Abstract
Purpose of Review
This paper will review the intestinal and gastric origins for diabetes resolution after bariatric surgery.
Recent Findings
In addition to the known metabolic effects of changes in the gut hormonal milieu, more recent studies investigating the role of the microbiome and bile acids and changes in nutrient sensing mechanisms have been shown to have glycemic effects in human and animal models.
Summary
Independent of weight loss, there are multiple mechanisms that may lead to amelioration or resolution of diabetes following bariatric surgery. There is abundant evidence pointing to changes in gut hormones, bile acids, gut microbiome, and intestinal nutrient sensing; more research is needed to clearly delineate their role in regulating energy and glucose homeostasis after bariatric surgery.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Diabetes. In: World Health Organization. http://www.who.int/mediacentre/factsheets/fs312/en/. Accessed 6 Dec 2017.
International Diabetes Federation. IDF Diabetes Atlas. 7th ed. Available from http://www.diabetesatlas.org. Accessed 20 February 2016.
Obesity and overweight. In: World Health Organization. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 6 Dec 2017.
Overweight & Obesity. In: Centers for Disease Control and Prevention, www.cdc.gov/obesity/data/adult.html. Accessed 29 Aug 2017.
Bariatric Surgery Procedures – ASMBS. In: American Society for Metabolic and Bariatric Surgery. https://asmbs.org/patients/bariatric-surgery-procedures. Accessed 5 Dec 2017.
Buse JB, Caprio S, Cefalu WT, Ceriello A, Del Prato S, Inzucchi SE, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5. https://doi.org/10.2337/dc09-9036.
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Surg Obes Relat Dis. 2009;5:409. https://doi.org/10.1016/j.soard.2009.04.006.
Purnell JQ, Selzer F, Wahed AS, Pender J, Pories W, Pomp A, et al. Type 2 diabetes remission rates after laparoscopic gastric bypass and gastric banding: results of the longitudinal assessment of bariatric surgery study. Diabetes Care. 2016;39:1101–7.
Pournaras DJ, Aasheim ET, Søvik TT, Andrews R, Mahon D, Welbourn R, et al. Effect of the definition of type II diabetes remission in the evaluation of bariatric surgery for metabolic disorders. Br J Surg. 2011;99:100–3. https://doi.org/10.1002/bjs.7704.
Adams TD, Davidson LE, Litwin SE, Kim J, Kolotkin RL, Nanjee MN, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55. https://doi.org/10.1056/nejmoa1700459.
Rubino F, Schauer PR, Kaplan LM, Cummings DE. Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanisms of action. Annu Rev Med. 2010;61:393–411.
Pories WJ, MacDonald KG, Flickinger EG, Dohm GL, Sinha MK, Barakat HA, et al. Is type II diabetes mellitus (NIDDM) a surgical disease? Ann Surg. 1992;215(6):633–43.
• Laferrere B, Heshka S, Wang K, Khan Y, Mcginty J, Teixeira J, et al. Incretin levels and effect are markedly enhanced 1 month after Roux-en-Y gastric bypass surgery in obese patients with type 2 diabetes. Diabetes Care. 2007;30:1709–16. https://doi.org/10.2337/dc06-1549. This study demonstrates that the early effects of gastric bypass on glucose metabolism are partly weight independent and mediated by an increased incretin effect.
Holter MM, Dutia R, Stano SM, Prigeon RL, Homel P, Mcginty JJ, et al. Glucose metabolism after gastric banding and gastric bypass in individuals with type 2 diabetes: weight loss effect. Diabetes Care. 2016;40:7–15. https://doi.org/10.2337/dc16-1376.
Korner J, Bessler M, Cirilo LJ, Conwell IM, Daud A, restuccia NL, et al. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab. 2005:90:359–365 Doi:10.1210.
Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011;54(10):2506–14. https://doi.org/10.1007/s00125-011-2204-7.
Jackness C, Karmally W, Febres G, Conwell IM, Ahmed L, Bessler M, et al. Very low-calorie diet mimics the early beneficial effect of Roux-en-Y gastric bypass on insulin sensitivity and β-cell function in type 2 diabetic patients. Diabetes. 2013;62:3027–32. https://doi.org/10.2337/db12-1762.
Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes. 2001;50:1714–9. https://doi.org/10.2337/diabetes.50.8.1714.
Sumithran P, Prendergast LA, Delbridge E, Purcell K, Shulkes A, Kriketos A, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365(17):1597–604. https://doi.org/10.1056/NEJMoa1105816.
• Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623–30. A seminal paper demonstrating that the increase in the plasma ghrelin levels observed with diet-induced weight loss is not seen after gastric bypass surgery-induced weight loss.
Bose M, Oliván B, Teixeira J, Pi-Sunyer FX, Laferrère B. Do incretins play a role in the remission of type 2 diabetes after gastric bypass surgery: what are the evidence? Obes Surg. 2008;19:217–29.
Thaler JP, Cummings DE. Minireview: hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocr Rev. 2009;30:409.
Ybarra J, Bobbioni-Harsch E, Chassot G, Huber O, Morel P, Assimacopoulos-Jeannet F, et al. Persistent correlation of ghrelin plasma levels with body mass index both in stable weight conditions and during gastric-bypass-induced weight loss. Obes Surg. 2008;19:327–33.
Yousseif A, Emmanuel J, Karra E, Millet Q, Elkalaawy M, Jenkinson AD, et al. Differential effects of laparoscopic sleeve gastrectomy and laparoscopic gastric bypass on appetite, circulating acyl-ghrelin, peptide YY3-36 and active GLP-1 levels in non-diabetic humans. Obes Surg. 2013;24:241–52. https://doi.org/10.1007/s11695-013-1066-0.
Patel RT, Shukla AP, Ahn SM, Moreira M, Rubino F. Surgical control of obesity and diabetes: the role of intestinal vs. gastric mechanisms in the regulation of body weight and glucose homeostasis. Obesity. 2013;22:159–69. https://doi.org/10.1002/oby.20441.
Woods SC, D’Alessio DA. Central control of body weight and appetite. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):S37–50. https://doi.org/10.1210/jc.2008-1630.
Boey D, Lin S, Enriquez RF, Lee NJ, Slack K, Couzens M, et al. PYY transgenic mice are protected against diet-induced and genetic obesity. Neuropeptides. 2008;42:19–30. https://doi.org/10.1016/j.npep.2007.11.003.
Boey D, Lin S, Karl T, Baldock P, Lee N, Enriquez R, et al. Peptide YY ablation in mice leads to the development of hyperinsulinaemia and obesity. Diabetologia. 2006;49:1360–70. https://doi.org/10.1007/s00125-006-0237-0.
Karamanakos SN, Vagenas K, Kalfarentzos F, Alexandrides TK. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy. Ann Surg. 2008;247:401–7. https://doi.org/10.1097/sla.0b013e318156f012.
Valderas JP, Irribarra V, Boza C, de la Cruz R, Liberona Y, Acosta AM, et al. Medical and surgical treatments for obesity have opposite effects on peptide YY and appetite: a prospective study controlled for weight loss. J Clin Endocrinol Metab. 2010;95(3):1069–75. https://doi.org/10.1210/jc.2009-0983.
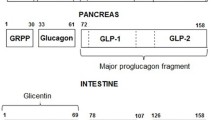
Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409–39.
Jirapinyo P, Jin DX, Qazi T, Mishra N, Thompson CCA. Meta-analysis of GLP-1 after Roux-en-Y gastric bypass: impact of surgical technique and measurement strategy. Obes Surg. 2017 Sep 5; https://doi.org/10.1007/s11695-017-291.
Rubino F, Forgione A, Cummings DE, Vix M, Gnuli D, Mingrone G, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244:741–9.
Ramzy AR, Nausheen S, Chelikani PK. Ileal transposition surgery produces Ileal length-dependent changes in food intake, body weight, gut hormones and glucose metabolism in rats. Int J Obes. 2013;38(3):379–87. https://doi.org/10.1038/ijo.2013.201.
Kindel TL, Yoder SM, Seeley RJ, D’Alessio DA, Tso P. Duodenal-jejunal exclusion improves glucose tolerance in the diabetic, Goto-Kakizaki rat by a GLP-1 receptor-mediated mechanism. J Gastrointest Surg. 2009;13:1762–72. https://doi.org/10.1007/s11605-009-0912-9.
