Abstract
Tapia’s syndrome is characterized by unilateral paralysis of the tongue and vocal cord, and is caused by a concurrent lesion of both the recurrent laryngeal and hypoglossal nerves. The proposed mechanism in most patients is compression or stretching of these nerves on their extracranial course due to airway manipulation under general anaesthesia. As Tapia’s syndrome is a rare and possibly devastating condition, recognition of the presence of concurrent paralyses is an important step in diagnosis and treatment. We report two cases of Tapia’s syndrome as a complication of intubation in the intensive care unit.
Similar content being viewed by others
Introduction
Tapia’s syndrome is a rare entity characterized by the association of unilateral tongue and vocal cord paralysis with normal soft palate function. In 1904, the Spanish otolaryngologist Antonia Garcia Tapia reported the first case of a bullfighter with an ipsilateral hemiplegia of the larynx and tongue after a neck wound from a bull’s horn (‘matador’s disease’) [1]. The eponym includes two distinct conditions. The central Tapia’s syndrome is a crossed brainstem syndrome caused by a lesion of the nucleus ambiguous, the nucleus of the hypoglossal nerve and the pyramidal tract. The peripheral Tapia’s syndrome is caused by an extracranial lesion at the crossing point of the hypoglossal nerve and recurrent laryngeal branch of the vagal nerve below the ganglion nodosum [2]. The latter explains the sparing of soft palate and pharynx motility, as the pharyngeal branch emerges more cranially. The clinical symptoms due to ipsilateral paralysis of the vocal cord and tongue include hoarseness, dysphagia due to tongue incoordination and food bolus propulsion. The clinical signs include unilateral deviation of the tongue toward the denervated side with atrophy of the tongue, as well as vocal cord paresis or paralysis visualized on endoscopy. In contrast to the traumatic cause described in the original case, most of the reports in literature are ascribed to airway manipulation under general anaesthesia [3]. However, other causes have been published in recent years.
Case report 1
A 64-year-old man was admitted to the psychiatry department because of self-neglect, confusion and relapse of alcohol abuse. His past medical history included alcohol abuse, liver cirrhosis and alcoholic pancreatitis. He was transferred to the intensive care unit (ICU) on the 4th day of admission because of respiratory failure due to pneumonia. Empirical antibiotic treatment was started, but later switched to piperacillin with tazobactam combined with systemic corticosteroids because of suspected aspiration pneumonia with acute respiratory distress syndrome (ARDS). An uncomplicated endotracheal intubation (ETI) [4] was performed at the ICU where he developed atrial fibrillation with hemodynamic instability and ascites because of decompensated liver cirrhosis. The endotracheal tube could be removed 15 days later. Because of poor cooperation and confusion, extensive swallow testing could only be carried out 8 days after extubation. He was fed by a nasogastral tube. At formal testing, hoarseness and dysphagia was detected. Laryngoscopic examination was initially difficult to interpret, because of massive stasis of saliva. Eventually, a percutaneous endoscopic gastrostomy tube was placed because of the high risk for aspiration. Forty days after extubation, laryngoscopic examination revealed a left vocal cord paralysis. Neurological examination showed deviation of the tongue to the left without atrophy and mild uvula distortion to the right. Further diagnostic work up for combined CNX and CNXII paralyses was performed. Imaging of the brain (magnetic resonance imaging, MRI), carotid and vertebral arteries, and skull base (computed tomography, CT) showed no abnormalities. A lumbar puncture, a PET scan of the brain and a chest-CT were normal. CT of the neck showed atrophy of the oropharynx with fatty degeneration of the tongue base.
A unilateral pressure neuropathy was suspected, due to traumatic tracheal intubation and pressure of the cuff. Speech and swallow therapy was further implemented. A reevaluation 3 months later showed no clear improvement, despite better phonation and less hoarseness. After 13 months, tongue mobility was recovered with a normal swallowing act. The PEG tube could be removed. Furthermore, his voice was clearer, despite a residual left vocal cord paralysis on laryngoscopic examination. After 22 months, recovery was complete.
