Abstract
Purpose
Antibiotic stewardship programs (ASP) optimize antibiotic usage and combat antibiotic resistance of bacteria. The objective of this study was to assess the impact of specific ASP interventions on antibiotic consumption in general pediatric wards.
Methods
We conducted a prospective study to compare a pre-intervention (Sept.–Dec. 2014) and post-intervention (Sept.–Dec. 2015) period. An ASP bundle was established including (1) infectious diseases (ID) ward rounds (prospective-audit-with-feedback), (2) ID consultation service, (3) internal guidelines on empiric antibiotic therapy. Medical records on four general pediatric wards were reviewed daily to analyze: (1) antibiotic consumption, (2) antibiotic dosage ranges according to local guidelines, and (3) guideline adherence for community-acquired pneumonia (CAP).
Results
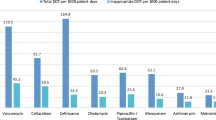
Antibiotic prescribing for 273 patients (pre-intervention) was compared to 263 patients (post-intervention). Antibiotic prescription rate did not change (30.6 vs. 30.5%). However, overall days-of-therapy and length-of-therapy decreased by 10.5 and 7.7%, respectively. Use of cephalosporins and fluoroquinolones decreased by 35.5 and 59.9%, whereas the use of penicillins increased by 15.0%. An increase in dosage accuracy was noted (78.8 vs. 97.6%) and guideline adherence for CAP improved from 39.5 to 93.5%. Between the two study periods, no adverse effects regarding length of hospital stay and in-hospital mortality were observed.
Conclusions
Our data demonstrate that implementation of an ASP was associated with a profound improvement of rational antibiotic use and, therefore, patient safety. Considering the relatively short observation period, the long-term effects of our ASP bundle need to be further investigated.




Similar content being viewed by others
Abbreviations
- ASP:
-
Antibiotic stewardship program
- ATC:
-
Anatomical therapeutic chemical
- CAP:
-
Community-acquired pneumonia
- CDI:
-
Clostridium difficile–infection
- CMI:
-
Case mix index
- CPOE:
-
Computerized physician order entry
- DDD:
-
Defined daily dose
- DGI:
-
German Society of Infectious Diseases
- DoT:
-
Days of antibiotic therapy
- ESBL:
-
Extended spectrum β-lactamase producing Gram-negative bacteria
- FQ:
-
Fluoroquinolone
- ID:
-
Infectious diseases
- IDSA:
-
Infectious Diseases Society of America
- i.v.:
-
Intravenous
- LMU:
-
Ludwig-Maximilians-University
- LoT:
-
Length of antibiotic therapy
- ME:
-
Medication errors
- MRGN:
-
Multi-resistant Gram-negative bacteria
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- PD:
-
Patient-days
- p.o.:
-
Oral
- RDD:
-
Recommended daily dose
- VRE:
-
Vancomycin-resistant Enterococcus
- WHO:
-
World Health Organization
References
Bundesamt für Verbraucherschutz und Lebensmittelsicherheit PEG eV. GERMAP 2015–Bericht über den Antibiotikaverbrauch und die Verbreitung von Antibiotikaresistenzen in der Human- und Veterinärmedizin in Deutschland. 2016. http://www.p-e-g.org/econtext/germap/. Accessed 04 Jan 2017.
Gerber JS, Newland JG, Coffin SE, Hall M, Thurm C, Prasad PA, et al. Variability in antibiotic use at children’s hospitals. Pediatrics. 2010;126:1067–73. doi:10.1542/peds.2010-1275.
Bolon MK, Arnold AD, Feldman HA, Rehkopf DH, Strong EF, Goldmann DA, et al. Evaluating vancomycin use at a pediatric hospital: new approaches and insights. Infect Control Hosp Epidemiol. 2005;26:47–55. doi:10.1086/502486.
Levy ER, Swami S, Dubois SG, Wendt R, Banerjee R. Rates and appropriateness of antimicrobial prescribing at an academic children’s hospital, 2007–2010. Infect Control Hosp Epidemiol. 2012;33:346–53. doi:10.1086/664761.
Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62:e51–77. doi:10.1093/cid/ciw118.
de With K, Allerberger F, Amann S, Apfalter P, Brodt HR, Eckmanns T, et al. Strategies to enhance rational use of antibiotics in hospital: a guideline by the German Society for Infectious Diseases. Infection. 2016;44:395–439. doi:10.1007/s15010-016-0885-z.
World Health Organization, WHO. Global Action Plan on Antimicrobial Resistance. 2015. http://www.wpro.who.int/entity/drug_resistance/resources/global_action_plan_eng.pdf. Accessed 04 Jan 2017.
Schmitt S, McQuillen DP, Nahass R, Martinelli L, Rubin M, Schwebke K, et al. Infectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin Infect Dis. 2014;58:22–8. doi:10.1093/cid/cit610.