Chambers AP, Jessen L, Ryan K, Sisley S, Wilson-Pérez HE, Stefater MA, et al. Weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterology. 2011;141(3):950–8. https://doi.org/10.1053/j.gastro.2011.05.050.
Ye J, Hao Z, Mumphrey MB, Townsend RL, Patterson LM, Stylopoulos N, et al. GLP-1 receptor signaling is not required for reduced body weight after RYGB in rodents. AJP Regul Integ Comp Physiol. 2014;306(5):R352–62. https://doi.org/10.1152/ajpregu.00491.2013.
Wilson-Pérez HE, Chambers AP, Ryan KK, Li B, Sandoval DA, Stoffers D, et al. Vertical sleeve gastrectomy is effective in two genetic mouse models of glucagon-like peptide 1 receptor deficiency. Diabetes. 2013;62(7):2380–5. https://doi.org/10.2337/db12-1498.
Lindqvist A, Spegel P, Ekelund M, Garcia Vaz E, Pierzynowski, Gomez MF, et al. Gastric bypass improves Î2-cell function and increases Î2-cell mass in a porcine model. Diabetes. 2014;63(5):1665–71. https://doi.org/10.2337/db13-0969.
Jorgensen NB, et al. Exaggerated glucagon-like peptide 1 response is important for improved β-cell function and glucose tolerance after Roux-En-Y gastric bypass in patients with type 2 diabetes. Diabetes. 2014;63(5):1665–71. https://doi.org/10.2337/db13-0969.
Meier JJ, Butler AE, Galasso R, Butler PC. Hyperinsulinemic hypoglycemia after gastric bypass surgery is not accompanied by islet hyperplasia or increased β-cell turnover. Diabetes Care. 2006;29:1554–9. https://doi.org/10.2337/dc06-0392.
Batterham RL, Cummings DE. Mechanisms of diabetes improvement following bariatric/metabolic surgery. Diabetes Care. 2016;39(6):893–901. https://doi.org/10.2337/dc16-0145.
Aguirre V, Stylopoulos N, Grinbaum R, Kaplan LM. An endoluminal sleeve induces substantial weight loss and normalizes glucose homeostasis in rats with diet-induced obesity. Obesity. 2008;16:2585–92.
Kindel TL, Martins PJ, Yoder SM, Jandacek RJ, Seeley RJ, Dalessio DA, et al. Bypassing the duodenum does not improve insulin resistance associated with diet-induced obesity in rodents. Obesity. 2010;19:380–7.
Rohde U, Hedbäck N, Gluud LL, Vilsbøll T, Knop FK. Effect of the EndoBarrier gastrointestinal liner on obesity and type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2016;18:300–5.
Prawitt J, Caron S, Staels B. Bile acid metabolism and the pathogenesis of type 2 diabetes. Curr Diabet Rep. 2011;11:160–6.
Tomkin GH, Owens D. Obesity diabetes and the role of bile acids in metabolism. J Transl Intern Med. 2016;4(2):73–80. https://doi.org/10.1515/jtim-2016-0018.
Kaska L, Sledzinski T, Chomiczewska A, Dettlaff-Pokora A, Swierczynski J. Improved glucose metabolism following bariatric surgery is associated with increased circulating bile acid concentrations and remodeling of the gut microbiome. World J Gastroenterol. 2016;22:8698–719.
Dutia R, Embrey M, O’Brien CS, Haeusler RA, Agénor KK, Homel P, et al. Temporal changes in bile acid levels and 12α-hydroxylation after Roux-en-Y gastric bypass surgery in type 2 diabetes. Int J Obes. 2015;39:806–13.
Fiorucci S, Cipriani S, Baldelli F, Mencarelli A. Bile acid-activated receptors in the treatment of dyslipidemia and related disorders. Prog Lipid Res. 2010;49:171–85.
Kuipers F, Groen AK. FXR: the key to benefits in bariatric surgery? Nat Med. 2014;20:337–8.
