Abstract
Obese individuals are advised to engage in daily physical activity to improve health and manage body weight. Walking is the most popular form of physical activity, yet the effects of obesity on the biomechanics of walking are still being discovered. In this review, I highlight recent research that has found that childhood and adult obesity are associated with slower level walking speeds, wider steps, and greater loads across lower extremity joints. Given the likely increase in risk of musculoskeletal injury/pathology in obese individuals, clinicians should use caution when recommending brisk walking as a form of physical activity. I also address how improvements in our ability to measure and model musculoskeletal actions as well as further cross-sectional and longitudinal studies will enhance our understanding of how obesity affects our ability to perform essential locomotor tasks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overweight and obese individuals are encouraged to engage in daily physical activity. Locomotor activity, walking in particular, is the most popular form of physical activity for weight management [1], presumably because it is easy to do and requires considerable metabolic energy. While studies that investigate how obesity affects the physiological responses to locomotion are essential and ongoing [2–9], biomechanical studies are also critical. Quantifying how obesity affects the biomechanics of gait provides important insights into the relationship between metabolic and mechanical energetics, mechanical loading (eg, joint loads), and the associated risk of musculoskeletal injury and/or pathology. Thus, biomechanical studies are necessary to advance basic science as well as to develop effective physical activity recommendations that achieve energy expenditure goals while reducing the risk of musculoskeletal injury in obese individuals.
Our understanding of how obesity affects gait biomechanics in adults and children is increasing, and there is now a body of literature and several reviews [10–13] describing the biomechanics of level walking in obese adults and children. While potentially limited by motion capture accuracy, these studies show that obese adults and children walk differently than their non-obese peers. Although there are fewer studies, those that examine the kinetics of gait generally report greater forces and moments in obese compared to non-obese individuals, suggesting greater musculoskeletal loads. Biomechanical studies of obese individuals with osteoarthritis (OA) demonstrate that obese individuals experience greater and abnormal (ie, altered distribution) joint loads that likely contribute to the development and/or progression of OA. Recent studies have also quantified the positive effects of weight loss on the biomechanics of walking. Acknowledging the progress in our knowledge of obesity’s effect on gait, there are several areas that have received little/no attention. These include techniques to improve kinematic data to address the considerable soft tissue over the skeleton, longitudinal studies, gradient locomotion (uphill and downhill), and running.
The aim of this review is to summarize the literature regarding the kinematics and kinetics of walking as well as mechanical work and its relationship to metabolic rate in adults and children. In addition, I will review the effectiveness of weight loss and other interventions aimed at reducing the risk of musculoskeletal injury/pathology. Given the importance of providing evidence-based recommendations to patients, the clinical implications of the literature will also be discussed. As there is much yet to learn, I will provide recommendations for future research efforts.
Lower Extremity Biomechanics and Obesity
Kinematics
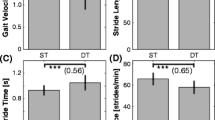
Obese adults and children tend to prefer slower walking speeds than their non-obese peers. Typical walking speeds are ~1.4 m/s for non-obese [3, 14] and ~1.2 m/s for obese adults [7, 15–17], although self-selected speeds may be inversely related to body mass index (BMI) [3, 18]. In children, walking speed is dependent upon age, but obese children still walk ~10 %–15 % slower than non-obese [19, 20]. The effects of obesity during level walking at a particular speed also include an increase in time spent in stance and less time in swing [16, 19, 21–24], a longer period of double support (both feet on the ground) [16, 21, 22], and an increased step width [19, 21, 25, 26]. Collectively, these adaptations are thought to arise from anthropometric characteristics (eg, increased thigh diameter) as well as the need to maintain balance during gait. Several studies have demonstrated that balance is impaired in obese adults [20, 27] and can be improved with weight loss [28–30]. Recently, Peyrot et al. reported that the mass-specific metabolic cost associated with body weight support and balance was reduced following weight loss in obese adolescents [31]. This study suggests that improvements in balance may be partially responsible for the improved walking economy in weight-reduced individuals.
