Abstract
Background
Strongyloides stercoralis may lead to overwhelming infestation [Strongyloides hyperinfection syndrome (SHS)]. We aimed at describing a case series of patients admitted in intensive care unit (ICU) with SHS and report a literature review of such cases.
Patients and methods
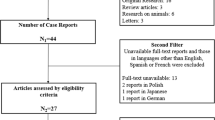
Retrospective multicenter study of 11 patients admitted to the ICU of tertiary hospitals with SHS between 2000 and 2013. Literature review with Pubmed retrieved 122 cases. Logistic regression analysis was performed to identify predictive factors of ICU mortality and shock occurrence.
Results
133 patients [median age 53 (39, 64), 72.2 % males] were included. Underlying immunosuppression was present in 127 patients, mostly long-term corticosteroid treatment in 111 (83.5 %) patients. Fever (80.8 %), respiratory (88.6 %), and gastrointestinal (71.2 %) symptoms were common clinical manifestations. Shock occurred in 75 (57.3 %) patients and mechanical ventilation was required in 89 (67.9 %) patients. Hypereosinophilia and a concomitant bacterial infection were observed in 34 (34.3 %) and 51 (38.4 %) patients, respectively. The in-ICU mortality rate was 60.3 %. Predictive factors of ICU mortality were shock occurrence [Odds ratio (OR) 18.1, 95 % confidence interval (95 % CI) 3.03–107.6, p < 0.01] and mechanical ventilation (OR 28.1, 95 % CI 3.6–217, p < 0.01). Hypereosinophilia (OR 0.21, 95 % CI 0.06–0.7, p = 0.01) and a concomitant bacterial infection (OR 4.68, 95 % CI 1.3–16.8, p = 0.02) were independent predictors of shock occurrence.
Conclusion
SHS remains associated with a poor outcome, especially when associated with shock and mechanical ventilation. Deterioration to shock is often related to concomitant bacterial infection. The poor outcome of established SHS pleads for a large application of antiparasitic primary prophylaxis in at-risk patients.
Similar content being viewed by others
References
Siddiqui AA, Berk SL. Diagnosis of Strongyloides stercoralis infection. Clin Infect Dis Off Publ Infect Dis Soc Am. 2001;33:1040–7.
Vadlamudi RS, Chi DS, Krishnaswamy G. Intestinal strongyloidiasis and hyperinfection syndrome. Clin Mol Allergy CMA. 2006;4:8.
Schär F, Trostdorf U, Giardina F, Khieu V, Muth S, Marti H, et al. Strongyloides stercoralis: global Distribution and Risk Factors. Plos Negl Trop Dis. 2013;7:e2288.
Ramanathan R, Nutman T. Strongyloides stercoralis infection in the immunocompromised host. Curr Infect Dis Rep. 2008;10:105–10.
Keiser PB, Nutman TB. Strongyloides stercoralis in the immunocompromised population. Clin Microbiol Rev. 2004;17:208–17.
Concha R, Harrington W Jr, Rogers AI. Intestinal strongyloidiasis: recognition, management, and determinants of outcome. J Clin Gastroenterol. 2005;39:203–11.
Debussche X, Toublanc M, Camillieri JP, Assan R. Overwhelming strongyloidiasis in a diabetic patient following ACTH treatment and keto-acidosis. Diabète Métabolisme. 1988;14:294–8.
Rivera E, Maldonado N, Vélez-García E, Grillo AJ, Malaret G. Hyperinfection syndrome with Strongyloides stercoralis. Ann Intern Med. 1970;72:199–204.
Milder JE, Walzer PD, Kilgore G, Rutherford I, Klein M. Clinical features of Strongyloides stercoralis infection in an endemic area of the United States. Gastroenterology. 1981;80:1481–8.
Montes M, Sanchez C, Verdonck K, Lake JE, Gonzalez E, Lopez G, et al. Regulatory T cell expansion in HTLV-1 and strongyloidiasis co-infection is associated with reduced IL-5 responses to Strongyloides stercoralis antigen. Plos Negl Trop Dis. 2009;3:e456.
