Abstract
Purpose
We aimed to investigate clinical features of patients with descending necrotizing mediastinitis (DNM) in order to improve management and outcome.
Methods
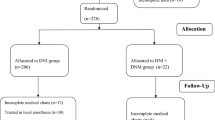
We prospectively examined all patients with DNM admitted to the Intensive Care Unit (ICU) during the period from April 2007 to December 2013. Demographics, clinical features, microbiology, medical and surgical treatment data were recorded. Survivor and nonsurvivor groups were analyzed to identify factors associated with mortality.
Results
Overall, 34 patients with DNM have been included. The mean age was 46.8 ± 11.2 years (range 24–70). The male/female ratio was 3.25. DNM arose from odontogenic infection in 22 (65 %) patients; from peritonsillar abscess in 9 (26 %) patients and from paranasal sinus in 3 (9 %) patients. Microbiological cultures revealed a high percentage of aerobic/anaerobic coinfection. Nonsurvivors were statistically more likely to have higher SAPS II score (mean difference 19.1, 95 % CI 12.3–25.9 P < 0.01) and more severe disease (P < 0.01) than survivors. Positive correlation was found between time to ICU admission after head or neck infection diagnosis and SAPS II score (ρ = 0.5, P = 0.03). The same was true for ICU length of stay and time to ICU admission (ρ = 0.6, P < 0.01) and time to surgery (ρ = 0.5, P = 0.03). Surgical treatments consisted in: transcervical drainage in 14 cases, (42 %); irrigation through subxiphoid and cervical incisions of the anterior mediastinum with additional percutaneous thoracic drainage when necessary in ten cases, (29 %); thoracotomy with radical mediastinal surgical debridement, excision of necrotic tissue and decortication in ten cases, (29 %). We have found a mortality rate of 12 %. Patients with DNM type IIB were admitted to the ICU later than patients with DNM type I and type IIA (mean difference 3.2 days, 95 % CI 1.2–5.1, P 0.02).
Conclusions
Prompt ICU admission in order to manage severe sepsis and/or septic shock, along with early and aggressive surgery and adequate antimicrobial therapy, could be key factors in reducing DNM mortality.
Similar content being viewed by others
Introduction
Necrotizing fasciitis (NF) are life-threatening infections involving fascia and subcutaneous tissues, with concomitant thrombosis of cutaneous microcirculation [1, 2]. The affected area is initially characterized by swelling, erythema and pain; edema outside the area of compromised skin, pain out of proportion to appearance, skin discoloration, vesicles, bullae, necrosis and crepitus and/or subcutaneous gas may be seen with disease progression [3]. “Descending necrotizing fasciitis” or “descending necrotizing mediastinitis” (DNM) is a rare disease secondary to pharyngeal and odontogenic infection [4]. Before wide antibiotic availability, DNM accounted for 10–31 % of mediastinitis cases [5]. The term DNM was first used in 1938 by Pearse [4] to describe an infectious disease starting from a dental or oropharyngeal focus which then spreads to potential fascial planes of the lower part of the face and upper part of the neck and extends downward into the mediastinum [6]. Odontogenic infections involving the second or third mandibular molar can spread to sublingual and submandibular spaces. From these spaces the infection can extend to lateral pharyngeal space to involve the retropharyngeal space and track into the anterior mediastinum or, if the danger space is affected, to the posterior mediastinum [7–9]. The “danger space” starts from C6 level of the spine where begins the retropharyngeal pathway and continues as far as the T1 level. This name is given because this space is patent from the skull base to the diaphragm, thereby allowing the spread of infection to the mediastinum. When infection reaches this level, the prognosis is usually poor.
In addition to odontogenic infection, mediastinitis can arise from other source of infection such as tonsils [10], parotid glands [11] or, rarely, otitis, mastoiditis and epiglottitis [5]. Optimal management of this potentially deadly infection requires a high index of suspicion and early diagnosis, immediate resuscitation and aggressive surgical debridement. We had the unusual opportunity to deal with a good number of patients admitted to the Intensive Care Unit (ICU) because of DNM during the second and third quarter of 2007, so we decided to collect DNM cases prospectively from April 2007. We stopped our data collection in December 2013. To our knowledge such a large case series has never been published before and this is why we believe it could be of great interest for clinical practice.