Movements of the lower extremities are affected by obesity, with differences being reported in sagittal, frontal, and transverse plane hip, knee, and ankle joint angles. However, there is no clear consensus on kinematic adaptations associated with adult or pediatric obesity. While some investigations report that obese adults and children walk with a more erect sagittal plane posture compared to non-obese individuals (eg, less flexed lower extremity joints), [22, 32], others do not report such a finding [16, 17, 21, 33]. One reason for the conflicting results is that walking speed has not been controlled in some studies, even though walking speed influences kinematics [34]. Thus, the differences in kinematics (less flexion) may be as much due to speed as obesity. As noted above, BMI might also play a role in sagittal plane joint kinematics, as studies that report a more erect walking posture used individuals with a greater BMI. If so, there may be a BMI threshold (~40 kg/m2) above which sagittal plane kinematics are altered, ostensibly to reduce the muscle forces required to support body weight (and consequently reduce joint loads).
Not surprisingly, frontal plane walking kinematics may also be affected by obesity, but again, consensus is lacking and the differences between obese and non-obese are typically small. Hip abduction has been reported to be greater in obese versus non-obese adults and children [10, 16, 26], but these results are not reported in all studies [17, 35]. Differences in frontal plane hip angles in obese individuals could result from the need for increased leg circumduction due to thigh dimensions or an increase in pelvic tilt due to stance leg hip abductor weakness. Lai et al. [17] report greater knee adduction in obese versus non-obese adults, while Shultz et al. [10] show no differences between obese and non-obese children and McMillan et al. [35] report slightly greater knee abduction during stance in obese versus non-obese adolescents. It is important to note that all of these studies compared kinematics at different walking speeds. Foot eversion is greater in obese versus non-obese adults [17, 36], but not in children [10, 35]. Very few studies have reported transverse plane angles in obese adults. The primary finding of these studies is that obese individuals walk with a greater toe-out angle (ie, foot progression angle) [25, 36, 37]. In summary, obesity clearly affects walking speed and spatiotemporal variables, but at this time there is no characteristic kinematic pattern that can be associated with all obese adults and children.
Kinetics
A primary determinant of walking kinetics is body mass; thus, obesity has a significant effect on ground reaction forces (GRFs) and lower extremity kinetics (joint reaction forces and net muscle moments [NMMs]). The interpretation of kinetic data, however, must consider whether the data is normalized. As joints experience the absolute forces/moments, non-normalized kinetic data should be used if the aim is to estimate joint loading [38]. However, when comparing across groups, normalization can provide insights into changes that occur independent of body size.
Kinetic investigations involving obese individuals have focused on describing lower extremity NMMs. NMMs provide insights into neuromuscular control and joint loading as well as mechanical work and power. NMMs are determined using an inverse dynamics approach, with joint kinematics and GRFs as inputs. Compared to non-obese individuals, obese individuals experience greater GRFs (N) during walking, but the increases are generally proportional to body mass (N/kg) [21, 33]. We and others have found that absolute (Nm) peak NMMs at the hip, knee, and ankle were greater in moderately obese versus non-obese adults and children [10, 17, 21, 26, 35]. Conversely, DeVita et al. [22] found that absolute hip and knee peak NMM were similar while the ankle peak NMM was greater in class III obese (BMI >40 kg/m2) adults, but a recent study by this same group suggests greater hip, knee, and ankle peak NMM in class III obese adults [33]. As NMMs are a proxy measure for axial joint loading, these results suggest that obesity increases peak loads across lower extremity joints, a finding that has been supported using a simple musculoskeletal model [39]. When peak sagittal plane NMMs are normalized by body mass, hip and knee NMM are similar but ankle moments are reduced in obese versus non-obese individuals [17, 21, 26, 35]. This suggests that obese individuals may rely on more proximal joints to perform the work required to walk.
A few studies have quantified frontal plane NMM in healthy obese individuals, particularly at the knee due to the relationship between this NMM (internal abduction or external adduction) and medial compartment loading [40, 41]. Peak external knee adduction NMMs (Nm) are greater in obese adults without OA compared to non-obese adults [17, 21, 26, 42], as is the knee adduction angular impulse [43]. These findings have been used as evidence that obesity may increase the risk of developing medial compartment OA [44–46]. Particularly troubling is the finding that obese children may also experience these greater adduction moments [10, 32], although this has not been reported in adolescents [35]. Greater adduction moments in children may result in the development of altered frontal plane alignment, further increasing the risk of OA development as adults [47].
