Abstract
Purpose
Urinary tract infections (UTIs), the most common serious bacterial infections in children, are frequently caused by Escherichia coli. The purpose of this study was to investigate E. coli resistance/multidrug resistance to antibiotics most frequently used for UTIs.
Methods
Children 0–18 years of age, hospitalized at the University Pediatric Hospital in Novi Sad, Serbia, were included in a 1-year observational prospective study. The microbiological analysis was performed using the standard Kirby–Bauer disk diffusion method. The results were analyzed using WHONET 5.4 software.
Results
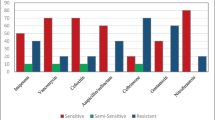
E. coli was isolated from 61.7 % of positive urine specimens. In general, higher average E. coli antibiotic resistance was found in infants and toddlers compared to children and adolescents (33.4 vs. 25.0 %) (p < 0.0001). Furthermore, it was observed that the average resistance to all the tested antibiotics was higher in boys than in girls (37.0 vs. 25.1 %) (p < 0.0001). E. coli was highly susceptible to piperacillin/tazobactam (>93.1 %), amikacin (86.3 %), quinolones (>75.0 %), and penems (>96.6 %). The prevalence of multiresistant E. coli strains was significantly higher in infants and toddlers (72.3 vs. 36.8 %) (p < 0.0001).
Conclusions
E. coli, a common cause of UTIs in children admitted to pediatric hospitals, is highly resistant/multidrug-resistant to commonly used antibiotics. Higher average resistance is found in infants and toddlers than in children and adolescents, as well as in boys compared to girls. These findings are important for the regional empiric therapy of UTIs and call for actions to decrease E. coli antibiotic resistance.

Similar content being viewed by others
References
Chung A, Perera R, Brueggemann AB, Elamin AE, Harnden A, Mayon-White R, Smith S, Crook DW, Mant D. Effect of antibiotic prescribing on antibiotic resistance in individual children in primary care: prospective cohort study. BMJ. 2007;335:429.
Henderson KL, Muller-Pebody B, Johnson AP, Goossens H, Sharland M; ARPEC Group. First set-up meeting for Antibiotic Resistance and Prescribing in European Children (ARPEC). Euro Surveill. 2009;14(45). pii = 19404.
Lutter SA, Currie ML, Mitz LB, Greenbaum LA. Antibiotic resistance patterns in children hospitalized for urinary tract infections. Arch Pediatr Adolesc Med. 2005;159:924–8.
Marcus N, Ashkenazi S, Samra Z, Cohen A, Livni G. Community-acquired Pseudomonas aeruginosa urinary tract infections in children hospitalized in a tertiary center: relative frequency, risk factors, antimicrobial resistance and treatment. Infection. 2008;36:421–6.
Catal F, Bavbek N, Bayrak O, Karabel M, Karabel D, Odemis E, Uz E. Antimicrobial resistance patterns of urinary tract pathogens and rationale for empirical therapy in Turkish children for the years 2000–2006. Int Urol Nephrol. 2009;41:953–7.
Yared A, Edwards KM. Reevaluating antibiotic therapy for urinary tract infections in children. Arch Pediatr Adolesc Med. 2005;159:992–3.
Winberg J, Andersen HJ, Bergström T, Jacobsson B, Larson H, Lincoln K. Epidemiology of symptomatic urinary tract infection in childhood. Acta Paediatr Scand Suppl. 1974;252:1–20.
Hellström A, Hanson E, Hansson S, Hjälmås K, Jodal U. Association between urinary symptoms at 7 years old and previous urinary tract infection. Arch Dis Child. 1991;66:232–4.
Kunin CM. Epidemiology and natural history of urinary tract infection in school age children. Pediatr Clin North Am. 1971;18:509–28.
Welch TR, Forbes PA, Drummond KN, Nogrady MB. Recurrent urinary tract infection in girls. Group with lower tract findings and a benign course. Arch Dis Child. 1976;51:114–9.
Ashkenazi S, Even-Tov S, Samra Z, Dinari G. Uropathogens of various childhood populations and their antibiotic susceptibility. Pediatr Infect Dis J. 1991;10:742–6.
Hellerstein S. Urinary tract infections. Old and new concepts. Pediatr Clin North Am. 1995;42:1433–57.
Schlager TA. Urinary tract infections in children younger than 5 years of age: epidemiology, diagnosis, treatment, outcomes and prevention. Paediatr Drugs. 2001;3:219–27.
Ronald A. The etiology of urinary tract infection: traditional and emerging pathogens. Dis Mon. 2003;49:71–82.
Quinonez JM. The continuing saga of antimicrobial resistance. Medscape Pediatrics. Medscape Education. 2004. http://www.medscape.org/viewarticle/495300. Accessed 24 Feb 2013.
Green M, Martin JM, Barbadora KA, Beall B, Wald ER. Reemergence of macrolide resistance in pharyngeal isolates of group a streptococci in southwestern Pennsylvania. Antimicrob Agents Chemother. 2004;48:473–6.