Patients and methods
Study design, patients and definitions
Medical data of all patients with DNM admitted to the ICU of Civico-Di Cristina-Benfratelli Hospital during the period from April 2007 to December 2013 were prospectively collected. DNM diagnosis was made on the basis of criteria defined by Estrera and colleagues [7] in 1983. Criteria include:
-
1.
Clinical evidence of severe oropharyngeal infection;
-
2.
radiographic characteristics of mediastinitis;
-
3.
intraoperative or post-mortem documentation of necrotizing mediastinal infection;
-
4.
establishment of the relationship of the oropharyngeal infection with the development of the mediastinal process.
The extent of dissemination of infection into the mediastinum was evaluated using CT scans and mediastinitis was classified according to Endo’s criteria in type I (focal) mediastinitis (infection located in the superior mediastinal space, above tracheal bifurcation) and type II (diffuse) mediastinitis; type II mediastinitis was in turn subdivided into two subtypes: subtype IIA (infection still located in the anterior inferior mediastinal space) and subtype IIB (infection process has reached posterior inferior mediastinum) [12]. Follow-up CT scans were also performed to establish the surgical management and to assess the adequacy of therapy.
Data extracted from medical charts included demographics (age, sex), predisposing conditions (diabetes mellitus, high blood pressure, cigarette smoking), source of infection (teeth, tonsils, paranasal sinuses), microbiological isolation, outpatient antibiotic treatment, time (days) to ICU admission after diagnosis of head or neck infection, SAPS II score at the time of ICU admission, time (hours) to mediastinal drainage after the diagnosis of mediastinitis, type of surgery, duration of mediastinal drainage, inpatient antibiotic treatment regimen and duration (days), ICU length of stay (days) and outcome. Number of patients who underwent tracheostomy was also reported.
Statistical analysis
All data were statistically analyzed using a commercially available statistical software package (SPSS, version 20.0; SPSS Inc., Chicago, Illinois). Continuous variables were compared using Student’s t test for independent samples. Categorical variables were evaluated using the χ 2 test or Fisher exact test, when appropriate, and Pearson product-moment correlation coefficient. All tests were 2-tailed and a P value <0.05 was considered statistically significant. Results were expressed as mean ± standard deviation (SD) for continuous normally distributed variables or as percentage for categorical variables. Multivariate analysis was used to identify independent predictors of ICU mortality. We used binary logistic regression, incorporating all variables found to be significant at univariate analysis with a stepwise method.
Results
Overall, 34 patients fulfilled criteria for DNM and were included in the final analysis. Most common physical findings on admission were tenderness beyond the apparent margins of infection, erythema, warmth of the skin to palpation and cervical subcutaneous crackling, indicating the presence of gas in subcutaneous tissues. Types of DNM occurred in our patients and classified based on Endo’s criteria [12] are reported in Table 1. Main clinical features of patients included in the study are shown in Table 2; an example of the typical computed tomography (CT) scan findings is shown in Fig. 1. The mean age was 46.8 ± 11.2 years (range 24–70). DNM was more frequent in males (26 patients, 77 %) than females (eight patients, 24 %). Ten (29 %) patients had diabetes mellitus type 2, 8 (24 %) patients were current cigarette smokers and 6 (18 %) patients had high blood pressure; ten (29 %) patients had no obvious risk factors. DNM arose from odontogenic infection in 22 (65 %) patients; source of infection was peritonsillar abscess in 9 (26 %) patients and paranasal sinus in 3 (9 %) patients. As shown in Table 3, Microbiological cultures were obtained from 24 (71 %) patients. Viridans streptococci (S. constellatus, S. sanguis, S. mitis) were isolated in 7 (29 %) cases, Prevotella spp. in 5 (21 %), K. pneumoniae in 4 (17 %) and Peptostreptococcus spp. in 3 (12 %). Cultures collected from 8 (33 %) patients yielded S. aureus. No bacteria were isolated from cultures obtained from four patients and a coinfection (aerobic/anaerobic bacteria) was present in 12 cases. All patients were given empirical antibiotic treatment with a beta-lactam (62 %) or a macrolide (23 %) or a fluoroquinolone (15 %) before hospital admission. Time to ICU admission after diagnosis of head or neck infection was 9.5 ± 2.9 days. Mean SAPS II score at the time of ICU admission was 31.2 ± 8.8 with a predicted mortality rate of 12 %. Twenty-nine (85 %) patients had a tracheostomy performed. Average time to mediastinal drainage after the diagnosis of mediastinitis was 11.2 ± 11.2 h and all patients sustained emergency surgical procedures after the diagnosis of DNM was confirmed. Surgical treatments consisted in extensive debridement of all ischemic appearing and grossly necrotic soft tissues and included:
Axial thorax CT scans of a 20 years old female who presented with an anterior mediastinitis developing as a complication of an odontogenic infection at hospital admission (a) and after 72 h at ICU admission (b). a Shows air and fluid in the anterior mediastinum and lung parenchymal consolidation in the right lung. b Shows further progression of the infection despite initial medical therapy with antibiotics and steroids with bilateral air spaces opacities, bilateral pneumothorax with pleural effusion, pneumo-mediastinum and mediastinal enlargement requiring surgical therapy
-
1.