Given the greater loads experienced by the lower extremity joints of obese individuals, the link between obesity and OA is thought to be due, in part, to mechanical loading [48, 49, 50•] and varus limb alignment (ie, bowlegged) [51, 52]. There are surprisingly few reports of lower extremity gait mechanics in obese individuals with OA. Most notable is the work of Miller et al. [53], whose ADAPT (Arthritis, Diet, and Activity Promotion Trial) intervention quantified gait biomechanics and knee joint forces before and after weight loss [39, 54]. Obese individuals in this study were found to walk slower and have associated changes in lower extremity kinematics [54, 55•]. In addition, these individuals walk with a greater external knee adduction moment [56]. Schipplein and Andriacchi [57] have reported greater adduction moments are accompanied by increased flexion/extension NMMs in individuals with OA, presumably to increase compressive forces that stabilize the knee joint. Of course, these greater compressive forces may act to accelerate the progression of OA.
Limitations of Motion Capture in Obese Individuals
Although there is increasing evidence that obesity affects lower extremity joint kinematics and kinetics, these results must be viewed with a clear understanding of the challenges associated with quantifying motions of a skeletal system covered by extensive soft tissue. Unfortunately, almost all studies reporting lower extremity kinematics/kinetics in obese individuals have used standard gait marker sets (eg, Vicon plug-in-gait) with almost no mention of model calibration procedures. This is surprising given the reported errors in kinematic and kinetic calculations associated with inaccurate marker placement and soft tissue artifact [58–61]. Of particular concern is the reliance on Anterior Superior Iliac Spine (ASIS) and/or greater trochanter markers to establish the pelvis and hip joint centers. We have found that markers placed over the soft tissue in the approximate location of the ASIS can be placed anterior to the true ASIS location by up to 14 cm (unpublished observations). This will result in inaccurate estimates of joint centers and errors in the resultant kinematics/kinetics (hip and knee in particular; Fig. 1) [62]. Future studies that report kinematic data using obese subjects need to clearly identify marker placement and skeletal model development procedures and how errors regarding marker placement were addressed. We recommend a combination of using dual-energy X-ray absorptiometry images for determining inter-ASIS distance and estimating segment inertial parameters [63–65], a sacral marker cluster and digitized pelvic anatomical landmarks [42] to improve the accuracy of marker-based motion capture. While this approach should improve kinematic accuracy, other methods for collecting kinematic data (eg, biplanar fluoroscopy) are needed [66].
Mean hip joint power (W/kg) during the stance phase of level walking at 1.25 m/s in moderately obese adults. This figure highlights the effect of marker set/calibration protocol on inverse dynamics derived variables. The standard marker set uses typical skin-mounted markers over the anterior superior iliac spine (ASIS) and sacrum to define the pelvis and thigh and knee markers to define the thigh. The full marker set uses a sacral cluster (5 markers), digitized pelvic markers over the ASIS, thigh cluster, and knee markers. The difference in hip power is primarily due to changes in the net muscle moment due to the estimated hip joint center and suggests that interpretation of joint mechanics data (particularly at the hip) is very sensitive to marker placement and calibration protocols
Mechanical Work
Walking requires complex movements of the lower extremities but can be modeled as a simple inverted pendulum [67] that conserves mechanical energy via the exchange of kinetic and potential energies during stance. This conversion is not perfect, however, and external mechanical work (Wext) is required to raise and accelerate the center of mass [68], particularly during double support [69]. In addition, internal mechanical work (Wint) is required to move the limbs relative to the center of mass [70]. Wext is a primary determinant of the metabolic cost of walking [71], and obese individuals walk with a greater metabolic cost compared to non-obese individuals. Thus, a few recent investigations have explored the effect of obesity on Wext. We calculated individual-limb Wext during walking in obese and non-obese adults and found no differences in Wext (J/step/kg) between the groups [72]. The individual-limb method of determining Wext uses leading and trailing limb GRFs during double support and is thought to best represent Wext during walking [69]. This method also has the advantage of not relying on potentially error-prone kinematic data. Our results and those of others using different methods [73, 74, 75•] would suggest that Wext is not responsible for the greater mass-specific metabolic cost of walking in obese adults. The similarity in mass-specific Wext in obese and non-obese individuals also makes it unlikely that obesity encourages the development of energy-conserving gait alterations, as has been observed in African head-load carriers [76] and Nepalese porters [77]. To date, no studies have quantified Wint in obese individuals. It is possible that the heavier legs associated with obesity would require greater Wint during walking, particularly given that obese individuals swing their legs more rapidly (shorter swing time) and with more lateral circumduction than non-obese individuals.