Dancer SJ, Kirkpatrick P, Corcoran DS, Christison F, Farmer D, Robertson C. Approaching zero: temporal effects of a restrictive antibiotic policy on hospital-acquired Clostridium difficile, extended-spectrum beta-lactamase-producing coliforms and meticillin-resistant Staphylococcus aureus. Int J Antimicrob Agents. 2013;41:137–42. doi:10.1016/j.ijantimicag.2012.10.013.
McCulloh RJ, Queen MA, Lee B, Yu D, Stach L, Goldman J, et al. Clinical impact of an antimicrobial stewardship program on pediatric hospitalist practice, a 5-year retrospective analysis. Hosp Pediatr. 2015;5:520–7. doi:10.1542/hpeds.2014-0250.
Newland JG, Stach LM, De Lurgio SA, Hedican E, Yu D, Herigon JC, et al. Impact of a prospective-audit-with-feedback antimicrobial stewardship program at a children’s hospital. J Pediatr Infect Dis Soc. 2012;1:179–86. doi:10.1093/jpids/pis054.
Newman RE, Hedican EB, Herigon JC, Williams DD, Williams AR, Newland JG. Impact of a guideline on management of children hospitalized with community-acquired pneumonia. Pediatrics. 2012;129:e597–604. doi:10.1542/peds.2011-1533.
Lee KR, Bagga B, Arnold SR. Reduction of Broad-Spectrum Antimicrobial Use in a Tertiary Children’s Hospital Post Antimicrobial Stewardship Program Guideline Implementation. Pediatr Crit Care Med. 2016;17:187–93. doi:10.1097/PCC.0000000000000615.
Hersh AL, De Lurgio SA, Thurm C, Lee BR, Weissman SJ, Courter JD, et al. Antimicrobial stewardship programs in freestanding children’s hospitals. Pediatrics. 2015;135:33–9. doi:10.1542/peds.2014-2579.
Di Pentima MC, Chan S, Hossain J. Benefits of a pediatric antimicrobial stewardship program at a children’s hospital. Pediatrics. 2011;128:1062–70. doi:10.1542/peds.2010-3589.
Di Pentima MC, Chan S, Eppes SC, Klein JD. Antimicrobial prescription errors in hospitalized children: role of antimicrobial stewardship program in detection and intervention. Clin Pediatr (Phila). 2009;48:505–12. doi:10.1177/0009922808330774.
Nguyen-Ha PT, Howrie D, Crowley K, Vetterly CG, McGhee W, Berry D, et al. A quality assessment of a collaborative model of a pediatric antimicrobial stewardship program. Pediatrics. 2016;137:e20150316. doi:10.1542/peds.2015-0316.
Versporten A, Bielicki J, Drapier N, Sharland M, Goossens H, Group Ap. The Worldwide Antibiotic Resistance and Prescribing in European Children (ARPEC) point prevalence survey: developing hospital-quality indicators of antibiotic prescribing for children. J Antimicrob Chemother. 2016;71:1106–17. doi:10.1093/jac/dkv418.
Versporten A, Sharland M, Bielicki J, Drapier N, Vankerckhoven V, Goossens H, et al. The antibiotic resistance and prescribing in European Children project: a neonatal and pediatric antimicrobial web-based point prevalence survey in 73 hospitals worldwide. Pediatr Infect Dis J. 2013;32:e242–53. doi:10.1097/INF.0b013e318286c612.
Huebner J, Rack-Hoch AL, Pecar A, Schmid I, Klein C, Borde JP. Pilot project of a pediatric antibiotic stewardship initiative at the Hauner children’s hospital. Klin Padiatr. 2013;225:223–9. doi:10.1055/s-0033-1349063.
Polk RE, Hohmann SF, Medvedev S, Ibrahim O. Benchmarking risk-adjusted adult antibacterial drug use in 70 US academic medical center hospitals. Clin Infect Dis. 2011;53:1100–10. doi:10.1093/cid/cir672.
Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53:e25–76. doi:10.1093/cid/cir531.
Pakyz AL, Gurgle HE, Ibrahim OM, Oinonen MJ, Polk RE. Trends in antibacterial use in hospitalized pediatric patients in United States academic health centers. Infect Control Hosp Epidemiol. 2009;30:600–3. doi:10.1086/597545.
Agwu AL, Lee CK, Jain SK, Murray KL, Topolski J, Miller RE, et al. A World Wide Web-based antimicrobial stewardship program improves efficiency, communication, and user satisfaction and reduces cost in a tertiary care pediatric medical center. Clin Infect Dis. 2008;47:747–53. doi:10.1086/591133.