FAAIR Scientific Advisory Panel. Policy recommendations. Clin Infect Dis. 2002;34:S76–7.
Zaidi AK, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA. Hospital-acquired neonatal infections in developing countries. Lancet. 2005;365:1175–88.
Livermore DM. Bacterial resistance: origins, epidemiology, and impact. Clin Infect Dis. 2003;36:S11–23.
Brinsley KJ, Sinkowitz-Cochran RL, Cardo DM; CDC Campaign to Prevent Antimicrobial Resistance Team. Assessing motivation for physicians to prevent antimicrobial resistance in hospitalized children using the Health Belief Model as a framework. Am J Infect Control. 2005;33:175–81.
Yüksel S, Oztürk B, Kavaz A, Ozçakar ZB, Acar B, Güriz H, Aysev D, Ekim M, Yalçinkaya F. Antibiotic resistance of urinary tract pathogens and evaluation of empirical treatment in Turkish children with urinary tract infections. Int J Antimicrob Agents. 2006;28:413–6.
Ilić K, Jakovljević E, Skodrić-Trifunović V. Social-economic factors and irrational antibiotic use as reasons for antibiotic resistance of bacteria causing common childhood infections in primary healthcare. Eur J Pediatr. 2012;171:767–77.
Levy SB. Antibiotic resistance: consequences of inaction. Clin Infect Dis. 2001;33:S124–9.
Accinelli C, Koskinen WC, Becker JM, Sadowsky MJ. Environmental fate of two sulfonamide antimicrobial agents in soil. J Agric Food Chem. 2007;55:2677–82.
Grigoryan L, Burgerhof JG, Haaijer-Ruskamp FM, Degener JE, Deschepper R, Monnet DL, Di Matteo A, Scicluna EA, Bara AC, Lundborg CS, Birkin J; SAR Group. Is self-medication with antibiotics in Europe driven by prescribed use? J Antimicrob Chemother. 2007;59:152–6.
Cizman M, Beovic B, Krcmery V, Barsic B, Tamm E, Ludwig E, Pelemis M, Karovski K, Grzesiowski P, Gardovska D, Volokha A, Keuleyan E, Stratchounski L, Dumitru C, Titov LP, Usonis V, Dvorák P. Antibiotic policies in Central Eastern Europe. Int J Antimicrob Agents. 2004;24:199–204.
Mandell LA, Peterson LR, Wise R, Hooper D, Low DE, Schaad UB, Klugman KP, Courvalin P. The battle against emerging antibiotic resistance: should fluoroquinolones be used to treat children? Clin Infect Dis. 2002;35:721–7.
Zhanel GG, Wang X, Nichol K, Nikulin A, Wierzbowski AK, Mulvey M, Hoban DJ. Molecular characterisation of Canadian paediatric multidrug-resistant Streptococcus pneumoniae from 1998–2004. Int J Antimicrob Agents. 2006;28:465–71.
Whitney CG, Farley MM, Hadler J, Harrison LH, Lexau C, Reingold A, Lefkowitz L, Cieslak PR, Cetron M, Zell ER, Jorgensen JH, Schuchat A; Active Bacterial Core Surveillance Program of the Emerging Infections Program Network. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med. 2000;343:1917–24.
Doern GV, Heilmann KP, Huynh HK, Rhomberg PR, Coffman SL, Brueggemann AB. Antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States during 1999–2000, including a comparison of resistance rates since 1994–1995. Antimicrob Agents Chemother. 2001;45:1721–9.
Al-Tawfiq JA, Antony A. Antimicrobial resistance of Klebsiella pneumoniae in a Saudi Arabian hospital: results of a 6-year surveillance study, 1998–2003. J Infect Chemother. 2007;13:230–4.
Rolston KV. New antimicrobial agents for the treatment of bacterial infections in cancer patients. Hematol Oncol. 2009;27:107–14.
Yao K, Shen X, Yul S, Lu Q, Deng L, Ye Q, Zhang H, Deng Q, Hu Y, Yang Y. Antimicrobial resistance and serotypes of nasopharyngeal strains of Streptococcus pneumoniae in Chinese children with acute respiratory infections. J Int Med Res. 2007;35:253–67.
World Health Organization (WHO). Surveillance standards for antimicrobial resistance (WHO/CDS/CSR/DRS/2001.5). 2002. http://whqlibdoc.who.int/hq/2002/WHO_CDS_CSR_DRS_2001.5.pdf. Accessed 24 Feb 2013.
World Health Organization (WHO). WHO Global Strategy for Containment of Antimicrobial Resistance (WHO/CDS/CSR/DRS/2001.2a). 2001. http://whqlibdoc.who.int/hq/2001/WHO_CDS_CSR_DRS_2001.2a.pdf. Accessed 24 Feb 2013.
