Abstract
Objectives
Enterococcal bacteremia can be complicated by infective endocarditis (IE) and when suspected, transesophageal echocardiography (TEE) should be performed. The previously published NOVA score can identify patients with enterococcal bacteremia at risk for IE and we aimed to improve the score.
Methods
Factors associated with IE were studied retrospectively in a population-based cohort of patients with monomicrobial Enterococcus faecalis bacteremia (MEFsB). Factors associated with IE in multivariable analysis were included in a new score system which was compared to the NOVA score and validated in a cohort of patients with MEFsB from another region.
Results
Among 397 episodes of MEFsB, 44 episodes with IE were compared to those without IE. Long Duration of symptoms (≥ 7 days) and Embolization were associated with IE in the multivariate analysis and hence were added to the NOVA variables (Number of positive cultures, Origin of infection unknown, Valve disease, and Auscultation of murmur) to generate a novel score; DENOVA. The area under the curve in ROC analyses was higher for DENOVA (0.95) compared to NOVA (0.91) (p = 0.001). With a cutoff at ≥ 3 positive variables the DENOVA score has a sensitivity of 100% and specificity of 83% which is superior to the NOVA score (specificity 29%). The DENOVA score was applied to the validation cohort (26 IE episodes and 256 non-IE episodes) and the resulting sensitivity was 100% and the specificity was 85% compared to 35% for NOVA.
Conclusions
The DENOVA score is a useful tool to identify patients with MEFsB where TEE is not needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Enterococci are part of the normal human gut flora and can cause severe infections including urinary tract infections, gastrointestinal infections, catheter-related infections, and infective endocarditis (IE). IE is defined by the modified Duke criteria [1] in which the identification of a causative bacterium and echocardiographic evidence of endocardial infection are major criteria.
Enterococcal bacteremia is a relatively common condition and has a mortality rate of around 20% [2, 3]. A substantial proportion of patients with enterococcal bacteremia are diagnosed with IE [2, 4,5,6], and recent population-based studies suggest that up to 25% of patients with community-acquired Enterococcus faecalis bacteremia (EFsB) have this condition [5, 6]. A number of factors have been associated with the presence of IE in enterococcal bacteremia including the species E. faecalis compared to other enterococci [3, 4, 6, 7], prosthetic heart valves [3, 5, 7], heart murmur [2, 4], previous endocarditis [5], other valve disease [2,3,4,5], embolization [4], monomicrobial bacteremia [2, 3, 5], a high number of positive cultures [3, 4], an unknown focus of infection [2, 4, 5], community acquisition, subacute syndrome [2], age [2, 3], and male sex [2, 5]. It is important to detect all cases of IE since the condition has a high mortality, and cure necessitates a long treatment course with a combination of antibiotics and sometimes surgery. Therefore, a scoring system to identify which patients with enterococcal bacteremia that have IE has to have a sensitivity close to 100%. Transesophageal echocardiography (TEE) is the method of choice to diagnose IE and identifies changes compatible with IE with a higher sensitivity than transthoracic echocardiography (TTE) [4]. However, TEE is a semi-invasive, resource-demanding procedure which is not readily available at all sites and it is not without discomfort for the patient. Thus, TEE should only be performed when there is a risk of IE. For this purpose, a diagnostic score termed NOVA [Number of positive blood cultures ≥ 3 (5 points), Origin of infection unknown (4 points), Valve disease (2 points) and Auscultation of heart murmur (1 point)] was developed by Bouza et al. meant to guide the use of TEE in enterococcal bacteremia [4]. The authors set the cutoff at 4 points, meaning that TEE is recommended in patients with three or more positive cultures (N) or unknown origin of infection (O). The NOVA score was later validated in an adapted form and was found to have a high sensitivity (97%) but limited specificity (23%) [5]. The majority of cases with enterococcal IE is due to E. faecalis and have a monomicrobial blood culture and in such cases IE should be considered [2, 4, 5]. We therefore aimed to improve the NOVA score using easy accessible clinical parameters in a population-based cohort of patients with monomicrobial E. faecalis bacteremia (MEFsB) from southern Sweden and to externally validate the NOVA score and the improved score in another cohort of patients from a tertiary referral center in another part of Sweden.
Methods
Calibration cohort
All consecutive blood cultures positive for E. faecalis from January 2012 through December 2016 were obtained from the database of the Laboratory for Clinical Microbiology in Skåne County, in southern Sweden. This is the only laboratory in the region and has a catchment area of 1.3 million inhabitants and nine hospitals. The medical records of patients with MEFsB were studied retrospectively. Data collection was carried out from 90 days prior to an episode until 1 year after the episode. Patients under the age of 18 years or where medical records could not be retrieved were excluded. Ethical approval was obtained from the Ethics Committee of Lund University (2013/31).