Metjian TA, Prasad PA, Kogon A, Coffin SE, Zaoutis TE. Evaluation of an antimicrobial stewardship program at a pediatric teaching hospital. Pediatr Infect Dis J. 2008;27:106–11. doi:10.1097/INF.0b013e318158603a.
Smith MJ, Gerber JS, Hersh AL. Inpatient antimicrobial stewardship in pediatrics: a systematic review. J Pediatr Infect Dis Soc. 2015;4:e127–35. doi:10.1093/jpids/piu141.
Newland JG, Banerjee R, Gerber JS, Hersh AL, Steinke L, Weissman SJ. Antimicrobial stewardship in pediatric care: strategies and future directions. Pharmacotherapy. 2012;32:735–43. doi:10.1002/j.1875-9114.2012.01155.x.
Goff DA, Bauer KA, Reed EE, Stevenson KB, Taylor JJ, West JE. Is the “low-hanging fruit” worth picking for antimicrobial stewardship programs? Clin Infect Dis. 2012;55:587–92. doi:10.1093/cid/cis494.
McKinnell JA, Kunz DF, Moser SA, Vangala S, Tseng CH, Shapiro M, et al. Patient-level analysis of incident vancomycin-resistant enterococci colonization and antibiotic days of therapy. Epidemiol Infect. 2016;144:1748–55. doi:10.1017/S0950268815003118.
Feazel LM, Malhotra A, Perencevich EN, Kaboli P, Diekema DJ, Schweizer ML. Effect of antibiotic stewardship programmes on Clostridium difficile incidence: a systematic review and meta-analysis. J Antimicrob Chemother. 2014;69:1748–54. doi:10.1093/jac/dku046.
Borde JP, Litterst S, Ruhnke M, Feik R, Hubner J, deWith K, et al. Implementing an intensified antibiotic stewardship programme targeting cephalosporin and fluoroquinolone use in a 200-bed community hospital in Germany. Infection. 2015;43:45–50. doi:10.1007/s15010-014-0693-2.
Upperman JS, Staley P, Friend K, Neches W, Kazimer D, Benes J, et al. The impact of hospitalwide computerized physician order entry on medical errors in a pediatric hospital. J Pediatr Surg. 2005;40:57–9. doi:10.1016/j.jpedsurg.2004.09.024.
Engum SA, Breckler FD. An evaluation of medication errors-the pediatric surgical service experience. J Pediatr Surg. 2008;43:348–52. doi:10.1016/j.jpedsurg.2007.10.042.
Lesar TS. Errors in the use of medication dosage equations. Arch Pediatr Adolesc Med. 1998;152:340–4.
Ekins-Daukes S, McLay JS, Taylor MW, Simpson CR, Helms PJ. Antibiotic prescribing for children. Too much and too little? Retrospective observational study in primary care. Br J Clin Pharmacol. 2003;56:92–5.
Guillemot D, Carbon C, Balkau B, Geslin P, Lecoeur H, Vauzelle-Kervroedan F, et al. Low dosage and long treatment duration of beta-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365–70.
Schrag SJ, Pena C, Fernandez J, Sanchez J, Gomez V, Perez E, et al. Effect of short-course, high-dose amoxicillin therapy on resistant pneumococcal carriage: a randomized trial. JAMA. 2001;286:49–56.
Aseeri MA. The impact of a pediatric antibiotic standard dosing table on dosing errors. J Pediatr Pharmacol Ther. 2013;18:220–6. doi:10.5863/1551-6776-18.3.220.
Ambroggio L, Thomson J, Murtagh Kurowski E, Courter J, Statile A, Graham C, et al. Quality improvement methods increase appropriate antibiotic prescribing for childhood pneumonia. Pediatrics. 2013;131:e1623–31. doi:10.1542/peds.2012-2635.
Smith MJ, Kong M, Cambon A, Woods CR. Effectiveness of antimicrobial guidelines for community-acquired pneumonia in children. Pediatrics. 2012;129:e1326–33. doi:10.1542/peds.2011-2412.
Davey P, Brown E, Charani E, Fenelon L, Gould IM, Holmes A, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2013;4:CD003543. doi:10.1002/14651858.CD003543.pub3.
Standiford HC, Chan S, Tripoli M, Weekes E, Forrest GN. Antimicrobial stewardship at a large tertiary care academic medical center: cost analysis before, during, and after a 7-year program. Infect Control Hosp Epidemiol. 2012;33:338–45. doi:10.1086/664909.
Acknowledgements
This work was supported by AOK Bayern and the interprofessional PhD-program Clinical Pharmacy, LMU Munich.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kreitmeyr, K., von Both, U., Pecar, A. et al. Pediatric antibiotic stewardship: successful interventions to reduce broad-spectrum antibiotic use on general pediatric wards. Infection 45, 493–504 (2017). https://doi.org/10.1007/s15010-017-1009-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1009-0