Abstract
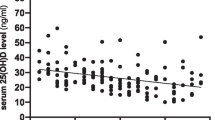
Antiepileptic drugs (AED) have potential side effects through vitamin-D. Prevalence of vitamin D insufficiency and potential risk factors for the longitudinal changes of vitamin D levels compared to its baseline levels under AED treatment were investigated in this study. This retrospective study includes patients whose AED therapy were started in only autumn months, between 2000 and 2014. Detailed assessment of neurologic diagnosis and brain MRI findings, ambulatory status, types and durations of AED treatment, and baseline bone health blood tests (vitamin-D, alkaline phosphatase, calcium, and phosphate levels) were obtained on all patients. Vitamin-D deficiency was defined as 25(OH)D <20 ng/mL, while vitamin-D insufficiency was defined as 25(OH)D between 21 and 29 ng/mL. A total of 172 children (mean age 9.6 ± 4.3 years) were followed up 5.3 years in average (range 1–14.7). The mean baseline 25(OH)D level was decreased from 24.4 ± 11.6 to 19.6 ± 10.7 ng/mL at the last follow up. The mean change in the vitamin-D levels (ΔD-vitamin) was −4.8 ng/mL (p = 0.003). The rate of vitamin-D deficiency was 54% and insufficiency was 25%. Multivariate logistic regression analysis identified only long-term use of AEDs as a risk factor for the longitudinal decrease. Monotherapy with valproic acid (n = 45), carbamazepine (n = 20), levetiracetam (n = 10) and phenobarbital (n = 12) was compared with each other. There was no difference in terms of longitudinal changes in 25(OH)D levels. In the treatment of childhood epilepsy, 25(OH)D levels should be monitored, especially when long-term AED used, in order to prevent D-hypovitaminosis.

Similar content being viewed by others
References
Wacker M, Holick MF (2013) Vitamin D effects of skeletal and extraskeletal health and the need for supplementation. Nutrients 5:111–148
Saggese G, Vierucci F, Boot AM, Czech-Kowalska J, Weber G, Camargo CA Jr et al (2015) Vitamin D in childhood and adolescence: an expert position statement. Eur J Pediatr 174:565–576
Shellhaas RA, Joshi SM (2010) Vitamin D and bone health among children with epilepsy. Pediatr Neurol 42:385–393
Medicines and Healthcare products Regulatory Agency (MHRA), Commission on Human Medicines (CHM (2009) Drug safety advice antiepileptics: adverse effects on bone. Drug Saf Update. 2:2
Cebeci AN, Ekici B (2014) Epilepsy treatment by sacrificing vitamin D. Expert Rev Neurother 14:481–491
Harijan P, Khan A, Hussain N (2013) Vitamin D deficiency in children with epilepsy: do we need to detect and treat it? J Pediatr Neurosci. 8:5–10
Shevell M, Ashwal S, Donley D, Flint J, Gingold M, Hirtz D, Majnemer A, Noetzel M, Sheth RD (2003) Quality Standards Subcommittee of the American Academy of N, Practice Committee of the Child Neurology S. Practice parameter: evaluation of the child with global developmental delay: report of the Quality Standards Subcommittee of the American Academy of Neurology and The Practice Committee of the Child Neurology Society. Neurology. 60:367–380
Erol M, Yiğit Ö, Küçük SH, Bostan Gayret Ö (2015) Vitamin D Deficiency in Children and Adolescents in Bağcılar, Istanbul. J Clin Res Pediatr Endocrinol. 7(2):134–139
Adams JS, Hewison M (2010) Update in vitamin D. J Clin Endocrinol Metab 95:471–478
Bergqvist AG, Schall JI, Stallings VA (2007) Vitamin D status in children with intractable epilepsy, and impact of the ketogenic diet. Epilepsia 48:66–71
Souverein PC, Webb DJ, Weil JG, Van Staa TP, Egberts AC (2006) Use of antiepileptic drugs and risk of fractures: case–control study among patients with epilepsy. Neurology 66:1318–1324
Baek JH, Seo YH, Kim GH, Kim MK, Eun BL (2014) Vitamin D levels in children and adolescents with antiepileptic drug treatment. Yonsei Med J 55:417–421
Lee YJ, Park KM, Kim YM, Yeon GM, Nam SO (2015) Longitudinal change of vitamin D status in children with epilepsy on antiepileptic drugs: prevalence and risk factors. Pediatr Neurol 52:153–159
Nettekoven S, Strohle A, Trunz B, Wolters M, Hoffmann S, Horn R et al (2008) Effects of antiepileptic drug therapy on vitamin D status and biochemical markers of bone turnover in children with epilepsy. Eur J Pediatr 167:1369–1377
El-Hajj Fuleihan G, Dib L, Yamout B, Sawaya R, Mikati MA (2008) Predictors of bone density in ambulatory patients on antiepileptic drugs. Bone 43:149–155
Bell RD, Pak CY, Zerwekh J, Barilla DE, Vasko M (1979) Effect of phenytoin on bone and vitamin D metabolism. Ann Neurol 5:374–378
Mintzer S, Boppana P, Toguri J, DeSantis A (2006) Vitamin D levels and bone turnover in epilepsy patients taking carbamazepine or oxcarbazepine. Epilepsia 47:510–515
Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M (2008) Drug, Therapeutics Committee of the Lawson Wilkins Pediatric Endocrine S. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics 122:398–417
Cansu A, Yesilkaya E, Serdaroglu A, Hirfanoglu TL, Camurdan O, Gulbahar O et al (2008) Evaluation of bone turnover in epileptic children using oxcarbazepine. Pediatr Neurol 39:266–271
Vanlint S, Nugent M, Durvasula S (2008) Vitamin D and people with intellectual disability. Aust Fam Phys 37:348–351
Babayigit A, Dirik E, Bober E, Cakmakci H (2006) Adverse effects of antiepileptic drugs on bone mineral density. Pediatr Neurol 35:177–181
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yildiz, E.P., Poyrazoglu, Ş., Bektas, G. et al. Potential risk factors for vitamin D levels in medium- and long-term use of antiepileptic drugs in childhood. Acta Neurol Belg 117, 447–453 (2017). https://doi.org/10.1007/s13760-017-0775-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-017-0775-x