Definitions
A detailed description of data collection and definitions is given in supplementary material 1. An episode was defined as a clinical situation in which a patient had MEFsB and the episode was ended after 7 days of effective treatment. IE was defined using the modified Dukes criteria considering definite cases only as IE [1]. Scoring of patients was performed using the information available to the clinician at the time of the receipt of the positive blood culture results. NOVA score parameters were defined as described by Bouza et al. [4] with modifications of number of cultures as described by Dahl et al. [5]. The origin of infection (O in NOVA, definition not detailed by Bouza et al. [4]) was defined as a focal infection (fulfillment of at least two of the following criteria (a) typical signs or symptoms of infection, (b) isolation of E. faecalis at the site of infection, and (c) imaging results compatible with focal infection which was likely to be the point of entry for the bacteria. Valve disease in NOVA (V) was defined as a history of any of the predisposing heart conditions that constitute a high or moderate risk of developing IE, including (1) native valve disease, (2) previous IE, or (3) the presence of a valve prosthesis [8, 9]. Auscultation of murmur (A in NOVA) included those with any murmur reported. Duration of symptoms was defined as the number of days before the first positive blood culture was taken with any symptom compatible with IE. Embolization was defined by signs on clinical examination or by findings using imaging techniques. A previous EFsB was defined as a blood culture with growth of E. faecalis, within the previous 90 days preceding an episode. Community and health-care site of acquisition was defined as previously described [10], whereas nosocomial acquisition was defined as a blood culture drawn after 48 or more hours of hospitalization [11]. Comorbidities were classified according to the Charlson index [12].
Validation cohort
The validation cohort was from Karolinska University Hospital, Stockholm, Sweden, a tertiary referral center serving the Stockholm County with a population of 2.3 million inhabitants. All blood culture data for patients with growth of enterococci were retrieved from January 2012 through December 2016 from the Department of Clinical Microbiology, Karolinska University Hospital. Records from patients with MEFsB were studied retrospectively and data were collected as described for the calibration cohort above. Ethical approval was obtained from the ethics committee review board in Stockholm (Dnr 2015/1184-31).
Statistics
For the results to be valid in the clinical setting, all episodes of MEFsB were included in the analyses. Hence, each patient could have more than one episode. To account for repeated events, we applied the statistical method generalized estimation equations (GEE). This method takes into account clustering and was used both in univariate and multivariate analyses [13]. P values are based on GEE estimates with a significance level of < 0.05. For the multivariate model, we were limited by the number of IE outcomes in the calibration test set (n = 44). We first performed a multivariate model that included all variables significantly associated with IE in univariate analyses. We then removed variables from the model that were not significantly associated with the outcome.
Results
Calibration cohort
653 patients with EFsB were identified, of whom 36 were excluded since they were < 18 years old, 6 due to lack of access to medical files, and 249 because they had polymicrobial bacteremia. The 362 included patients had 397 episodes of MEFsB, of which 44 episodes in 44 patients (11%) fulfilled the Duke criteria for IE (Supplementary material 2). Four episodes, in which the Dukes criteria were not fulfilled, were treated as possible IE by the physician.
Most patients (336) had only one episode of MEFsB. However, 26 patients had at least one more episode of MEFsB (in total, 35 additional episodes). The first episode was a non-IE in all these patients, but six of these patients later had an episode with IE. 153 patients died within the study period of 360 days for reasons presumed to be unrelated to IE based on comorbidities, clinical presentation, and absence of positive blood culture for EFs.
Differences in distribution of variables between episodes of IE and non-IE that could tentatively be included in a score are given in Table 1 with odds ratios and significance levels. Additional information on the treatment, investigations, and outcome is given in Supplementary material 3. In the univariate analysis, the number of positive blood cultures, unknown origin of infection, valve disease, heart murmur, a long duration of symptoms, embolization, age, community acquisition, and previous EFsB were associated with IE. These variables were included in a multivariate model. Community acquisition, previous EFsB, and valve disease were not significantly associated with IE in the multivariate analysis and were thus removed from the model. Furthermore, we removed age from the model since this variable resulted in very large standard errors of other estimates indicating a numerical problem.
In the final multivariate model, symptom duration, embolization, number of positive blood cultures, unknown origin of infection, and heart murmur were associated with IE (Table 2). These variables were included in a novel score, and despite not being significantly correlated with IE in multivariate analysis, we chose to include also the valve disease criterion of NOVA in our new score to conform with earlier studies [4, 5]. The novel score was termed DENOVA and each variable was given one point to make it easy to use (Table 2).