O’Brien TF, Stelling JM. WHONET: an information system for monitoring antimicrobial resistance. Emerg Infect Dis. 1995;1:66.
Rocha JL, Tuon FF, Johnson JR. Sex, drugs, bugs, and age: rational selection of empirical therapy for outpatient urinary tract infection in an era of extensive antimicrobial resistance. Braz J Infect Dis. 2012;16:115–21.
Johnson JR, Urban C, Weissman SJ, Jorgensen JH, Lewis JS 2nd, Hansen G, Edelstein PH, Robicsek A, Cleary T, Adachi J, Paterson D, Quinn J, Hanson ND, Johnston BD, Clabots C, Kuskowski MA; AMERECUS Investigators. Molecular epidemiological analysis of Escherichia coli sequence type ST131 (O25:H4) and blaCTX-M-15 among extended-spectrum-β-lactamase-producing E. coli from the United States, 2000 to 2009. Antimicrob Agents Chemother. 2012;56:2364–70.
European Medicines Agency (EMA). Note for Guidance on Clinical Investigation of Medicinal Products in the Paediatric Population (CPMP/ICH/2711/99). 2001. http://www.emea.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002926.pdf. Accessed 24 Feb 2013.
Horvat O. Utilization of antibiotics in outhospital conditions in South-Backa district. Dissertation, School of Medicine, University of Novi Sad, Serbia; 2010.
English M, Mohammed S, Ross A, Ndirangu S, Kokwaro G, Shann F, Marsh K. A randomised, controlled trial of once daily and multi-dose daily gentamicin in young Kenyan infants. Arch Dis Child. 2004;89:665–9.
Hey E. Unlicensed and off label drug use in neonates. Arch Dis Child Fetal Neonatal Ed. 2000;82:F77–8.
Meier S, Weber R, Zbinden R, Ruef C, Hasse B. Extended-spectrum β-lactamase-producing Gram-negative pathogens in community-acquired urinary tract infections: an increasing challenge for antimicrobial therapy. Infection. 2011;39:333–40.
Elder JS. Urinary tract infections. In: Behrman RE, Kliegman RM, Jenson HB, editors. Nelson textbook of pediatrics. 16th ed. Philadelphia: WB Saunders Company; 2000. p. 1621–5.
Sharland M; SACAR Paediatric Subgroup. The use of antibacterials in children: a report of the Specialist Advisory Committee on Antimicrobial Resistance (SACAR) Paediatric Subgroup. J Antimicrob Chemother. 2007;60:i15–26.
Bartoloni A, Pallecchi L, Benedetti M, Fernandez C, Vallejos Y, Guzman E, Villagran AL, Mantella A, Lucchetti C, Bartalesi F, Strohmeyer M, Bechini A, Gamboa H, Rodríguez H, Falkenberg T, Kronvall G, Gotuzzo E, Paradisi F, Rossolini GM. Multidrug-resistant commensal Escherichia coli in children, Peru and Bolivia. Emerg Infect Dis. 2006;12:907–13.
International Monetary Fund. Tensions from the Two-Speed Recovery; Unemployment, Commodities, and Capital Flows. 2011. http://www.imf.org/external/pubs/ft/weo/2011/01/pdf/text.pdf. Accessed 24 Feb 2013.
Stefan-Mikić S. Antibiotic utilisation surveillance from pharmacoeconomic/pharmacotherapeutic standpoint with control of bacterial resistance. Med Pregl. 2008;61:7–8.
Tseng SH, Lee CM, Lin TY, Chang SC, Chang FY. Emergence and spread of multi-drug resistant organisms: think globally and act locally. J Microbiol Immunol Infect. 2011;44:157–65.
Doyle E. CDC: act locally, participate regionally, to combat antimicrobial resistance. Today’s Hospitalist. 2006. http://www.todayshospitalist.com/index.php?b=articles_read&cnt=73. Accessed 24 Feb 2013.
Acknowledgments
Katarina Ilić’s work is supported by the Ministry of Education and Science, Republic of Serbia, Project No. 175064, 2011-2014. Part of the data collected within the first 5 months of the study were presented orally at the 16th World Congress of Basic and Clinical Pharmacology (Copenhagen, Denmark, 17–23 July 2010) and published in an abstract form in Basic and Clinical Pharmacology and Toxicology 2010; 107(Suppl 1), p. 135. The 12-month data were presented in a poster session of the 2011 Annual Meeting of the American Society for Clinical Pharmacology and Therapeutics (Dallas, Texas, USA, 2–5 March 2011) and published in an abstract form in Clinical Pharmacology and Therapeutics 2011; 89(Suppl 1), p. S64.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jakovljević, E., Ilić, K., Jelesić, Z. et al. A one-year prospective study on the antibiotic resistance of E. coli strains isolated in urinary specimens of children hospitalized at the University Pediatric Medical Center in Novi Sad, Serbia. Infection 41, 1111–1119 (2013). https://doi.org/10.1007/s15010-013-0493-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-013-0493-0