transcervical drainage in DNM type I (14 cases, 42 %);
-
2.
irrigation through subxiphoid and cervical incisions of the anterior mediastinum with additional percutaneous thoracic drainage when necessary in DNM type IIA (ten cases, 29 %);
-
3.
thoracotomy with radical mediastinal surgical debridement, excision of necrotic tissue and decortication in DNM type IIB (ten cases, 29 %).
Post-operative mediastinopleural irrigation with saline, when required, was performed once or twice a day until cultures of pleural effusion became negative. Ten (29 %) patients received additional surgical procedures to prevent the spread of infection to subcutaneous thoracic tissues (six cases, 18 %) and to the muscles of the nuchal region (four cases, 12 %). On average, two surgical debridements were performed within the first 5 days and the mean time to wound healing was 14 days after initial surgery. Mediastinal drainage was left in place for an average time of 10.2 ± 3.8 days (range 4–20 days). All patients underwent intravenous empirical antimicrobial chemotherapy with piperacillin-tazobactam (4.5 g q6 h) and daptomycin (8 mg/kg qd) as soon as the diagnosis of DNM was made. Daptomycin was de-escalated if cultures were negative for S. aureus growth. The mean duration of empirical antibiotic regimen was 12.9 ± 4.8 days. Mean ICU length of stay was 13.9 ± 3.7. All patients suffered severe sepsis and 4 (12 %) of them with septic shock eventually died. Survivors were transferred to a medical or surgical ward with an average post ICU length of stay of 10.8 ± 5.4 days. As shown in Table 4, at univariate analysis, variables significantly associated with increased ICU mortality were advanced age (mean difference 16.9 years, 95 % CI 6.2–27.7, P < 0.01) and longer ICU length of stay (mean difference 6 days, 95 % CI 2.5–9.5, P < 0.01). Nonsurvivors were statistically more likely to have higher SAPS II score at ICU admission (mean difference 19.1, 95 % CI 12.3–25.9 P < 0.01) and more severe disease as assessed by Endo’s criteria (P = 0.04) than survivors. Positive moderate linear correlation was found between time to ICU admission after head or neck infection diagnosis and SAPS II score (ρ = 0.5, P = 0.03). The same was true for ICU length of stay and time to ICU admission after head or neck infection diagnosis (ρ = 0.6, P < 0.01) and time to mediastinal drainage (ρ = 0.5, P = 0.03). Patients with DNM type IIB were admitted to the ICU later than patients with DNM type I and type IIA and the difference was statistically significant (mean difference 3.2 days, 95 % CI 1.2–5.1, P = 0.02). Moreover DNM type IIB was associated with longer time to mediastinal drainage than DMN type I and type IIA (mean difference 11 h, 95 % CI 3.1–18.9, P < 0.01). No statistically significant associations were found between microbiological isolates and other variables. Significant variables at univariate analysis were included in the binary logistic regression model, but none of the covariates proved to be statistically significant.