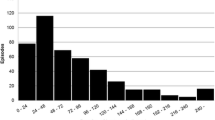
The DENOVA score was tested for its ability to separate episodes with IE from episodes without IE and the resulting receiver operator characteristics (ROC) curve had an area under the curve (AUC) of 0.95 (95% CI, 0.94–0.97) compared to the adapted NOVA score which had a significantly lower AUC of 0.91 (95% CI, 0.89–0.95) (p = 0.001 for difference) (Fig. 1). With a cutoff at ≥ 3 points DENOVA had a sensitivity of 100% and a specificity of 83% to identify episodes of IE in MEFsB, while at the suggested cutoff of 4 points [4], the NOVA score had a sensitivity of 100% and a specificity of 29%.
Receiver operator characteristics (ROC) curve for the ability of the NOVA (blue) and DENOVA (red) score to separate episodes with IE from non-IE episodes. The inset shows the number of episodes of IE (black bars) and non-IE (gray bars) in relation to the score obtained using DENOVA (data from the calibration cohort)
Validation cohort
The NOVA and the DENOVA score were validated in a separate cohort of 485 patients with EFsB, 233 patients were excluded due to polymicrobial bacteremia (n = 168), age under 18 years (n = 42), or unavailable records (n = 23). Finally, 268 episodes in 252 patients were included in the analyses, 26 classified as IE and 242 as non-IE.
The majority (238 patients) had only one episode of MEFsB. Sixteen episodes, 4 with IE and 12 non-IE, were followed by a new episode within 360 days. The episodes that followed an IE were always another episode of IE. Six non-IE episodes were followed by a new non-IE and six were followed by an episode of IE. Two patients had three episodes. 62 patients died within 360 days because of reasons presumed to be unrelated to IE.
The characteristics of patients in the validation cohort were similar to that of the calibration cohort, though some differences were noted (Supplementary material 4).
When the DENOVA score was applied to the validation cohort, the resulting ROC curve had an AUC of 0.95 (95% CI, 0.93–0.98) which was significantly higher than that of the adapted NOVA (AUC 0.92 (95% CI 0.88–0.95), p = 0.007). At the predefined cutoff of three points, DENOVA had a sensitivity of 100% and a specificity of 85% compared to the NOVA score (with cutoff 4 [4]) with a sensitivity of 100% and a specificity of 35%.
Combining the calibration and validation cohorts and analyzing the subgroup of patients where echocardiography had been performed, DENOVA had a sensitivity of 100% and a specificity of 62%. The numbers needed to screen to find one case of IE was 2.4 for DENOVA (≥ 3) and 7 for NOVA (> 4).
Discussion
Bacteremia with enterococci is a condition which can be complicated by IE, and tools to aid clinicians, to decide whether echocardiography should be performed, are potentially very useful. We propose the use of the DENOVA scoring system to guide the use of TEE in MEFsB. Importantly, DENOVA had a high sensitivity and specificity both in the original cohort and in the separate validation cohort. DENOVA had a higher specificity than the previously proposed NOVA score and the number needed to screen to find one case of IE was 2.4 for DENOVA, as compared to 7 for NOVA. Using DENOVA to guide the use of TEE could reduce the number of procedures for patients at low risk of IE and the costs for the health-care system. Moreover, DENOVA is easy to use since each variable gives one point as compared to the more differentiated NOVA score [4]. Another strength of our study is that the DENOVA score was generated in a population-based cohort avoiding the potential bias of single center studies and further it was validated in a separate cohort, from a referral hospital with partly different epidemiology, with similar performance. Finally, our design avoids the bias introduced when patients subjected to TEE with a finding of IE are compared to patients subjected to TEE without a finding of IE (a type of over-matching) such as in the study behind the NOVA score [4]. When we applied the DENOVA score only to patients that had undergone echocardiography, the sensitivity was still 100%, whereas the specificity dropped to 62%. This was expected since the decision by the treating physician to perform TEE was likely based on a perceived increased risk for IE.
However, there are several limitations to this study. First, the DENOVA score cannot be applied to E. faecium bacteremia and not to polymicrobial EFsB. In both these conditions, IE is uncommon [2, 4, 6] and separate very large studies would be needed to adapt the score to these conditions. Secondly, the retrospective design of our study makes it sensitive to misclassification, potentially non-differential. For example, a clinician who suspects IE might be more prone to take additional blood cultures, make a more thorough heart auscultation, or look for emboli, which will potentially increase the DENOVA score. Further external validation and most importantly prospective studies are needed to address this concern.
Thirdly, a limited number of patients underwent TEE in our study. This is a common problem in this type of studies [4, 5, 14, 15] and a consequence of the retrospective design. Even in prospective studies, however, a high frequency of TEE in bacteremia is not always obtained [16] and, importantly, a negative TEE does not rule out the presence of IE or that a visible vegetation can develop after TEE. To assess the risk of misclassification, we followed the patients for 360 days. Patients with a non-IE MEFsB were rarely treated more than 14 days and it is thus unlikely that a misclassified IE would have been without a relapse. However, a large number of patients died within 360 days after a non-IE episode (142 and 62 in the calibration and validation cohorts, respectively). We cannot rule out that some of these patients died from a missed IE, yet the analysis of patient records did not indicate that this was the cause of death. The proportion of patients diagnosed with IE was very similar in our cohort and a recent Danish cohort also indicating that we did not miss a substantial number of IE cases [6].