Work performed by individual joints can be quantified using NMMs and angular velocities. As is the case with Wext, joint work has been shown to be related to metabolic cost in non-obese adults during level walking [78]. Given the greater NMMs and similar sagittal plane kinematics, absolute positive joint work is greater but mass-specific joint work is similar in obese versus non-obese adults [22, 26]. Joint work can also be used to examine storage and return of elastic energy within a joint as well as transfer of energy across joints. At the ankle during stance, there is a long period of negative work followed by a relatively brief period of positive work. This pattern would suggest opportunities for storage and return of elastic energy in the Achilles tendon [79], which may be enhanced in obese individuals due to the greater triceps surae forces required to walk. Future studies using ultrasound imaging are needed to confirm this hypothesis. Not all work need be performed by muscles, tendons, and ligaments, as movement of other soft tissue (eg, adipose) can also perform work on the center of mass. Zelik et al. [80] recently compared Wext and joint work during level walking and found that soft tissues did in fact contribute to Wext. Given the much greater soft tissue mass in obese individuals, we would expect that soft tissue work may be greater and help to reduce the metabolic cost of walking in obese adults.
Weight Loss and Other Interventions
The scientific literature regarding weight loss in obese individuals is extensive, but only a few studies have examined changes in walking biomechanics in weight-reduced individuals. As expected, walking speed increases after weight loss, as does the percent of the gait cycle spent in swing [7, 33]. Peyrot et al. [75•] reported that stride frequency and lateral leg swing decreased while stride length increased when obese adolescents who lost ~5 % of body mass walked at 1.25 m/s. In addition, Peyrot et al. [75•] show that net metabolic cost decreased more than would be expected based on the change in body mass and that this decrease was related to changes in body mass, lateral kinetic and vertical potential energy, single support duration, percent body fat and percent gynoid fat [75•]. Although this study did not collect kinematic data, results suggest that kinematic changes (hip and knee extension) may have been responsible for the reduction in net metabolic cost.
Hortobágyi et al. [33] recently published a study that recorded biomechanics data before and after bariatric surgery. Participants in this study lost ~34 % of their initial mass (~42 kg) over a 13-month period, and self-selected walking speed increased as body mass decreased. Although this study reports changes in lower extremity kinematics and kinetics (NMMs, Nm/kg) at self-selected speeds, no changes are reported at a standard speed (1.5 m/s), suggesting that the weight loss did not alter sagittal plane kinematics and that changes in NMMs were due to changes in body mass. Although faster walking speeds are generally thought to be advantageous, in this study the increased speeds mitigated some of the decreases in joint loading associated with weight loss. Similar findings have been reported in obese individuals with OA. Messier et al. [39] have reported that knee joint loads were decreased with weight loss as did a study by Aaboe et al. [55•]. While not a biomechanical study, weight loss has also been associated with reductions in musculoskeletal pain [81], which would presumably make walking more comfortable and could also influence walking speed.
While most obesity-related interventions focus on weight loss, recent investigations have explored the effects of gradient, stride length, and lateral wedges on walking biomechanics [43, 82, 83]. Our group is exploring the combination of slower walking speeds and moderate inclines as a form of walking exercise for obese adults. Initial results suggest that walking at 0.75 m/s up a 6° inclined treadmill is metabolically similar to walking on a level treadmill at 1.50 m/s, but results in smaller peak knee NMMs and loading rates compared to the faster level speed [82]. Russell et al. [83] had obese women walk with an increased stride frequency while walking speed was held constant. This manipulation increased metabolic rate slightly (~5 %) but did not change the knee external adduction moment or impact shock, suggesting that walking with a greater stride frequency may increase energy expenditure while not increasing the risk of musculoskeletal injury or OA [83]. Another study by Russell and Hamill [43] used laterally wedged insoles as a means of reducing medial compartment knee loading during walking in obese women. The lateral wedges did decrease the knee external adduction moment, suggesting shoe-based interventions may be a useful strategy to reduce the risk of OA in moderately obese females.
Muscle Function and Obesity
Muscle function, particularly strength and voluntary fatigue, are affected by obesity. As a result, obese individuals may find some locomotor tasks (eg, prolonged exercise, stairs) difficult. While obese individuals have greater absolute strength than non-obese individuals, their strength normalized to body mass is reduced [84–86]. Class III obese adults have also been reported to have reduced voluntary fatigue resistance in the quadriceps muscle group compared to non-obese adults [87], but this has not been confirmed in less obese (Class I) adolescents [88]. A reduction in relative strength and fatigue resistance likely reduces functional capacity and mobility [89] and also possibly increases the risk of falls during locomotor tasks [90].
