Abstract
Purpose
Hitherto, studies on highly active antiretroviral therapy (HAART) initiation have shown partly inconsistent results. Our study investigated the clinical course and course of immune status after HAART initiation at CD4-cell-count/μl of treated patients between 250 and 349 (group 1), compared to 350–449 (group 2), on the basis of the cohort of the Competence Network for HIV/AIDS (KompNet cohort).
Methods
Patients had to be HAART-naïve. Medication had to start at the earliest in 1996, being at least triple combination therapy. The primary endpoints of death, first AIDS-defining illness and first drop of CD4-cell-count/μl below 200 were evaluated as censored event times between the initiation of HAART (t 0) and the date of the first event/date of last observation. Probabilities of event-free intervals since t 0 were calculated by Kaplan–Meier estimation, compared by logrank tests. The results were adjusted for confounders using Cox regression. Additionally, incidences were estimated.
Results
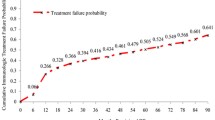
A total of 822 patients met the inclusion criteria (group 1: 526, group 2: 296), covering 4,133 patient years (py) overall. In group 1, 0.64 death cases/100 py were found, with the corresponding vale being 0.17 in group 2. In group 1, 1.38 AIDS-defining events/100 py occurred, whereas it was 0.78 in group 2. In group 1, 2.64 events of first drop of CD4-cell-count/μl below 200 occurred per 100 py, compared to 0.77 in group 2. Kaplan–Meier estimations showed borderline significant differences regarding death (p = 0.063), no differences regarding first AIDS-defining illness (p = 0.148) and distinct differences regarding the first drop of CD4-cell-count/μl below 200 (p = 0.0004).
Conclusions
The results gave a strong hint for a therapy initiation at higher CD4-cell-count/μl regarding the outcome of death in treated patients. A distinct benefit was shown regarding the first decline of CD4-cell-count/μl below 200.


Similar content being viewed by others
Notes
Central clinical and therapy related data of patients regarding the time before enrolment into the cohort are documented retrospectively [3]. Due to the high proportion of data documented retrospectively before 2005, the calendar year of the start of HAART (<2005 vs. ≥2005) was considered as a confounder to adjust for potential influences of different modes of data documentation (retrospective vs. prospective).
The percentage of quarters with a documented CD4-cell-count/μl measurement is lower for the subpopulation with an observation time ≥3 years than in all patients. For the analysis shown in Table 3, a fixed datum reference of 12 quarters was used as a basis for the analyses due to the observation period of at least 3 years. Because not every patient had a CD4-cell-count/μl measurement just in the 12 quarter, the named percentage is lower.
It was not reasonable to calculate the incidences of death for this subpopulation due to the inclusion criteria of this group (observation period at least 3 years) and due to seven cases of death within the first 3 years.
References
Emery S, Neuhaus JA, Phillips AN, et al. Major clinical outcomes in antiretroviral therapy (ART)-naive participants and in those not receiving ART at baseline in the SMART study. J Infect Dis. 2008;197:1133–44.
Strategies for Management of Antiretroviral Therapy (SMART) Study Group. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283–96.
Kitahata MM, Gange SJ, Abraham AG, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360(18):1815–26.
Sterne JA, May M, Costagliola D, et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009;373(9672):1352–63.
Ahdieh-Grant L, Yamashita TE, Phair JP, et al. When to initiate highly active antiretroviral therapy: a cohort approach. Am J Epidemiol. 2003;157:738–46.
Anastos K, Barrón Y, Miotti P, et al. Risk of progression to AIDS and death in women infected with HIV-1 initiating highly active antiretroviral treatment at different stages of disease. Arch Intern Med. 2002;162:1973–80.
Hughes MD, Ribaudo HR. The search for data on when to start treatment for HIV infection. J Infect Dis. 2008;197:1084–6.
Opravil M, Ledergerber B, Furrer H, et al. Clinical efficacy of early initiation of HAART in patients with asymptomatic HIV infection and CD4 cell count >350 × 10(6)/l. AIDS. 2002;16:1371–81.
Palella FJ Jr, Deloria-Knoll M, Chmiel JS, et al. Survival benefit of initiating antiretroviral therapy in HIV-infected persons in different CD4+ cell strata. Ann Intern Med. 2003;138:620–6.
