Abstract
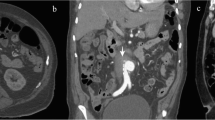
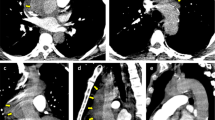
Non-typhoidal Salmonella (NTS) spp. causes about 40% of all infective aortitis and it is characterized by high morbidity and mortality. Human infection occurs by fecal–oral transmission through ingestion of contaminated food, milk, or water (inter-human or zoonotic transmission). Approximately 5% of patients with NTS gastroenteritis develop bacteremia and the incidence of extra-intestinal focal infection in NTS bacteremia is about 40%. The organism can reach an extra-intestinal focus through blood dissemination, direct extension from the surrounding organs and direct bacterial inoculation (e.g. invasive medical procedures). Medical and surgical interventions are both needed to successfully control the infection. Here, we report a case of abdominal sub-renal aortitis caused by Salmonella enterica serovar Enteritidis in an 80-year-old man.





Similar content being viewed by others
References
Hakim S, Davila F, Amin M, Hader I, Cappell MS. Infectious aortitis: a life-threatening endovascular complication of nontyphoidal salmonella bacteremia. Case Rep Med. 2018. https://doi.org/10.1155/2018/6845617.
Strahm C, Lederer H, Schwarz EI, Bachli EB. Salmonella aortitis treated with endovascular aortic repair: a case report. J Med Case Rep. 2012;6(1):1. https://doi.org/10.1186/1752-1947-6-243.
Molacek J, Treska V, Baxa J, Certik B, Houdek K. Acute conditions caused by infectious aortitis. Aorta. 2014;2(3):93–9. https://doi.org/10.12945/j.aorta.2014.14-004.
Parekh PJ, Shams R, Challapallisri V, Marik PE. Successful treatment of Salmonella aortitis with endovascular aortic repair and antibiotic therapy. BMJ Case Rep. 2014. https://doi.org/10.1136/bcr-2014-204525.
Guo Y, Bai Y, Yang C, Wang P, Gu L. Mycotic aneurysm due to Salmonella species: clinical experiences and review of the literature. Braz J Med Biol Res. 2018;51(9):1–9. https://doi.org/10.1590/1414-431X20186864.
Kommaraju K, Brinster DR. Endovascular abdominal aortic stent grafting in unrecognized salmonella aortitis. Vasc Endovasc Surg. 2012;46(5):431–4. https://doi.org/10.1177/1538574412449393.
Nakayama M, Fuse K, Sato M, et al. Infectious aortitis caused by Salmonella Dublin followed by aneurysmal dilatation of the abdominal aorta. Intern Med. 2012;51(20):2909–11. https://doi.org/10.2169/internalmedicine.51.7937.
Montrivade S, Kittayarak C, Suwanpimolkul G, Chattranukulchai P. Emphysematous Salmonella aortitis with mycotic aneurysm. BMJ Case Rep. 2017. https://doi.org/10.1136/bcr-2017-220520.
Kub CT, Kub TCT, Diseases I, Act R. Salmonella aortitis—a case of mistaken identity. ANZ J Surg. 2010;80(4):284–5. https://doi.org/10.1111/j.1445-2197.2010.05245.x.
Looi JL, Cheung L, Lee APW. Salmonella mycotic aneurysm: a rare cause of fever and back pain in elderly. Int J Cardiovasc Imaging. 2013;29(3):529–31. https://doi.org/10.1007/s10554-012-0115-4.
Erbel R, Aboyans V, Boileau C, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases. Russ J Cardiol. 2015;123(7):7–72. https://doi.org/10.15829/1560-4071-2015-07-7-72.
Luo C, Ko W, Kan C, Lin P, Yang J. In situ reconstruction of septic aortic pseudoaneurysm due to Salmonella or Streptococcus microbial aortitis: long-term follow-up. J Vasc Surg. 2003;38:975–82. https://doi.org/10.1016/s0741-5214(03)00549-4.
Mangioni D, Bonera G, Bonardelli S, Castelli F, Stellini R. Abdominal aortitis and aneurysm impending rupture during pneumococcal meningitis. Lancet Infect Dis. 2016;16(8):980. https://doi.org/10.1016/S1473-3099(16)30114-1.
Acknowledgements
We thank the participants who contributed to this report.
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Informed consent
A consent for the use of the clinical data was provided.
Rights and permissions
About this article
Cite this article
Gardini, G., Zanotti, P., Pucci, A. et al. Non-typhoidal Salmonella aortitis. Infection 47, 1059–1063 (2019). https://doi.org/10.1007/s15010-019-01344-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-019-01344-z