Application of Current Knowledge to Clinical Practice
Our understanding of how obesity affects the biomechanics of walking continues to improve and can be used to guide physical activity recommendations for obese adults and children seeking weight management guidance. Clearly, weight loss should remain the primary goal, due to its ability to reduce stresses on lower extremity joints and improve balance control. Regular physical activity should be advised, but an assessment of current levels of physical activity, ideally with an objective method (eg, accelerometry), should be completed prior to making specific recommendations. If patients are not currently physically active, and this is likely the case [91, 92], a program that gradually increases physical activity (aerobic and resistance) will likely reduce the risk of musculoskeletal injury associated with initiation of regular physical activity [93].
Walking should be recommended as an appropriate form of exercise for obese adults and children without OA or varus knee alignment to promote or maintain weight loss. However, suggesting moderate speeds (<1.25 m/s) rather than brisk or fast walking is sound advice. Although energy expenditure will be reduced compared to faster walking speeds, the risk of musculoskeletal injury will likely be smaller. Slower speeds (~1.0 m/s) should be recommended for class III obese individuals, assuming these individuals have no pre-existing musculoskeletal complaints. Alternatively, class III obese individuals may do well to walk on a treadmill with body weight support, as this will reduce GRFs while allowing reasonable walking speeds. This type of exercise intervention may be particularly useful prior to bariatric surgery to develop familiarity and compliance with regular physical activity. For obese individuals with OA, bicycling or other forms of non-weight-bearing physical activity should be recommended, although slow walking may also prove effective. Walking relatively slowly on a moderately inclined treadmill may also be an effective strategy as it elicits an appropriate physiological intensity and may reduce the risk of musculoskeletal injury/pathology [82]. Obese children should be enthusiastically encouraged to engage in regular physical activity, with activities selected that minimize joint pain. While walking can and should be recommended, other age-appropriate activities (eg, playground activities) are essential for motor development, balance, stability, and functional capacity.
Future Directions
Given the prevalence of childhood and adult obesity and the lack of effective, long-term weight loss interventions, it is critical that we continue to improve our understanding of how obesity affects the biomechanics and energetics of human locomotion. As noted above, particular attention should be directed toward improving our ability to record the movements and activation of the musculoskeletal system in obese individuals. This will most certainly include the use of imaging technologies (eg, x-ray) to guide marker placement or as a data collection methodology. Ideally, this research will progress with an aim of aiding investigators who do not possess these technologies in improving their ability to collect and analyze kinematic data. For example, biplanar fluoroscopy could be used to develop circumference-based equations to estimate anatomical landmarks for kinematic models. The absence of electromyographic data in obese individuals adds to our limited understanding of how muscles function and studies that utilize surface or in-dwelling electrodes are needed. Integrative approaches that quantify both mechanical and metabolic responses to locomotion are lacking, resulting in a limited understanding of how obesity affects locomotor efficiency. Finally, the use of ultrasound may also provide needed insights into muscle/tendon function.
Additional studies of individuals of varying ages, degrees of adiposity, ethnicities/race, and comorbidities associated with obesity (eg, diabetes) are needed to develop a comprehensive understanding of how obesity affects locomotion. This includes studies on very young (<4 years old) children and older adults as well as severely obese (BMI >50 kg/m2) individuals. As noted above, obesity is typically associated with poor aerobic capacity [7], reduced relative strength, and limited muscular endurance [87], yet we have no information on how gait mechanics change with fatigue in obese individuals. It may be that alterations in gait associated with fatigue further increase the risk of musculoskeletal injury or abnormal loading [94]. Given the association between body weight and joint loading, further attempts to develop interventions intended to moderate this relationship are vital. Investigations using body weight support, assistive devices, and/or powered orthosis will allow the development of new interventions that may facilitate weight management success. A critical need is longitudinal data so that we may better understand the etiology of musculoskeletal disorders associated with obesity and the effects of weight loss approaches (eg, bariatric surgery) on the risk of these disorders. With the exception of the few studies mentioned above, little is known about how increasing or decreasing body mass, cardiovascular fitness, or musculoskeletal strength affects gait biomechanics in obese individuals. Such studies are necessary to implement successful weight management programs that promote physiological as well as musculoskeletal health.