Zhang F, Yu L, Lin X, Cheng P, He L, Li X, et al. Minireview: roles of fibroblast growth factors 19 and 21 in metabolic regulation and chronic diseases. Mol Endocrinol. 2015;29:1400–13.
Raghow R. Ménage-à-trois of bariatric surgery, bile acids and the gut microbiome. World J Diabetes. 2015;6:367–70.
Fiorucci S, Distrutti E. Bile acid-activated receptors, intestinal microbiota, and the treatment of metabolic disorders. Trends Mol Med. 2015;21:702–14.
Kohli R, Bradley D, Setchell KD, Eagon JC, Abumrad N, Klein S. Weight loss induced by Roux-en-Y gastric bypass but not laparoscopic adjustable gastric banding increases circulating bile acids. J Clin Endocrinol Metab. 2013;98:E708–12.
Parker HE, Wallis K, le Roux CW, Wong KY, Reimann F, Gribble FM. Molecular mechanisms underlying bile acid-stimulated glucagon-like peptide-1 secretion. Br J Pharmacol. 2012;165:414–23.
Nakatani H, Kasama K, Oshiro T, Watanabe M, Hirose H, Itoh H. Serum bile acid along with plasma incretins and serum high-molecular weight adiponectin levels are increased after bariatric surgery. Metabolism. 2009;58:1400–7.
Steinert RE, Peterli R, Keller S, Meyer-Gerspach AC, Drewe J, Peters T, et al. Bile acids and gut peptide secretion after bariatric surgery: a 1-year prospective randomized pilot trial. Obesity (Silver Spring). 2013;21:E660–8.
Belgaumkar AP, Vincent RP, Carswell KA, Hughes RD, Alaghband-Zadeh J, Mitry RR, et al. Changes in bile acid profile after laparoscopic sleeve gastrectomy are associated with improvements in metabolic profile and fatty liver disease. Obes Surg. 2016;26:1195–202.
Parekh PJ, Balart LA, Johnson DA. The influence of the gut microbiome on obesity, metabolic syndrome and gastrointestinal disease. Clin Transl Gastroenterol. 2015;6(6):e91. https://doi.org/10.1038/ctg.2015.16.
Backhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Scie. 2004;101:15718–23.
Nieuwdorp M, Gilijamse PW, Pai N, Kaplan LM. Role of the microbiome in energy regulation and metabolism. Gastroenterology. 2014;146:1525–33.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–131.
Vrieze A, Van Nood E, Holleman F, Salojarvi J, Kootte RS, Bartelsman JF, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143(4):913–6. https://doi.org/10.1053/j.gastro.2012.06.031.
Perry RJ, Peng L, Barry NA, Cline GW, Zhang D, Cardone RL, et al. Acetate mediates a microbiome–brain–β-cell axis to promote metabolic syndrome. Nature. 2016;534:213–7.
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, et al. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010;59:3049–57. https://doi.org/10.2337/db10-0253.
Liou AP, Paziuk M, Luevano J-M, Machineni S, Turnbaugh PJ, Kaplan LM. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med. 2013;5(178):178ra41. https://doi.org/10.1126/scitranslmed.3005687.
• Tremaroli V, Karlsson F, Werling M, Ståhlman M, Kovatcheva-Datchary P, Olbers T, et al. Roux-en-Y gastric bypass and vertical banded gastroplasty induce long-term changes on the human gut microbiome contributing to fat mass regulation. Cell Metabolism. 2015;22(2):228–38. https://doi.org/10.1016/j.cmet.2015.07.009. Study showing changes in the gut microbiome after RYGB and VBG, along with changes in levels of fecal and circulating metabolites; colonization of germ-free mice with stool from surgical subjects showed a reduction in fat deposition in recipients, providing evidence for the role of the microbiome in weight regulation.
Ilhan ZE, DiBaise JK, Isern NG, Hoyt DW, Marcus AK, Kang DW, et al. Distinctive microbiomes and metabolites linked with weight loss after gastric bypass, but not gastric banding. ISME J. 2017;11(9):2047–58. https://doi.org/10.1038/ismej.2017.71.
Cheung GW, Kokorovic A, Lam CK, Chari M, Lam TK. Intestinal cholecystokinin controls glucose production through a neuronal network. Cell Metab. 2009;10:99–109.
