Abstract
Background:
The Hand Hygiene Liaison Group and Epic Projects (Pratt et al., J Hosp Infect 47[Suppl A], 2001) have asked specifically for further trials of educational interventions to improve hand decontamination compliance and infection control in the hospital setting. This study investigates the efficacy of a ‘clean practice protocol’ (CPP), derived from international guidelines, to improve compliance of infection-control practices by surgical teams in a large UK teaching hospital.
Methods:
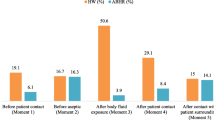
The key infection-control activities were summated to form the CPP presented here. An undisclosed infection-control audit of consultant-led ward-rounds from breast, gastrointestinal, vascular, urological, and intensivecare departments was performed. The audit results were presented to the surgical teams, after which an education/awareness program was implemented. A repeat undisclosed audit was performed 3 months later. In both audits, infection-control activities were recorded together with consultation time and any patient infective complications.
Results:
The surgical teams performed as follows in the initial audit: hand decontamination (28% of consultations), correct use of gloves (2%), instrument cleaning (0%), garment contamination (49%), and notes contamination (34%). Introduction of the CPP education program significantly improved hand decontamination to 87% (p < 0.0001), the correct use of gloves/aprons to 50% (p < 0.0001), and overall infection-control practice from 63% to 89% (p < 0.05).
Conclusions:
The introduction of the CPP significantly improved compliance of hand decontamination, correct usage of gloves and aprons, and overall infection-control in a large teaching hospital. The CPP is a highly effective auditing and educational tool that can be readily adapted for use in hospitals globally to monitor and improve infection-control practices.
Similar content being viewed by others
References
Plowman R, Graves N, Griffin M, Roberts J, Swan T, Cookson B, Taylor L: The socio-economic burden of hospital acquired infection. Public Health Laboratory Service, London 2000. ISBN: 0901144487.
Ducel G, Fabry J, Nicolle L: Prevention of hospital acquired infections. A practical guide (2nd edn). World Health Organisation, Geneva 2002.
House of Lords Select Committee on Science and Technology: Resistance to antibiotics and other antimicrobial agents. HL paper 81-I, 7th report session, 1997–1998. Stationery Office, London 1998.
Hospital Infection Working Group of the Department of Health & Public Health Laboratory Service (PHLS) Hospital infection control: guidance on the control of infection in hospitals. PHLS 1995; 84: 8.
Pratt RJ, Pellowe C, Liveday HP, Robinson N, Smith GW: The EPIC project: developing national evidence-based guidelines for preventing healthcare associated infections. J Hosp Infect 2001; 47 [Suppl A].
Pratt RJ, Pellowe CM, Wilson JA, Loveday HP, Harper P, Jones SRLJ, McDougall C, Wilcox MH: EPIC2: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2007; 65S: S1–S64.
Wilson J: Infection control in clinical practice. Baillière Tindall, London, 1995, pp 161–162.
Stone SP: Hand hygiene — the case for evidence-based education. J R Soc Med 2001; 94: 278–281.
Pittet D, Hugonnet S, Harbarth S, Mourouga S, Sauvan V, Touveneau S, Perneger T: Effectiveness of a hospital wide programme to improve compliance with hand hygiene: infection control programme. Lancet 2000; 356: 1307–1312.
Larson EL, Early E, Cloonan P, Sugrue S, Parides M: An organizational climate intervention associated with increased handwashing and decreased nosocomial infections. Behav Med 2000; 26: 14–22.
Eldridge NE, Woods S, Bonello RS, Clutter K, Ellingson L, Harris M, Livingston B, Bagian J, Danko L, Dunn E, Parlier R, Pederson C, Reichling K, Roselle G, Wright S: Using the six sigma process to implement the centers for disease control and prevention guideline for hand hygiene in 4 intensive care units. J Gen Intern Med 2006; 21: S35–S42.
Teare EL, Cookson B, French G, Jenner EA, Scott G, Pallett A: UK handwashing initiative. J Hosp Infect 1999; 43: 1–3.
National Collaborating Centre for Nursing and Supportive Care: Infection control. Prevention of healthcare-associated infection in primary and community care. NICE guideline. National Institute for Health and Clinical Excellence 2003, June.
Garner JS: The Hospital Infection Control Practices Advisory Committee: guidelines for isolation precautions in hospitals. Infect Control Hosp Epidemiol 1996; 17: 53–80.
Cooper BS, Stone SP, Kibbler CC, Cookson B, Roberts J, Medley F, Duckworth G, Lai R, Ebrahim S: Isolation measures in the hospital management of methicillin resistant Staphylococcus aureus (MRSA): systematic review of the literature. Br Med J 2004; 329: 7533.
Johnston P, Norrish AR, Brammar T, Walton N, Hegarty TA, Coleman NP: Reducing methicillin-resistant Staphylococcus aureus (MRSA) patient exposure by infection control measures. Ann R Coll Surg Engl 2005; 87: 123–125.
Bebbington A, Parkin I, James PA, Chichester LJ, Kubiak EM: Patients’ case-notes: look but don’t touch. J Hosp Infect 2003; 55: 299–301.
Jones JS, Hoerle D, Riekse R: Stethoscopes: a potential vector of infection? Ann Emerg Med 1995; 26: 296–299.
Parmar RC, Valvi CC, Sira P, Kamat JR: A prospective, randomised, double-blind study of comparative efficacy of immediate versus daily cleaning of stethoscope using 66% ethyl alcohol. Indian J Med Sci 2004; 58: 423–430.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Howard, D.P.J., Williams, C., Sen, S. et al. A Simple Effective Clean Practice Protocol Significantly Improves Hand Decontamination and Infection Control Measures in the Acute Surgical Setting. Infection 37, 34–38 (2009). https://doi.org/10.1007/s15010-008-8005-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-008-8005-3