We also need to extend our knowledge of how obesity effects gait beyond level walking. Although level walking is an essential and common form of physical activity, individuals encounter gradients and surface variations (eg, soft or rocky paths), and may even engage in running. To date, there is almost no data on how variations in terrain influence the biomechanics of walking in obese individuals and there is no data on running, even in children. The development of inclinable, instrumented treadmills should facilitate this research. Finally, the utilization of complex, individualized musculoskeletal models (eg, OpenSim [95]) will allow estimates of muscle function and joint loading and will also allow us to predict the outcome of interventions prior to their implementation.
Conclusions
Obese adults and children accommodate their greater body mass by walking slower with wider steps. While obese individuals make relatively minor kinematic adjustments compared to non-obese individuals during level walking, they experience greater forces across their lower extremity joints that likely predispose them to musculoskeletal injury/pathology. As a result, caution must be used when recommending brisk walking as a form of physical activity. Improvements in quantifying movements and actions of the musculoskeletal system in obese individuals, combined with longitudinal studies, will improve our ability to prescribe walking as a form of physical activity for weight management.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1):222S–5S.
Ayub BV, Bar-Or O. Energy cost of walking in boys who differ in adiposity but are matched for body mass. Med Sci Sports Exerc. 2003;35(4):669–74.
Browning RC, Baker EA, Herron JA, Kram R. Effects of obesity and sex on the energetic cost and preferred speed of walking. J Appl Physiol. 2006;100(2):390–8.
Foster GD, Wadden TA, Kendrick ZV, et al. The energy cost of walking before and after significant weight loss. Med Sci Sports Exerc. 1995;27(6):888–94.
Bloom WL, Marshall FE. The comparison of energy expenditure in the obese and lean. Metabolism. 1967;16(8):685–92.
Freyschuss U, Melcher A. Exercise energy expenditure in extreme obesity: influence of ergometry type and weight loss. Scand J Clin Lab Inves. 1978;38(8):753–9.
Mattsson E, Larsson UE, Rossner S. Is walking for exercise too exhausting for obese women? Int J Obes. 1997;21(5):380–6.
Lafortuna CL, Agosti F, Galli R, et al. The energetic and cardiovascular response to treadmill walking and cycle ergometer exercise in obese women. Eur J Appl Physiol. 2008;103(6):707–17.
Peyrot N, Thivel D, Isacco L, et al. Do mechanical gait parameters explain the higher metabolic cost of walking in obese adolescents? J Appl Physiol. 2009;106(6):1763–70.
Shultz SP, Anner J, Hills AP. Paediatric obesity, physical activity and the musculoskeletal system. Obes Rev. 2009;10(5):576–82.
Shultz SP, Browning RC, Schutz Y, et al. Childhood obesity and walking: guidelines and challenges. Int J Pediatr Obes. 2011;6(5–6):332–41.
Runhaar J, Koes BW, Clockaerts S, Bierma-Zeinstra SMA. A systematic review on changed biomechanics of lower extremities in obese individuals: a possible role in development of osteoarthritis. Obes Rev. 2011;12(12):1071–82.
Nantel J, Mathieu ME, Prince F. Physical activity and obesity: biomechanical and physiological key concepts. J Obes. 2011;201(1):650230.
Bornstein, MH and Bornstein, HG: The pace of life. Nature 1976, 259.
Melanson EL, Bell ML, Knoll JR, et al. Body mass index and sex influence the energy cost of walking at self-selected speeds. Med Sci Sports Exerc. 2003;35(5 Supplement):S183.
Spyropoulos P, Pisciotta JC, Pavlou KN, et al. Biomechanical gait analysis in obese men. Arch Phys Med Rehabil. 1991;72(13):1065–70.
Lai PPK, Leung AKL, Li ANM, Zhang M. Three-dimensional gait analysis of obese adults. Clin Biomech. 2008;23(1):S2–6.
Browning RC, Kram R. Energetic cost and preferred speed of walking in obese vs. normal weight women. Obes Res. 2005;13:891–9.
Hills AP, Parker AW. Gait characteristics of obese children. Archives of Physical Medicine & Rehabilitation. 1991;72(6):403–7.
McGraw B, McClenaghan BA, Williams HG, et al. Gait and postural stability in obese and nonobese prepubertal boys. Arch Phys Med Rehabil. 2000;81(4):484–9.
Browning RC, Kram R. Effects of obesity on the biomechanics of walking at different speeds. Med Sci Sports Exerc. 2007;39(9):1632–41.