Powley TL, Chi MM, Schier LA, Phillips RJ. Obesity: should treatments target visceral afferents? Physiol Behav. 2005;86:698–708.
Sobocki J, Fourtanier G, Estany J, Otal P. Does vagal nerve stimulation affect body composition and metabolism? Experimental study of a new potential technique in bariatric surgery. Surgery. 2006;139:209–16.
Moran TH. Cholecystokinin and satiety: current perspectives. Nutrition. 2000;16:858–65.
Berthoud HR, Shin AC, Zheng H. Obesity surgery and gut-brain communication. Physiol Behav. 2011;105(1):106–19.
Browning KN, Fortna SR, Hajnal A. Roux-en-Y gastric bypass reverses the effects of diet-induced obesity to inhibit the responsiveness of central vagal motoneurones. J Physiol. 2013;591:2357–72.
Hao Z, Townsend RL, Mumphrey MB, Patterson LM, Ye J, Berthoud H-R. Vagal innervation of intestine contributes to weight loss after Roux-en-Y gastric bypass surgery in rats. Obes Surg. 2016, 24:2145–51.
Skandalakis JE, Gray SW, Soria RE, Sorg JL, Rowe JS Jr. Distribution of the vagus nerve to the stomach. Am Surg. 1980;46(3):130–9.
Roux CW, Neary NM, Halsey TJ, Small CJ, Martinez-Isla AM, Ghatei MA, et al. Ghrelin does not stimulate food intake in patients with surgical procedures involving vagotomy. J Clin Endocrinol Metab. 2005;90:4521–4.
Abbott CR, Monteiro M, Small CJ, Sajedi A, Smith KL, Parkinson JR, et al. The inhibitory effects of peripheral administration of peptide YY(3–36) and glucagon-like peptide-1 on food intake are attenuated by ablation of the vagal–brainstem–hypothalamic pathway. Brain Res. 2005;1044:127–31.
Breen DM, Rasmussen BA, Kokorovic A, Wang R, Cheung GW, Lam TK. Jejunal nutrient sensing is required for duodenal-jejunal bypass surgery to rapidly lower glucose concentrations in uncontrolled diabetes. Nat Med. 2012;18(6):950–5. https://doi.org/10.1038/nm.2745.
Salinari S, Carr RD, Guidone C, Bertuzzi A, Cercone S, Riccioni ME, et al. Nutrient infusion bypassing duodenum-jejunum improves insulin sensitivity in glucose-tolerant and diabetic obese subjects. AJP Endocrinol Metab. 2013;305(1):E59–66. https://doi.org/10.1152/ajpendo.00559.2012.
• Cavin JB, Couvelard A, Lebtahi R, Ducroc R, Arapis K, Voitellier E, et al. Differences in alimentary glucose absorption and intestinal disposal of blood glucose after Roux-en-Y gastric bypass vs sleeve gastrectomy. Gastroenterology. 2016;150(2):454–64. https://doi.org/10.1053/j.gastro.2015.10.009. This is a recent publication pointing to intestinal adaptation as a putative mechanism for glucose control after gastric bypass and sleeve gastrectomy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Caroline Andrew declares that she has no conflict of interest.
Devika Umashanker declares that she has no conflict of interest.
Louis J. Aronne has received consulting fees from and/has served on advisory boards for Jamieson Laboratories, Pfizer, Novo Nordisk, Eisai, GI Dynamics, Real Appeal, Janssen, United Health Group Ventures, and Gelesis; has received research funding from Aspire Bariatrics, Eisai, and AstraZeneca; has an equity interest in BMIQ, Zafgen, Gelesis, MYOS, and Jamieson Laboratories; and has served on a board of directors for MYOS, BMIQ and Jamieson Laboratories.
Alpana P. Shukla declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Obesity Treatment
Rights and permissions
About this article
Cite this article
Andrew, C.A., Umashanker, D., Aronne, L.J. et al. Intestinal and Gastric Origins for Diabetes Resolution After Bariatric Surgery. Curr Obes Rep 7, 139–146 (2018). https://doi.org/10.1007/s13679-018-0302-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-018-0302-2