Discussion
Broad case series and meta-analysis regarding DNM have already been published [13–17]. To our knowledge this is the largest prospective study about DNM ever reported in the literature. For the first time clinical characteristics and risk factors associated with DNM mortality have been systematically and statistically examined. According to a small Italian case series and literature review published by Pellis and colleagues in 2001 [18], we confirm that DNM most frequently arises from odontogenic infections (65 %). The finding of dental infections as main cause of DNM in our case series could be explained by the fact that our institution serves a low-income community with inadequate access to dental cures. However, nowadays, with better oral hygiene, growing access to appropriate dental treatments and wide availability of antibiotics, the common cause of DNM should have shifted from odontogenic infection to oropharyngeal conditions (82.3 %), as described by Kocher et al. [6]. Even though typical risk factors have not been identified, some conditions appear to be more commonly associated with DNM such as intravenous drug use, alcoholism and chronic debilitating comorbidities (obesity, diabetes mellitus and immune suppression) [19, 20]. Seventy percent of our patients had predisposing conditions, including cigarette smoking and high blood pressure. Thirty percent had no apparent risk factors and this is in line with other reports [21]. It has been suggested that necrotizing cellulitis is due to a symbiosis between aerobic and anaerobic bacteria [22] and this synergistic effect is of great importance in order to propagate the infectious process toward these spaces [23]. Our result of mixed (aerobic/anaerobic) microbiological cultures obtained in 12 (50 %) out of 24 cases is consistent with these classical observations.
There are three possible remarkable findings from this study. First, we have found a mortality rate of 11.8 % and these data confirm previous observations of DNM-related mortality ranging from 11 to 35 % [17]. The relatively low death rate of our case series could be attributable to early diagnosis, rapid initiation of appropriate and fast medical treatment after onset of sepsis, severe sepsis or septic shock, and timely aggressive surgical treatment. The most important tool for early diagnosis is a high index of suspicion. Clinical signs and symptoms, although nonspecific, can help in making the diagnosis and could be local or systemic. The former consists in swelling, erythema and pain and, with disease progression, edema outside the area of compromised skin, pain out of proportion to appearance, skin discoloration, vesicles, bullae, necrosis and crepitus and/or subcutaneous gas [3]. The latter includes fever, tachycardia, hypotension and shock [3]. Makeieff and colleagues [21] have suggested a link between delayed diagnosis and previous exposure to glucocorticoids that could act by blunting severity of symptoms. It is not known whether any of our patients have been exposed to glucocorticoids, but time to ICU admission after diagnosis of head or neck infection in our study (9.5 ± 2.9 days) was very similar to that reported by Makeieff and colleagues (mean time 7 days) [21]. In addition to Estera et al. [7], other authors have worked on intraoperative criteria for diagnosis of DNM: intraoperative macroscopic findings consisting with DNM include gray necrotic tissue, lack of bleeding, thrombosed vessels, foul smelling pus, noncontracting muscle, and a positive “finger test” result, which is characterized by lack of resistance to finger dissection in normally adherent tissues. [24–26]. Delay in diagnosis and late or inappropriate drainage of the mediastinum are well-known risk factors for high mortality [27]. Surgical debridement is a mandatory life-saving approach to patients with DNM and should be performed as soon as possible. Wong et al. [28] reported a ninefold increase in mortality if surgery is delayed more than 24 h after ICU admission. Other authors reported increased mortality in patients who underwent incomplete debridement [29]. In our study, both higher SAPS II score and DNM type IIB were variables significantly associated with greater ICU mortality (P < 0.01 and P = 0.04, respectively). A significant linear correlation (ρ = 0.5, P = 0.03) between time to ICU admission and SAPS II score has been found. Moreover more severe disease (DNM type IIB versus DNM type I and type IIA) was statistically more likely in patients with longer time to ICU admission (mean difference 3.2 days, 95 % CI 1.2–5.1, P = 0.02) and longer time to mediastinal drainage after ICU admission (mean difference 11 h, 95 % CI 3.1–18.9, P < 0.01). These data demonstrate that prompt and appropriate medical treatment and early surgical treatment are of uttermost importance in reducing mortality in patients with DNM. Failure to perform early surgery or incomplete surgical drainage with ongoing mediastinal involvement is an indication for major thoracic surgery with no delay, before the onset of fatal events such as vessel erosion, hemorrhage and cardiac or respiratory complications [21].