DeVita P, Hortobagyi T. Obesity is not associated with increased knee joint torque and power during level walking. J Biomech. 2003;36:1355–62.
Messier SP, Ettinger WH, Doyle TE, et al. Obesity: Effects on gait in an osteoarthritic population. J Appl Biomech. 1996;12:161–72.
Lai PP, Leung AK, Li AN, Zhang M. Three-dimensional gait analysis of obese adults. Clin Biomech (Bristol, Avon). 2008;23(1):S2–6.
Vismara L, Bertocco P, Parisio C, et al. Gait analysis on a treadmill in young, obese women. J Appl Biomater Biomech. 2006;4:215–6.
Ko S-u, Stenholm S, Ferrucci L. Characteristic gait patterns in older adults with obesity--Results from the Baltimore Longitudinal Study of Aging. J Biomech. 2010;43(6):1104–10.
Hue O, Simoneau M, Marcotte J, et al. Body weight is a strong predictor of postural stability. Gait Posture. 2007;26(1):32–8.
Handrigan G, Hue O, Simoneau M, et al. Weight loss and muscular strength affect static balance control. Int J Obes. 2010;34(5):936–42.
Teasdale N, Hue O, Marcotte J, et al. Reducing weight increases postural stability in obese and morbid obese men. Int J Obes (Lond). 2007;31(1):153–60.
Maffiuletti NA, Agosti F, Proietti M, et al. Postural instability of extremely obese individuals improves after a body weight reduction program entailing specific balance training. J Endocrinol Invest. 2005;28(1):2–7.
Peyrot N, Thivel D, Isacco L, et al. Why does walking economy improve after weight loss in obese adolescents? Med Sci Sports Exerc. 2012;44(4):659–65.
Gushue DL, Houck J, Lerner AL. Effects of childhood obesity on three-dimensional knee joint biomechanics during walking. J Pediatr Orthop. 2005;25(6):763–8.
Hortobágyi T, Herring C, Pories WJ, et al. Massive weight loss-induced mechanical plasticity in obese gait. J Appl Physiol. 2011;111(5):1391–9.
Lelas JL, Merriman GJ, Riley PO, Kerrigan DC. Predicting peak kinematic and kinetic parameters from gait speed. Gait Posture. 2003;17(2):106–12.
McMillan AG, Pulver AM, Collier DN, Williams DS. Sagittal and frontal plane joint mechanics throughout the stance phase of walking in adolescents who are obese. Gait Posture. 2010;32(2):263–8.
Messier SP, Davies AB, Moore DT, et al. Severe obesity: Effects on foot mechanics during walking. Foot Ankle. 1994;15:29–34.
de Souza SA, Faintuch J, Valezi AC, et al. Gait cinematic analysis in morbidly obese patients. Obes Surg. 2005;15(9):1238–42.
Robbins SM, Birmingham TB, Maly MR, et al. Comparative diagnostic accuracy of knee adduction moments in knee osteoarthritis: a case for not normalizing to body size. J Biomech. 2011;44(5):968–71.
Messier SP, Gutekunst DJ, Davis C, DeVita P. Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum. 2005;52(7):2026–32.
Andriacchi TP. Dynamics of knee malalignment. Orthop Clin North Am. 1994;25:395–403.
Shelburne KB, Torry MR, Steadman JR, Pandy MG. Effects of foot orthoses and valgus bracing on the knee adduction moment and medial joint load during gait. Clin Biomech (Bristol, Avon). 2008;23(6):814–21.
Segal NA, Yack HJ, Khole P. Weight, rather than obesity distribution, explains peak external knee adduction moment during level gait. Am J Phys Med Rehabi. 2009;88(3):180–8.
Russell EM, Hamill J. Lateral wedges decrease biomechanical risk factors for knee osteoarthritis in obese women. J Biomech. 2011;44(12):2286–91.
Miyazaki T, Wada M, Kawahara H, et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–22.
Baliunas AJ, Hurwitz D, Ryals A, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002;10:573–9.
Messier SP. Osteoarthritis of the knee and associated factors of age and obesity: Effects on gait. Med Sci Sports Exerc. 1994;26(12):1446–52.
Taylor ED, Theim KR, Mirch MC, et al. Orthopedic complications of overweight in children and adolescents. Pediatrics. 2006;117(6):2167–74.
Felson DT, Anderson JJ, Naimark A, et al. Obesity and knee osteoarthritis: The Framingham study. Ann Intern Med. 1988;109:18–24.