Sterling TR, Chaisson RE, Moore RD. HIV-1 RNA, CD4 T-lymphocytes, and clinical response to highly active antiretroviral therapy. AIDS. 2001;15:2251–7.
Sterling TR, Chaisson RE, Moore RD. Initiation of highly active antiretroviral therapy at CD4+ T lymphocyte counts of >350 cells/mm3: disease progression, treatment durability, and drug toxicity. Clin Infect Dis. 2003;36:812–5.
Zolopa A, Andersen J, Powderly W, et al. Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: a multicenter randomized strategy trial. PLoS ONE. 2009;4(5):e5575.
Grant P, Zolopa A. Initiation of antiretroviral therapy in the hospitalized patient with an acute AIDS-related opportunistic infection and other conditions: no time to lose. Curr HIV/AIDS Rep. 2009;6(2):63–7.
Phillips AN, Gazzard B, Gilson R, et al. Rate of AIDS diseases or death in HIV-infected antiretroviral therapy-naive individuals with high CD4 cell count. AIDS. 2007;21(13):1717–21.
May MT, Sterne JA, Costagliola D, et al. HIV treatment response and prognosis in Europe and North America in the first decade of highly active antiretroviral therapy: a collaborative analysis. Lancet. 2006;368(9534):451–8.
Bonnet F, Thiébaut R, Chêne G, et al. Determinants of clinical progression in antiretroviral-naive HIV-infected patients starting highly active antiretroviral therapy. Aquitaine Cohort, France, 1996–2002. HIV Med. 2005;6(3):198–205.
Chêne G, Sterne JA, May M, et al. Prognostic importance of initial response in HIV-1 infected patients starting potent antiretroviral therapy: analysis of prospective studies. Lancet. 2003;362(9385):679–86.
Jacobson LP, Li R, Phair J, et al. Evaluation of the effectiveness of highly active antiretroviral therapy in persons with human immunodeficiency virus using biomarker-based equivalence of disease progression. Am J Epidemiol. 2002;155(8):760–70.
Thompson MA, Aberg JA, Cahn P, et al. Antiretroviral treatment of adult HIV infection: 2010 recommendations of the International AIDS Society USA—Panel. JAMA. 2010;304(3):321–33.
Clumeck N, Dedes N, Pozniak A, et al. Clinical management and treatment of HIV infected adults in Europe. EACS Guidelines Version 5.2. Available online at: http://www.europeanaidsclinicalsociety.org/guidelines.asp. Accessed 16 September 2010.
Lau B, Gange SJ, Kirk GD, et al. Evaluation of human immunodeficiency virus biomarkers: inferences from interval and clinical cohort studies. Epidemiology. 2009;20(5):664–72.
Jaén A, Esteve A, Miró JM, et al. Determinants of HIV progression and assessment of the optimal time to initiate highly active antiretroviral therapy: PISCIS Cohort (Spain). J Acquir Immune Defic Syndr. 2008;47(2):212–20.
Stöhr W, Dunn D, Porter K, et al. CD4 cell count and initiation of antiretroviral therapy: trends in seven UK centres, 1997–2003. HIV Med. 2007;8(3):135–41.
May M, Sterne JA, Sabin C, et al. Prognosis of HIV-1-infected patients up to 5 years after initiation of HAART: collaborative analysis of prospective studies. AIDS. 2007;21(9):1185–97.
Ho C, Lee S, Wong Kh, et al. Setting a minimum threshold CD4 count for initiation of highly active antiretroviral therapy in HIV-infected patients. HIV Med. 2007;8(3):181–5.
Lapadula G, Torti C, Maggiolo F, et al. Predictors of clinical progression among HIV-1-positive patients starting HAART with CD4+ T-cell counts > or = 200 cells/mm3. Antivir Ther. 2007;12(6):941–7.
Locadia M, van Grieken RA, Prins JM, et al. Patients’ preferences regarding the timing of highly active antiretroviral therapy initiation for chronic asymptomatic HIV-1 infection. Antivir Ther. 2006;11(3):335–41.
Fardet L, Mary-Krause M, Heard I, et al. Influence of gender and HIV transmission group on initial highly active antiretroviral therapy prescription and treatment response. HIV Med. 2006;7(8):520–9.