The role of tracheostomy in DNM is controversial. Several authors [30] speculated that tracheostomy sites are sources of downward spread and subsequent mediastinal infection. We do believe that tracheostomy is an essential part in the management of severe DNM. It should be performed early because edema of upper airway can be life-threatening [18]. We performed a median surgical tracheostomy in 29 (85 %) out of 34 patients and no post-operative complications such as contamination or infection of the tracheostomy site from the nearby cervical wounds occurred. Moreover tracheostomy offers some advantages, namely, simplification of bedside procedures, faster ventilator weaning process and shorter ICU length of stay and it may help in reducing need for sedation and unnecessary resource utilization [31, 32].
Second, the most frequently isolated organisms in DNM include viridans group streptococci, S. aureus, peptostreptococci, Bacteroides spp., Prevotella spp. and Fusobacterium [5]. Reported relative frequencies of these organisms vary because appropriate techniques for anaerobic specimen transport and culture might not be routinely used [33]. Streptococcus species are commonly recognized as predominant etiological agents [6], but in our case series methicillin-sensitive S. aureus was the most frequently encountered microorganism with a relative proportion of 33 % of isolates. This result is comparable with bacteriology of DNM highlighted by Suehara and colleagues in a retrospective analysis of 80 cases of DNM [16]. As shown in Table 3, S. aureus was always isolated in mixed cultures with anaerobes belonging to the genera Peptostreptococcus, Bacteroides and Prevotella. Interestingly, synergistic enhancement of virulence of S. aureus in combination with the aforementioned genera is a well-known phenomenon [34].
Third, in light of what we have found about microbiology of our cases of DNM, an empirical approach with daptomycin and piperacillin-tazobactam has been used after diagnosis of DNM with de-escalation of daptomycin if no growth of S. aureus occured. Daptomycin is an effective agent against methicillin-susceptible and -resistant S. aureus (MSSA and MRSA, respectively) [35] but it is untrustworthy against Streptococcus species because of erratic MICs displayed by viridans group streptococci, particularly S. anginosus and S. oralis [36]. These in vitro results correspond clinically to a report of S. anginosus breakthrough bacteremia in a patient treated with daptomycin for a MRSA bacteremia and osteomyelitis [37] and to the observation by Tascini et al. of treatment failure in a case of mitro-aortic native-valve S. oralis endocarditis [38]. Enhanced antistaphylococcal activity of beta-lactam plus daptomycin versus MRSA has been described [39]. We could speculate that a similar synergistic effect against both MSSA and MRSA might be achieved by using daptomycin plus beta-lactam/beta-lactamase inhibitor combinations and this could explain the favorable prognosis of our patients who were all exposed to such a combination. Additionally, daptomycin reduces macrophage inflammatory response to S. aureus by diminishing release of proinflammatory bacterial components [40]. We used a daptomycin dosage of 8 mg/kg/day, as suggested by current recommendations in cases of severe staphylococcal infections [41, 42]; the need of higher daptomycin dosages has been demonstrated in patients with MRSA infection and severe sepsis or septic shock [43, 44], to achieve adequate serum levels and avoid underexposure of drug [42–44]. Of importance the use of a fixed initial dose of daptomycin of 750 mg/day has been associated with optimal activity and minimization of risk of muscular toxicity [43]. We have to outline that in the present study no patients experienced increase of creatine phosphokinase necessitating withdrawn of the drug. Despite all these considerations, we recommend to spare daptomycin if no clinical isolation of S. aureus is yielded.
Our work has several limitations. Even though it exhibits the largest prospective DNM case series ever published in the literature, this case series still remains a small one. Moreover, this study is uncontrolled and nonrandomized.
In conclusion, DNM is a life-threatening disease burdened by great mortality. Prompt admission to the ICU in order to manage severe sepsis and/or septic shock, in combination with early and aggressive surgery, could be key factors in reducing such a high mortality rate.
References
Mathieu D, Neviere R, Teillon C, Chagnon JL, Lebleu N, Wattel F. Cervical necrotizing fasciitis: clinical manifestations and management. Clin Infect Dis. 1995;21:51–6.
Sudarsky LA, Laschinger JC, Coppa GF, Spencer FC. Improved results from a standardized approach in treating patients with necrotizing fasciitis. Ann Surg. 1987;206:661–5.
Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis. 2007;44:705–10.