In patients with multiple MEFsB episodes, the first classified as non-IE, in both the calibration and validation cohort together, a new episode of IE was detected in 12 patients during 360 days of follow-up. In eight of these, no TEE was done during the first episode. The initial episodes might thus have been misclassified in these cases. However, DENOVA score in these eight episodes was ≥ 3 in five cases, which would have been subjected to TEE if DENOVA would have been used.
In summary, the use of DENOVA in clinical decision-making will help physicians to focus echocardiographic investigations on persons at high risk for IE.
References
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG, Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633–8.
Maki DG, Agger WA. Enterococcal bacteremia: clinical features, the risk of endocarditis, and management. Medicine (Baltimore). 1988;67:248–69.
Fernández-Guerrero ML, Herrero L, Bellver M, Gadea I, Roblas RF, de Górgolas M. Nosocomial enterococcal endocarditis: a serious hazard for hospitalized patients with enterococcal bacteraemia. J Intern Med. 2002;252:510–5.
Bouza E, Kestler M, Beca T, Mariscal G, Rodríguez-Créixems M, Bermejo J, et al. The NOVA score: a proposal to reduce the need for transesophageal echocardiography in patients with enterococcal bacteremia. Clin Infect Dis. 2015;60:528–35.
Dahl A, Lauridsen TK, Arpi M, Sørensen LL, Ostergaard C, Sogaard P, et al. Risk factors of endocarditis in patients with Enterococcus faecalis bacteremia: external validation of the NOVA score. Clin Infect Dis. 2016;63:771–5.
Pinholt M, Ostergaard C, Arpi M, Bruun NE, Schønheyder HC, Gradel KO, et al. Incidence, clinical characteristics and 30-day mortality of enterococcal bacteraemia in Denmark 2006–2009: a population-based cohort study. Clin Microbiol Infect. 2014;20:145–51.
Anderson DJ, Murdoch DR, Sexton DJ, Reller LB, Stout JE, Cabell CH, et al. Risk factors for infective endocarditis in patients with enterococcal bacteremia: a case-control study. Infection. 2004;32:72–7.
Dajani AS, Bisno AL, Chung KJ, Durack DT, Freed M, Gerber MA, et al. Prevention of bacterial endocarditis. Recommendations by the American Heart Association. JAMA. 1990;264:2919–22.
Steckelberg JM, Wilson WR. Risk factors for infective endocarditis. Infect Dis Clin N Am. 1993;7:9–19.
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care–associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002;137:791–7.
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–40.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
David W, Hosmer J, Lemeshow S, Sturdivant R. Applied logistic regression. Third. Wiley. 2013. pp. 313–76.
Holland TL, Arnold C, Fowler VG. Clinical management of Staphylococcus aureus bacteremia: a review. JAMA. 2014;312:1330–41.
Palraj BR, Baddour LM, Hess EP, Steckelberg JM, Wilson WR, Lahr BD, et al. Predicting risk of endocarditis using a clinical tool (PREDICT): scoring system to guide use of echocardiography in the management of Staphylococcus aureus bacteremia. Clin Infect Dis. 2015;61:18–28.
Tubiana S, Duval X, Alla F, Selton-Suty C, Tattevin P, Delahaye F, et al. The VIRSTA score, a prediction score to estimate risk of infective endocarditis and determine priority for echocardiography in patients with Staphylococcus aureus bacteremia. J Infect. 2016;72:544–53.
Acknowledgements
This work was supported by the Swedish Government Fund for Clinical Research (ALF), the Stockholm County Council, the foundations of Marianne and Marcus Wallenberg, Crafoord, Österlund. Lundgren, and the Royal Physiographic Society in Lund. We acknowledge the advice by Dr Per Åkesson and the invaluable help of Mrs. Lena Hyllebusk at the Department for Clinical Microbiology, Lund. Part of this work has been presented at the ISCVID meeting in Dublin 2017.
Author information
Authors and Affiliations
Contributions
MR concieved the study and wrote the manuscript together with AB. All authors contributed to the design of the study. AK, AB and HÖ collected data and PN performed statistical analyses. All authors contributed to the writing and gave their final consent.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Berge, A., Krantz, A., Östlund, H. et al. The DENOVA score efficiently identifies patients with monomicrobial Enterococcus faecalis bacteremia where echocardiography is not necessary. Infection 47, 45–50 (2019). https://doi.org/10.1007/s15010-018-1208-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1208-3