Abstract
Background:
Given the high incidence (1.5%–10%) of invasive aspergillosis (IA) after liver transplantation and the associated mortality, prophylaxis according to the patients’ circumstances is a reasonable approach. The purpose of this investigation was to determine the effect and significance of risk factors for IA in a specialized transplantation center.
Methods:
We collected data from patients who underwent liver transplantation at the Transplantation Center of the University Hospital Heidelberg (Germany) between December 2001 and December 2004 in a specifically designed database for retrospective analysis. Invasive aspergillosiswas defined according to the European Organization for Research and Treatment of Cancer classifications. Univariate analysis and logistic regression were performed to assess the influence of each assumed risk factor.
Results:
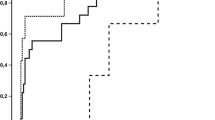
A total of 195 liver transplantationswere performed in 170 patients, with two patients (1.2%) developing a proven IA, seven (4.1%) developing a probable IA, and five developing a possible IA (2.9%). All patients received oral itraconazole prophylaxis. Of these 14 patients with proven, probable or possible IA, 13 died within 4 weeks after the initial diagnosis; this represents 33.3% of all patients with a fatal outcome. Univariate significant factors were retransplantation (p = 0.004), cytomegalovirus (CMV) infection (p = 0.024), dialysis (p < 0.001), renal insufficiency (p = 0.05), thrombocytopenia (p = 0.001), and leukocytopenia (p = 0.002). Multivariate analysis showed an independent influence of CMV infection (OR 6.032, 95% CI 1.446–25.163) and dialysis (OR 14.985, 95%CI 2.936–76.486).
Conclusion:
The rate of IA found in this investigation is within the range reported in published studies. Based on our data, extended antifungal prophylaxis should be given to liver transplant patients with specific risk factors, such as renal insufficiency, requirement for dialysis, CMV infection, or thrombocytopenia. Additional focus should be on the prevention of CMV infections.
Similar content being viewed by others
Abbreviations
- CMV::
-
Cytomegalovirus
- CT::
-
Computer tomography
- EORTC::
-
European Organization for Research and Treatment of Cancer
- IA::
-
Invasive aspergillosis
- OLT::
-
Orthotopic liver transplantation
- SAPS::
-
Simplified acute physiology score
- SOT::
-
Solid organ transplantation
- UNOS::
-
United Network for Organ Sharing
References
Paterson DL, Singh N: Invasive aspergillosis in transplant recipients. Medicine (Baltimore) 1999; 78: 123–138.
Kusne S, Troke PF, Marino IR: Factors associated with invasive lung aspergillosis and the significance of positive Aspergillus culture after liver transplantation. J Infect Dis 1992; 166: 1379–1383.
Paya CV, Hermans PE, Washington JA, et al. Incidence, distribution and outcome of episodes of infection in 100 orthotopic liver transplantations. Mayo Clin Proc 1993; 64: 555–564.
Singh N, Mieles L, Yu VL, Gayowski T: Invasive aspergillosis in liver transplant recipients: association with candidemia and consumption coagulopathy and failure of prophylaxis with low-dose amphotericin B. Clin Infect Dis 1993; 17: 906–908.
Denning DW: Echinocandin antifungal drugs. Lancet 2003; 362: 1142–1151.
Denning DW, Ribaud P, Milpied N, Caillot D, Herbrecht R, Thiel E, Haas A, Ruhnke M, Lode H: Efficacy and safety of voriconazole in the treatment of acute invasive aspergillosis. Clin Infect Dis 2002; 34: 563–571.
Fisher NC, Singhal S, Miller SJ, Hastings JGM, Mutimer DJ: Fungal infection and liposomal amphotericin B (AmBisome) therapy in liver transplantation: a 2 year review. J Antimicrob Chemother 1999; 43: 597–600.
Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, Kern WV, Marr KA, Ribaud P, Lortholary O, Sylvester R, Rubin RH, Wingard JR, Stark P, Durand C, Caillot D, Thiel E, Chandrasekar PH, Hodges MR, Schlamm HT, Troke PF, de Pauw B, The Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 2002; 347: 408–415.
Alexander BD: Prophylaxis of invasive mycoses in solid organ transplantation. Curr Opin Infect Dis 2002; 15: 583–589.
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, Denning DW, Donnelly JP, Edwards JE, Erjavec Z, Fiere D, Lortholary O, Maertens J, Meis JF, Patterson TF, Ritter J, Selleslag D, Shah PM, Stevens DA, Walsh TJ: Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 2002; 34: 7–14.
Le Gall J-R, Lemeshow S, Saulnier F: A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 1993; 270: 2957–2963.
Singh N: The changing face of invasive aspergillosis in liver transplant recipients. Liver Transpl 2002; 8: 1071–1072.
Singh N, Avery RK, Munoz P, Pruett TL, Alexander B, Jacobs R, Tollemar JG, Dominguez EA, Yu CM, Paterson DL, Husain S, Kusne S, Linden P: Trends in risk profiles for and mortality associated with invasive aspergillosis among liver transplant recipients. Clin Infect Dis 2003; 36: 46–52.
Singh N, Paterson DL: Aspergillus infections in transplant recipients. Clin Microbiol Rev 2005; 18: 44–69.
Singh N, Arnow PM, Bonham A, Dominguez E, Paterson DL, Pankey GA, Wagener MM, Yu VL: Invasive aspergillosis in liver transplant recipients in the 1990 s. Transplantation 1997; 64: 716–720.