Pearse HE. Mediastinitis following cervical suppuration. Ann Surg. 1938;108:588–611.
Mandell GL, Bennet JE, Dolin R. Mandell, Douglas, and Bennett’s principles and practise of infectious diseases. 7th ed. Philadelphia: Churchill Livingstone Elsevier; 2007.
Kocher GJ, Hoksch B, Caversaccio M, Wiegand J, Schmid RA. Diffuse descending necrotizing mediastinitis: surgical therapy and outcome in a single-centre series. Eur J Cardiothorac Surg. 2012;42:e66–72. doi:10.1093/ejcts/ezs385.
Estrera AS, Landay MJ, Grisham JM, Sinn DP, Platt MR. Descending necrotizing mediastinitis. Surg Gynecol Obstet. 1983;157:545–52.
Levine TM, Wurster CF, Krespi YP. Mediastinitis occurring as a complication of odontogenic infections. Laryngoscope. 1986;96:747–50.
Jaworsky D, Reynolds S, Chow AW. Extracranial head and neck infections. Crit Care Clin. 2013;29:443–63. doi:10.1016/j.ccc.2013.03.003.
Roccia F, Pecorari GC, Oliaro A, et al. Ten years of descending necrotizing mediastinitis: management of 23 cases. J Oral Maxillofac Surg. 2007;65:1716–24.
Guardia SN, Cameron R, Phillips A. Fatal necrotizing mediastinitis secondary to acute suppurative parotitis. J Otolaryngol. 1991;20:54–6.
Endo S, Murayama F, Hasegawa T, et al. Guideline of surgical management based on diffusion of descending necrotizing mediastinitis. Jpn J Thorac Cardiovasc Surg. 1999;47:14–9.
Wheatley MJ, Stirling MC, Kirsh MM, Gago O, Orringer MB. Descending necrotizing mediastinitis: transcervical drainage is not enough. Ann Thorac Surg. 1990;49:780–4.
Kiernan PD, Hernandez A, Byrne WD, et al. Descending cervical mediastinitis. Ann Thorac Surg. 1998;65:1483–8.
Scaglione M, Pinto A, Romano S, Giovine S, Sparano A, Romano L. Determining optimum management of descending necrotizing mediastinitis with CT; experience with 32 cases. Emerg Radiol. 2005;11:275–80.
Suehara AB, Gonçalves AJ, Alcadipani FA, Kavabata NK, Menezes MB. Deep neck infection: analysis of 80 cases. Braz J Otorhinolaryngol. 2008;74:253–9.
Ridder GJ, Maier W, Kinzer S, Teszler CB, Boedeker CC, Pfeiffer J. Descending necrotizing mediastinitis: contemporary trends in etiology, diagnosis, management, and outcome. Ann Surg. 2010;251:528–34. doi:10.1097/SLA.0b013e3181c1b0d1.
Pellis T, Berlot G, Giacomarra V, Bregant M. Descending necrotizing mediastinitis. Clinical experience and review of the literature. Minerva Anestesiol. 2001;67:731–6.
Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC (laboratory risk indicator for necrotizing fasciitis) score: a tool for distinguishing necrotize fasciitis from other soft tissue infections. Crit Care Med. 2004;32:1535–41.
Childers BJ, Potyondy LD, Nachreiner R, et al. Necrotizing fasciitis: a fourteen year retrospective study of 163 consecutive patients. Am Surg. 2002;68:109–16.
Makeieff M, Gresillon N, Berthet JP, et al. Management of descending necrotizing mediastinitis. Laryngoscope. 2004;114:772–5.
Stone HH, Martin JD Jr. Synergistic necrotizing cellulitis. Ann Surg. 1972;175:702–11.
Moncada R, Warpeha R, Pickleman J, et al. Mediastinitis from odontogenic and deep cervical infection. Anatomic pathways of propagation. Chest. 1978;73:497–500.
Wong CH, Wang YS. The diagnosis of necrotizing fasciitis. Curr Opin Infect Dis. 2005;18:101–6.
Cainzos M, Gonzalez-Rodriguez J. Necrotizing soft tissue infections. Curr Opin Crit Care. 2007;13:433–9.
Goldstein EJC, Anaya DA, Patchen Dellinger E. Necrotizing soft tissue infection: diagnosis and management. Clin Infect Dis. 2007;44:705–10.