Porto AF, Neva FA, Bittencourt H, Lisboa W, Thompson R, Alcântara L, et al. HTLV-1 decreases Th2 type of immune response in patients with strongyloidiasis. Parasite Immunol. 2001;23:503–7.
Blankenhaus B, Klemm U, Eschbach M-L, Sparwasser T, Huehn J, Kühl AA, et al. Strongyloides ratti infection induces expansion of Foxp3+ regulatory T cells that interfere with immune response and parasite clearance in BALB/c mice. J Immunol Baltim Md. 1950;2011(186):4295–305.
Galioto AM, Hess JA, Nolan TJ, Schad GA, Lee JJ, Abraham D. Role of eosinophils and neutrophils in innate and adaptive protective immunity to larval strongyloides stercoralis in mice. Infect Immun. 2006;74:5730–8.
Herbert DR, Lee JJ, Lee NA, Nolan TJ, Schad GA, Abraham D. Role of IL-5 in innate and adaptive immunity to larval Strongyloides stercoralis in mice. J Immunol Baltim Md. 1950;2000(165):4544–51.
Kerepesi LA, Hess JA, Nolan TJ, Schad GA, Abraham D. Complement component C3 is required for protective innate and adaptive immunity to larval strongyloides stercoralis in mice. J Immunol Baltim Md. 1950;2006(176):4315–22.
Rotman HL, Yutanawiboonchai W, Brigandi RA, Leon O, Gleich GJ, Nolan TJ, et al. Strongyloides stercoralis: eosinophil-dependent immune-mediated killing of third stage larvae in BALB/cByJ mice. Exp Parasitol. 1996;82:267–78.
Padigel UM, Hess JA, Lee JJ, Lok JB, Nolan TJ, Schad GA, et al. Eosinophils act as antigen-presenting cells to induce immunity to Strongyloides stercoralis in mice. J Infect Dis. 2007;196:1844–51.
Padigel UM, Lee JJ, Nolan TJ, Schad GA, Abraham D. Eosinophils can function as antigen-presenting cells to induce primary and secondary immune responses to Strongyloides stercoralis. Infect Immun. 2006;74:3232–8.
Coffman RL, Seymour BW, Hudak S, Jackson J, Rennick D. Antibody to interleukin-5 inhibits helminth-induced eosinophilia in mice. Science. 1989;245:308–10.
Grimaldi JC, Yu NX, Grunig G, Seymour BW, Cottrez F, Robinson DS, et al. Depletion of eosinophils in mice through the use of antibodies specific for C-C chemokine receptor 3 (CCR3). J Leukoc Biol. 1999;65:846–53.
Gurish MF, Humbles A, Tao H, Finkelstein S, Boyce JA, Gerard C, et al. CCR3 is required for tissue eosinophilia and larval cytotoxicity after infection with Trichinella spiralis. J Immunol Baltim Md. 1950;2002(168):5730–6.
Liu H-C, Hsu J-Y, Chang K-M. Strongyloides stercoralis hyperinfection presenting with symptoms mimicking acute exacerbation of chronic obstructive pulmonary disease. J Chin Med Assoc. 2009;72:442–5.
Lagacé-Wiens PRS, Harding GKM. A Canadian immigrant with coinfection of Strongyloides stercoralis and human T-lymphotropic virus 1. Can Med Assoc J . 2007;177:451–3.
Igra-Siegman Y, Kapila R, Sen P, Kaminski ZC, Louria DB. Syndrome of hyperinfection with Strongyloides stercoralis. Rev Infect Dis. 1981;3:397–407.
Adedayo O, Grell G, Bellot P. Hyperinfective strongyloidiasis in the medical ward: review of 27 cases in 5 years. South Med J. 2002;95:711–6.
Fardet L, Généreau T, Poirot J-L, Guidet B, Kettaneh A, Cabane J. Severe strongyloidiasis in corticosteroid-treated patients: case series and literature review. J Infect. 2007;54:18–27.