Case report 2
A 49-year-old patient with a history of myocardial infarction and percutaneous coronary intervention was admitted to the hospital due to ventricular tachycardia. In the coronary care unit, there was a fast evolution to ventricular fibrillation and asystolia with emergency cardiopulmonary resuscitation and defibrillation. After antiarrhythmic drugs were given, a stable sinus rhythm was eventually obtained. Ablation was performed, and finally a DDD-ICD pacemaker was placed. During his stay in the intensive care unit, endotracheal intubation was performed twice. After 11 days, an attempt to extubation was performed. Exhaustion and stridor because of ventilator associated pneumonia made this attempt impossible; a new intubation procedure was performed without complications [4]. After 2 days, a new attempt to extubation was successful. He complained of hoarseness and swallowing problems with sialorrhea. Neurological examination showed an absent gag reflex and paralysis of tongue musculature without deviation. There was hoarseness of the voice. Examination of the other cranial nerves was normal. There was no sensorimotor abnormality of the four limbs and coordination reflexes were normal. Bilateral vocal cord paralysis was seen during laryngoscopy.
Brain-CT and CT angiography showed no abnormalities of the carotid arteries or brain stem region. Unfortunately, MRI of the brain was not possible because of the presence of a pacemaker.
A bilateral pressure neuropathy was suspected due to traumatic tracheal intubation and pressure of the cuff. Percutaneous endoscopic gastrostomy tube was placed, and speech and swallowing therapy was started. A treatment with corticosteroids was started, at a dose of 48 mg prednisolone daily with a slow reduction schedule for 8 weeks. After 1 month, a reevaluation showed no improvement. Two months later, phonation was better, tongue mobility was stronger, and after 4 months, total recovery took place.
Discussion
We report two cases of peripheral Tapia’s syndrome with a suspected pressure neuropathy of the cranial nerves, probably due to traumatic tracheal intubation.
Reports of a central Tapia’s syndrome are sparse. Only three cases of medial or mediolateral medullary infarction with the classic clinical features of central Tapia’s syndrome have been reported; two of these patients had brainstem infarctions and one had meningovascular syphilis [5–7]. Another case has been attributed to a metastatic hemangiosarcoma in the medulla oblongata [8].
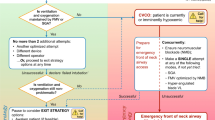
Most cases of peripheral Tapia’s syndrome have been encountered by anaesthesiologists, surgeons or otorhinolaryngologists. One of the hypothesized etiological mechanisms is a pressure neuropathy, caused by malpositioning of the orotracheal tube during surgery or respiratory support in intensive care settings [2]. Depending on the extent and duration of the injury, the nerve function may be temporarily impaired due to stretching (neuropraxia) or the nerve may be permanently damaged (neurotmesis). The use of a concurrent throat pack, pressure from airway instrumentation or cuff overinflation may worsen the condition [2, 3]. The lateral wall of the lower part of the oropharynx (tongue base) and the upper part of the hypopharynx (pyriform fossa), where RLN and vagus nerve (CNX) are in close proximity, are the anatomical sites where local pressure may arise [2]. Another anatomical location is the lateral prominence of the transverse process of the first cervical vertebra, where the hypoglossal nerve crosses the CNX [9]. Neck hyperextension during endotracheal tube placing or during surgeries, which require manipulation of the patient’s head, can cause stretching of these nerves against the vertebra [2, 9]. Examples of the latter are the reported cases following (septo-rhinoplasties [2, 10–14], cervical spine [15–18] and cardiac surgery [9, 19–21]). Other causes reported in literature are summarized in Table 1 [1, 22–33]. Only one case following airway intubation because of pneumonia and ARDS has been reported [34] (see Table 2).
Tables 1 and 2 provide an overview of all reported cases of Tapia’s syndrome following intubation during surgery or respiratory support. The neurological deficit is usually unilateral, but scarce reports on bilateral involvement are also available [13, 19, 20], as was the case in our second patient. Aktas and Boga proposed a classification scheme for Tapia syndrome, ranging from grade I (mild type) to grade III (severe type) with additional therapeutic recommendations, although not based on evidence from clinical trials [11].
Treatment of peripheral Tapia’s syndrome following intubation is mainly supportive. Speech and language therapy including swallowing rehabilitation play a key role. In the acute setting, administration of intravenous or oral steroids for 10–14 days has been advocated. Some physicians recommend the additional use of vitamins (B1, B6, B12 or combinations) for up to 3 months [3]. These medical treatments are not supported by clear scientific evidence. Furthermore, data on predicting factors for clinical outcome are currently lacking.