Ledergerber B, Lundgren JD, Walker AS, et al. Predictors of trend in CD4-positive T-cell count and mortality among HIV-1-infected individuals with virological failure to all three antiretroviral-drug classes. Lancet. 2004;364(9428):51–62.
Jansen K, Michalik C, Hahn M; Competence Network for HIV/AIDS, et al. The Patient Cohort of the German Competence Network For HIV/AIDS (KompNet): a profile. Eur J Med Res. 2009;14(10):323–31.
Jansen K, Brockmeyer NH, Hahn M; Competence Network for HIV/AIDS, et al. Epidemiological composition, clinical and treatment characteristics of the patient cohort of the German Competence Network for HIV/AIDS. Eur J Med Res. 2009;14(10):415–25.
Kalbfleisch JD, Prentice RL. The statistical analysis of failure time data. New York: Wiley; 1980. p. 21–38.
Kaplan JE, Hanson DL, Cohn DL, et al. When to begin highly active antiretroviral therapy? Evidence supporting initiation of therapy at CD4+ lymphocyte counts <350 cells/microL. Clin Infect Dis. 2003;37(7):951–8.
Palella F, Armon C, Buchacz K, et al. CD4 at HAART initiation predicts long-term CD4 responses and mortality from AIDS and non-AIDS causes in the HIV Outpatient Study (HOPS). In: Proceedings of the 17th Annual Canadian Conference on HIV/AIDS Research, Saskatoon, Canada, May 2010. San Francisco, CA: CROI; 2010. Abstract 983.
Antiretroviral Therapy Cohort Collaboration. Causes of death in HIV-1-infected patients treated with antiretroviral therapy, 1996–2006: collaborative analysis of 13 HIV cohort studies. Clin Infect Dis. 2010;50(10):1387–96.
HIV-CAUSAL Collaboration. The effect of combined antiretroviral therapy on the overall mortality of HIV-infected individuals. AIDS. 2010;24(1):123–37.
Acknowledgments
Firstly, we thank all of the patients participating in our cohort for providing their data and biomaterials to the study. We are grateful for all the work and dedication of the documentation officers and of the heads of our documenting sites. We thank the Ruhr University Bochum for the financial and structural encouragement. We thank the Federal Ministry of Education and Research especially for its ongoing financial and ideal support since 2002 (grant no. BMBF-01 KI 0501). The following documenting sites currently contribute data to the basis module of the KompNet cohort: Gemeinschaftspraxis Driesener Straße, Berlin; Gemeinschaftspraxis Mehringdamm, Berlin; Gemeinschaftspraxis Turmstraße, Berlin; Gemeinschaftspraxis Fuggerstraße, Berlin; Praxiszentrum Kaiserdamm, Berlin; Universitätsklinikum Benjamin Franklin, Charité, Berlin; Dermatologische Klinik, Ruhr Universität, Bochum; Klinikum, Dortmund; Universitätsklinikum, Düsseldorf; Medizinische Klinik 3, Universitätsklinikum, Erlangen; Klinik für Dermatologie, Universität Essen; HIVCENTER, Universitätsklinikum, Frankfurt; Ifi-Institut, Hamburg; Infektionsmedizinisches Centrum Hamburg (ICH), Hamburg; Medizinische Hochschule, Hannover; Praxis Georgstraße, Hannover; Gemeinschaftspraxis, Kriegsstraße, Karlsruhe; Städtisches Krankenhaus Kemperhof, Koblenz; Praxis Hohenstaufenring, Köln; Gemeinschaftspraxis Isartorplatz, München; MVZ Karlsplatz, HIV Research and Clinical Centre, München; Praxisgemeinschaft Franz Joseph-Straße, München; Klinikum, Osnabrück; Gemeinschaftspraxis Ulmer/Frietsch/Müller, Stuttgart.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Plettenberg, A., Brockmeyer, N.H., Haastert, B. et al. Impact of earlier HAART initiation on the immune status and clinical course of treated patients on the basis of cohort data of the German Competence Network for HIV/AIDS. Infection 39, 3–12 (2011). https://doi.org/10.1007/s15010-010-0070-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-010-0070-8