Coulter C, Walker DG, Günsberg M, Brown IG, Bligh JF, Prociv P. Successful treatment of disseminated strongyloidiasis. Med J Aust. 1992;157:331–2.
Ghoshal UC, Ghoshal U, Jain M, Kumar A, Aggarwal R, Misra A, et al. Strongyloides stercoralis infestation associated with septicemia due to intestinal transmural migration of bacteria. J Gastroenterol Hepatol. 2002;17:1331–3.
Kakati B, Dang S, Heif M, Caradine K, McKnight W, Aduli F. Strongyloides duodenitis: case report and review of literature. J Natl Med Assoc. 2011;103:60–3.
Gutierrez Y, Bhatia P, Garbadawala ST, Dobson JR, Wallace TM, Carey TE. Strongyloides stercoralis eosinophilic granulomatous enterocolitis. Am J Surg Pathol. 1996;20:603–12.
Sipahi AM, Damião AO, Simionato CS, Bonini N, Santos MA, de Moraes-Filho JP, et al. Small bowel bacterial overgrowth in strongyloidiasis. Digestion. 1991;49:120–4.
Younis AE, Soblik H, Ajonina-Ekoti I, Erttmann KD, Luersen K, Liebau E, et al. Characterization of a secreted macrophage migration inhibitory factor homologue of the parasitic nematode Strongyloides acting at the parasite-host cell interface. Microbes Infect Inst Pasteur. 2012;14:279–89.
Pastrana DV, Raghavan N, FitzGerald P, Eisinger SW, Metz C, Bucala R, et al. Filarial nematode parasites secrete a homologue of the human cytokine macrophage migration inhibitory factor. Infect Immun. 1998;66:5955–63.
Suputtamongkol Y, Premasathian N, Bhumimuang K, Waywa D, Nilganuwong S, Karuphong E, et al. Efficacy and safety of single and double doses of ivermectin versus 7-day high dose albendazole for chronic strongyloidiasis. Plos Negl Trop Dis. 2011;5:e1044.
Muennig P, Pallin D, Challah C, Khan K. The cost-effectiveness of ivermectin vs. albendazole in the presumptive treatment of strongyloidiasis in immigrants to the United States. Epidemiol Infect. 2004;132:1055–63.
Hauber HP, Galle J, Chiodini PL, Rupp J, Birke R, Vollmer E, et al. Fatal outcome of a hyperinfection syndrome despite successful eradication of Strongyloides with subcutaneous ivermectin. Infection. 2005;33:383–6.
Leung V, Al-Rawahi GN, Grant J, Fleckenstein L, Bowie W. Case report: failure of subcutaneous ivermectin in treating Strongyloides hyperinfection. Am J Trop Med Hyg. 2008;79:853–5.
Lichtenberger P, Rosa-Cunha I, Morris M, Nishida S, Akpinar E, Gaitan J, et al. Hyperinfection strongyloidiasis in a liver transplant recipient treated with parenteral ivermectin. Transpl Infect Dis Off J Transplant Soc. 2009;11:137–42.
Pacanowski J, Santos MD, Roux A, Maignan CLE, Guillot J, Lavarde V, et al. Subcutaneous ivermectin as a safe salvage therapy in Strongyloides stercoralis hyperinfection syndrome: a case report. Am J Trop Med Hyg. 2005;73:122–4.
Santiago M, Leitão B. Prevention of strongyloides hyperinfection syndrome: a rheumatological point of view. Eur J Intern Med. 2009;20:744–8.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Groupe de Recherche sur la Réanimation Respiratoire en Onco-Hématologie (Grrr-OH).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Geri, G., Rabbat, A., Mayaux, J. et al. Strongyloides stercoralis hyperinfection syndrome: a case series and a review of the literature. Infection 43, 691–698 (2015). https://doi.org/10.1007/s15010-015-0799-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-015-0799-1