Tapia’s syndrome is not a benign condition. It can cause severe morbidity and it is not always reversible. Thirty-seven percent of cases (7 of 19) attributed to endotracheal intubation for surgery recovered incompletely or not at all [3, 14–16, 19, 21, 31, 34, 35]. In four reported cases with incomplete recovery, there was residual hypoglossal nerve palsy [14, 16, 19, 31]. However, the mean follow-up period reported for these four cases was only 8 months. Two cases showed no recovery at all, one 12 months after thoracotomy, the other 3 years after liposuction [3, 21].
Only very limited data on Tapia’s syndrome in patients requiring respiratory support are available. We add two new cases with this problem. The only reported case concerns a 15-year-old patient with pneumonia and ARDS. He had a bilateral Tapia’s syndrome (left RLN and bilateral CN XII paresis), which recovered incompletely with residual RLN paresis, although the follow-up period probably was too short to make a conclusion [33]. One of our cases showed a complete recovery after 4 months, the other one recovered after a period of 22 months. Considering the extended time of endotracheal intubation and hence possible neuropraxis in case of respiratory support, the recovery phase can be longer in this setting. We stress the importance of a long-term follow-up and supportive treatment in Tapia’s syndrome as recovery still may occur more than 1 year after symptom-onset like in one of our cases. Furthermore, an important part of cases of Tapia's syndrome are iatrogenic, so it is of utmost importance to be aware of the possibility of cranial nerve injury due to airway manipulation as well as head and neck repositioning during surgery or respiratory support in the intensive care unit. Preventive measures should focus on safely securing the endotracheal tube, avoiding cuff overinflation and positioning of the throat pack causing excessive pressure on the pharynx [35].
Conclusion
Tapia’s syndrome can be a complication of endotracheal intubation in the setting of respiratory support in the intensive care unit. Preventive measures should be taken into account to minimize the chance of occurrence. It is important to make a timely diagnosis so treatment and rehabilitation can be started early to achieve a good long-term outcome.
References
Schoenberg BS, Massey EW (1979) Tapia’s syndrome. The erratic evolution of an eponym. Arch Neurol 36:257–260
Lykoudis EG, Seretis K (2012) Tapia’s syndrome: an unexpected but real complication of rhinoplasty: case report and literature review. Aesth Plast Surg 36:557–559
Gevorgyan A, Nedzelski M (2013) A late recognition of Tapia syndrome: a case report and literature review. Laryngoscope 123:2423–2427
Divatia J, Bhowmick K (2005) Complications of endotracheal intubation and other airway management procedures. Indian J Anaesth 49:308–318
Bogousslavsky J, Fox AJ, Barnett HJ et al (1986) Clinico-topographic correlation of small vertebrobasilar infarct using magnetic resonance imaging. Stroke 17:929–938
Terao S, Izumi M, Takatsu S et al (1998) Serial magnetic resonance imaging shows separate medial and lateral medullary infarctions resulting in the hemimedullary syndrome. J Neurol Neurosrug Psychiatry 65:134–141
Tyler KL, Sandberg E, Baum KF (1994) Medial medullary syndrome and meningovascular syphilis: a case report in an HIV-infected man and a review of literature. Neurology 44:134–141
Krasnianski M, Neudecker S, Schluter A et al (2003) Central Tapia’s syndrome (“matador’s disease”) caused by metastatic hemangiosarcoma. Neurology 61:868–869
Nalladaru Z, Wessels A, DuPreez L (2012) Tapia’s syndrome—a rare complication following cardiac surgery. Interact CardioVasc Thorac Surg 14:131–132
Ghorbani J, Dabir S, Givehchi G, Najafi M (2014) Co-presentation of Tapia’s syndrome en pressure alopecia—a rare event after septorhinoplasty: a case report and literature review. Acta Anaesthesiol Taiwan 52:38–40
Boga I, Aktas S (2010) Treatment, classification and review of Tapia syndrome. J Craniofac Surg 21:278–280