Singh N: Antifungal prophylaxis for solid organ transplant recipients: seeking clarity amidst controversy. Clin Infect Dis 2000; 31: 545–553.
Snydman DR: Infection in solid organ transplantation. Transpl Infect Dis 1999; 1: 21–28.
Rubin RH: The indirect effects of cytomegalovirus infection on the outcome of organ transplantation. JAMA 1989; 261: 3607–3609.
Singh N: Interactions between viruses in transplant recipients. Clin Infect Dis 2005; 40: 430–436.
George MJ, Snydman DR, Werner BG, Griffith J, Falagas ME, Dougherty NN, Rubin RH: The independent role of cytomegalovirus as a risk factor for invasive fungal disease in orthotopic liver transplant recipients. Boston Center for Liver Transplantation CMVIG-Study Group. Cytogam, MedImmune, Inc. Gaithersburg, Maryland. Am J Med 1997; 103: 106–113.
Singh N: Late-onset cytomegalovirus disease as a significant complication in solid organ transplant recipients receiving antiviral prophylaxis: a call to heed the mounting evidence. Clin Infect Dis 2005; 40: 704–708.
Snydman DR: Counterpoint: prevention of cytomegalovirus (CMV) infection and CMV disease in recipients of solid organ transplants: the case for prophylaxis. Clin Infect Dis 2005; 40: 709–712.
Singh N, Limaye AP, Forrest G, Safdar N, Munoz P, Pursell K, Houston S, Rosso F, Montoya JG, Patton PR, Del BR, Aguado JM, Wagener MM, Husain S: Late-onset invasive aspergillosis in organ transplant recipients in the current era. Med Mycol 2006; 44: 445–449.
Flechner SM, Kobashigawa J, Klintmalm G: Calcineurin inhibitorsparing regimens in solid organ transplantation: focus on improving renal function and nephrotoxicity. Clin Transplant 2008; 22: 1–15.
Sommerer C, Giese T, Schmidt J, Meuer S, Zeier M. Ciclosporin: A tapering monitored by NFAT-regulated gene expression: a new concept of individual immunosuppression. Transplantation 2008; 85: 15–21.
Potter M: Strategies for managing systemic fungal infection and the place of itraconazole. J Antimicrob Chemother 2005; 56 (Suppl 1): i49–i54.
Morgenstern GR, Prentice AG, Prentice HG, Ropner JE, Schey SA, Warnock DW: A randomized controlled trial of itraconazole versus fluconazole for the prevention of fungal infections in patients with haematological malignancies. U.K. Multicentre Antifungal Prophylaxis Study Group. Br J Haematol 1999; 105: 901–911.
Winston DJ, Busuttil RW: Randomized controlled trial of oral itraconazole solution versus intravenous/oral fluconazole for prevention of fungal infections in liver transplant recipients. Transplantation 2002; 74: 688–695.
Mora NP, Klintmalm G, Solomon H, Goldstein RM, Gonwa TA, Husberg BS: Selective amphotericin B prophylaxis in the reduction of fungal infections after liver transplant. Transplant Proc 1992; 24: 154–155.
Fortun J, Martin-Davila P, Moreno S, Barcena R, de Vicente E, Honrubia A, Garcia M, Nuno J, Candela A, Uriarte M, Pintado V: Prevention of invasive fungal infections in liver transplant recipients: the role of prophylaxis with lipid formulations of amphotericin B in high-risk patients. J Antimicrob Chemother 2003; 52: 813–819.
Lorf T, Braun F, Ruchel R, Muller A, Sattler B, Ringe B: Systemic mycoses during prophylactical use of liposomal amphotericin B (Ambisome) after liver transplantation. Mycoses 1999; 42: 47–53.
Biancofiore G, Bindi ML, Baldassarri R, Romanelli AM, Catalano G, Filipponi F, Vagelli A, Mosca F: Antifungal prophylaxis in liver transplant recipients: a randomized placebo-controlled study. Transpl Int 2002; 15: 341–347.
Hamza NS, Ghannoum MA, Lazarus HM: Choices aplenty: antifungal prophylaxis in hematopoietic stem cell transplant recipients. Bone Marrow Transplant 2004; 34: 377–389.
Walsh TJ, Raad I, Patterson TF, Chandrasekar P, Donowitz GR, Graybill R, Greene RE, Hachem R, Hadley S, Herbrecht R, Langston A, Louie A, Ribaud P, Segal BH, Stevens DA, van Burik JA, White CS, Corcoran G, Gogate J, Krishna G, Pedicone L, Hardalo C, Perfect JR: Treatment of invasive aspergillosis with posaconazole in patients who are refractory to or intolerant of conventional therapy: an externally controlled trial. Clin Infect Dis 2007; 44: 2–12.
Ullmann AJ, Lipton JH, Vesole DH, Chandrasekar P, Langston A, Tarantolo SR, Greinix H, Morais de AW, Reddy V, Boparai N, Pedicone L, Patino H, Durrant S: Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med 2007; 356: 335–347.
Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ, Helfgott D, Holowiecki J, Stockelberg D, Goh YT, Petrini M, Hardalo C, Suresh R, ngulo-Gonzalez D: Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med 2007; 356: 348–359.
Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, van Burik JA, Wingard JR, Patterson TF: Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 2008; 46: 327–360.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosenhagen, M., Feldhues, R., Schmidt, J. et al. A Risk Profile for Invasive Aspergillosis in Liver Transplant Recipients. Infection 37, 313–319 (2009). https://doi.org/10.1007/s15010-008-8124-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-008-8124-x