Lavini C, Natali P, Morandi U, Dallari S, Bergamini G. Descending necrotizing mediastinitis. Diagnosis and surgical treatment. J Cardiovasc Surg. 2003;44:655–60.
Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. Necrotizing fascitiis: clinical presentation, microbiology and determinants of mortality. J Bone Joint Surg Am. 2003;85:1454–60.
Bilton BD, Zibari GB, Mc Millan RW, Aultman DF, Dunn G, McDonald JC. Aggressive surgical management of necrotizing fascitiis serves to decrease mortality: a retrospective study. Am Surg. 1998;64:397–400.
Mitjans MS, Sanchís JB, Padro XB, García I, Garolera JM, Garay MR. Descending necrotizing mediastinitis. Int Surg. 2000;85:331–5.
Arabi Y, Haddad S, Shirawi N, Al Shimemeri A. Early tracheostomy in intensive care trauma patients improves resource utilization: a cohort study and literature review. Crit Care. 2004;8:R347–52.
Pierson DJ. Tracheostomy and weaning. Respir Care. 2005;50:526–33.
Murray PM, Finegold SM. Anaerobic mediastinitis. Rev Infect Dis. 1984;6:S123–7.
Brook I. The role of encapsulated anaerobic bacteria in synergistic infections. FEMS Microbiol Rev. 1994;13:65–74.
LaPlante KL, Rybak MJ. Impact of high-inoculum Staphylococcus aureus on the activities of nafcillin, vancomycin, linezolid, and daptomycin, alone and in combination with gentamicin, in an in vitro pharmacodynamic model. Antimicrob Agents Chemother. 2004;48:4665–72.
Sader HS, Flamm RK, Farrell DJ, Jones RN. Daptomycin activity against uncommonly isolated streptococcal and other gram-positive species groups. Antimicrob Agents Chemother. 2013;57:6378–80. doi:10.1128/AAC.01906-13.
Palacio F, Lewis JS 2nd, Sadkowski L, Echevarria K, Jorgensen JH. Breakthrough bacteremia and septic shock due to Streptococcus anginosus resistant to daptomycin in a patient receiving daptomycin therapy. Antimicrob Agents Chemother. 2011;55:3639–40. doi:10.1128/AAC.00231-11.
Tascini C, Di Paolo A, Poletti R, et al. Daptomycin concentrations in valve tissue and vegetation in patients with bacterial endocarditis. Antimicrob Agents Chemother. 2013;57:601–2. doi:10.1128/AAC.01608-12.
Dhand A, Bayer AS, Pogliano J, et al. Use of antistaphylococcal beta-lactams to increase daptomycin activity in eradicating persistent bacteremia due to methicillin-resistant Staphylococcus aureus: role of enhanced daptomycin binding. Clin Infect Dis. 2011;53:158–63. doi:10.1093/cid/cir340.
English BK, Maryniw EM, Talati AJ. Diminished macrophage inflammatory response to Staphylococcus aureus isolates exposed to daptomycin versus vancomycin or oxacillin. Antimicrob Agents Chemother. 2006;50:2225–7.
Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285–92.
Falcone M, Russo A, Venditti M. Optimizing antibiotic therapy of bacteremia and endocarditis due to staphylococci and enterococci: new insights and evidence from the literature. J Infect Chemother. 2015;21:330–9.
Falcone M, Russo A, Venditti M, Novelli A, Pai MP. Considerations for higher doses of daptomycin in critically ill patients with methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2013;57:1568–76.
Falcone M, Russo A, Cassetta MI, et al. Variability of pharmacokinetic parameters in patients receiving different dosages of daptomycin: is therapeutic drug monitoring necessary? J Infect Chemother. 2013;19:732–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare they have no conflict of interests.
Ethical standards
Informed consent from all patients or a patient’s next of kin was obtained and the study has been approved by the appropriate ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Rights and permissions
About this article
Cite this article
Palma, D.M., Giuliano, S., Cracchiolo, A.N. et al. Clinical features and outcome of patients with descending necrotizing mediastinitis: prospective analysis of 34 cases. Infection 44, 77–84 (2016). https://doi.org/10.1007/s15010-015-0838-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-015-0838-y