Tesei F, Poveda LM, Strali W, Tosi L, Farneti G (2006) Unilateral laryngeal and hypoglossal paralysis (Tapia’s syndrome) following rhinoplasty in general anaesthesia: case report and review of literature. Acta Otorhinolaryngol Ital 26:219–221
Cinar SO, Seven H, Cinar U, Turgut S (2005) Isolated bilateral paralysis of the hypoglossal and recurrent laryngeal nerves (bilateral Tapia’s syndrome) after transoral intubation for general anesthesia. Acta Anaesthesiol Scand 49:98–99
Yavuzer R, Basterzi Y, Ozkose Z, Yucel Demir H, Yilmaz M, Ceylan A (2004) Tapia’s syndrome following septorhinoplasty. Aesthetic Plast Surg 28:208–211
Kang JH, Kim DM, Kim SW (2013) Tapia syndrome after cervical spine surgery.Korean J. Spine 10:249–251
Park J, Ahn R, Weon Y, Yang D (2011) Diagnosing Tapia syndrome using a videofluoroscopic swallowing study and electromyography after anterior cervical spine surgery. Am J Phys Med Rehabil 90:948–953
Lim K, Kim M, Kang M, Lee H et al (2013) Tapia’s syndrome following cervical laminoplasty. Korean J Anesthesiol 64:172–174
Park CK, Lee DC, Park CJ, Hwang JH (2013) Tapia’s syndrome after posterior cervical spine surgery under general anesthesia. J Korean Neurosurg Soc 54:423–425
Rotondo F, De Paulis S, Modoni A, Schiavello R (2010) Peripheral Tapia’s syndrome after cardiac surgery. Eur J Anaesthesiol 27:575–576
Sotiriou K, Balanika M, Anagnostopoulou S et al (2007) Postoperative airway obstruction due to Tapia’s syndrome after coronary bypass grafting surgery. Eur J Anaesthesiol 24:378–379
Gelmers HJ (1983) Tapia’s syndrome after thoracotomy. Arch Otolaryngol 109:622–623
McCleary AJ (1993) A fracture of the odontoid process complicated by tenth and twelfth cranial nerve palsies. A case report. Spine 18:932–935
Cantalupo G, Spagnoli C, Cerasti D, Piccolo B, Crisi G, Pisani F (2014) Tapia’s syndrome secondary to laterocervical localization of diffuse large cell lymphoma. Brain Dev 36:548–550
Quattrocolo G, Giobbe D, Baggiore P (1986) Tapia’s syndrome caused by a neurilemmoma of vagus and hypoglossal nerves in the neck. Acta Neurol (Napoli) 8:535–540
Andriolo G, Rigobello L, Mingrino S, Toso V (1980) Tapia’s syndrome caused by neurofibroma of the hypoglossal and vagus nerves: case report. J Neurosurg 52:730–732
Lo Casto A, Spataro R, Purpura P, La Bella V (2013) Unilateral laryngeal and hypoglossal paralysis (Tapia’s syndrome) in a patient with an inflammatory pseudotumor of the neck. Clin Neurol Neurosurg 115:1499–1501
De Freitas MR, Nascimento OJ, Chimelli L (1991) Tapia’s syndrome caused by Paracoccidioidis brasiliensis. J Neurol Sci 103:179–181
Takimoto T, Saito Y, Suzuki M, Nishimura T (1991) Radiation-induced cranial nerve palsy: hypoglossal nerve and vocal cord palsies. J Laryngol Otol 105:44–45
Johnson TM, Moore HJ (1999) Cranial nerve X and XII paralysis (Tapia’s syndrome) after an interscalene brachial plexus block for a left shoulder Mumford procedure. Anesthesiology 90:311–312
Al-Sihan M, Schumacher M, Lohle E (2011) Tapia syndrome caused by a vertebral artery dissection. Ear Nose Throat J 90:313–314
Kashyap SA, Patterson AR, Loukota RA, Kelly G (2010) Tapia’s syndrome after repair of a fractured mandible. Br J Oral Maxillofac Surg 48:53–54
Boisseau N, Rabarijaona H, Grimaud D, Raucoules-Aime M (2002) Tapia’s syndrome following shoulder surgery. Br J Anaesth 88:869–870
Turan I, Yildirim ZK, Tan H (2012) Bilateral Tapia syndrome secondary to oropharyngeal intubation. J Neurosurg Anesthesiol 24:78
Mayer A, Opran H (1974) Tapia syndrome. JAMA 227:326
Varedi P, Shirani G, Karimi A et al (2013) Tapia syndrome after repairing a fractured zygomatic complex: a case report and review of the literature. J Oral Maxillofac Surg 71:1665–1669
Conflicts of interest
None.
Ethical standard
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of report formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coninckx, M., Cardoen, S. & Hemelsoet, D. Tapia’s syndrome in the intensive care unit: a rare cause of combined cranial nerve palsy following intubation. Acta Neurol Belg 115, 533–537 (2015). https://doi.org/10.1007/s13760-015-0500-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-015-0500-6