, Daniel E, Job CK. Are viable Mycobacterium leprae present in lepromatous patients after completion of 12 months’ and 24 months’ multi-drug therapy? Indian J Lepr. 2004;76:199–206.
Duthie MS, Orcullo FM, Abbelana J, Maghanoy A, Balagon MF. Comparative evaluation of antibody detection tests to facilitate the diagnosis of multibacillary leprosy 2016. Appl Microbiol Biotechnol. 2016. https://doi.org/10.1007/s00253-016-7328-8.
Acknowledgements
The authors thank Mrs. Kerstin Helfrich and Mrs. Carolin Mengele for excellent laboratory assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards statement
Approval by the appropriate ethics committee is not applicable. The patient sought medical advice at our outpatient department and was subjected to routine clinical and laboratory procedures. Like all patients seeking medical advice through our institute, also this patient routinely signed a consent form approving the collection of data and samples. The form is approved by the institutional ethics review board of the Medical Center of the University of Munich (LMU).
Informed consent
Written informed consent to publish case history and pictures was obtained from the patient.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1
As an additional file the run protocol of the 16S rRNA RT qPCR used for viability assessment is attached (PDF 127 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Saar, M., Hanus, I., Huber, K. et al. Report on an unusual case of leprosy from Germany: just an exception of the rule?. Infection 47, 1065–1069 (2019). https://doi.org/10.1007/s15010-019-01349-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-019-01349-8