Griffin TM, Guilak F. The role of mechanical loading in the onset and progression of osteoarthritis. Exerc Sport Sci Rev. 2005;33(4):195–200.
• Andriacchi TP, Koo S, Scanlan SF. Gait mechanics influence healthy cartilage morphology and osteoarthritis of the knee. J Bone Joint Surg Am. 2009;91 Suppl 1:95–101. This study used MRI of the cartilage and walking mechanics to show that altered repetitive loading can influence the initation and progression of knee OA. These findings suggest that joint injury, in addition to obesity, must be considered in the assessment of OA risk.
Sharma L, Lou C, Cahue S, Dunlop DD. The mechanism of the effect of obesity in knee osteoarthritis: the mediating role of malalignment. Arthritis Rheum. 2000;43(3):568–75.
Felson DT, Goggins J, Niu J, et al. The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum. 2004;50(12):3904–9.
Miller GD, Rejeski WJ, Williamson JD, et al. The Arthritis, Diet and Activity Promotion Trial (ADAPT): Design, rationale, and baseline results. Control Clin Trials. 2003;24(4):462–80.
Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: The arthritis, diet, and activity promotion trial. Arthritis Rheum. 2004;50(5):1501–10.
• Aaboe J, Bliddal H, Messier SP, et al. Effects of an intensive weight loss program on knee joint loading in obese adults with knee osteoarthritis. Osteoarthritis Cartilage. 2011;19(7):822–8. This study used a relatively large sample to quantify the reduction in knee joint load with weight loss and demonstrates the significant impact of weight reduction to reduce joint loading.
Andriacchi TP, Mundermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol. 2006;18(5):514–8.
Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(1):113–9.
Baker R. Gait analysis methods in rehabilitation. J Neuroeng Rehabil. 2006;3:4.
Della Croce U, Leardini A, Chiari L, Cappozzo A. Human movement analysis using stereophotogrammetry: Part 4: assessment of anatomical landmark misplacement and its effects on joint kinematics. Gait Posture. 2005;21(2):226–37.
Leardini A, Cappozzo A, Catani F, et al. Validation of a functional method for the estimation of hip joint centre location. J Biomech. 1999;32(1):99–103.
Taylor WR, Ehrig RM, Duda GN, et al. On the influence of soft tissue coverage in the determination of bone kinematics using skin markers. J Orthop Res. 2005;23(4):726–34.
Stagni R, Leardini A, Cappozzo A, et al. Effects of hip joint centre mislocation on gait analysis results. J Biomech. 2000;33(11):1479–87.
LaForgia J, Dollman J, Dale MJ, et al. Validation of DXA body composition estimates in obese men and women. Obes. 2009;17(4):821–6.
Chambers AJ, Sukits AL, McCrory JL, Cham R. The effect of obesity and gender on body segment parameters in older adults. Clin Biomech (Bristol, Avon). 2010;25(2):131–6.
Matrangola SL, Madigan ML, Nussbaum MA, et al. Changes in body segment inertial parameters of obese individuals with weight loss. J Biomech. 2008;41(15):3278–81.
Farrokhi S, Tashman S, Gil AB, et al. Are the kinematics of the knee joint altered during the loading response phase of gait in individuals with concurrent knee osteoarthritis and complaints of joint instability? A dynamic stereo X-ray study. Clin Biomech (Bristol, Avon). 2012;27(4):384–9.
Margaria, R, Biomechanics and Energetics of Muscular Exercise. 1976, Oxford: Clarendon Press. 146.
Cavagna GA, Saibene FP, Margaria R. External work in walking. J Appl Physiol. 1963;18(1):1–9.
Donelan JM, Kram R, Kuo AD. Simultaneous positive and negative external mechanical work in human walking. J Biomech. 2002;35(1):117–24.
Willems PA, Cavagna GA, Heglund NC. External, internal and total work in human locomotion. J Exp Biol. 1995;198:379–93.
Donelan JM, Kram R, Kuo AD. Mechanical work for step-to-step transitions is a major determinant of the metabolic cost of human walking. J Exp Biol. 2002;205(Pt 23):3717–27.
Browning RC, McGowan CP, Kram R. Obesity does not increase external mechanical work per kilogram body mass during walking. J Biomech. 2009;42(14):2273–8.
Malatesta D, Vismara L, Menegoni F, et al. Mechanical external work and recovery at preferred walking speed in obese subjects. Med Sci Sports Exerc. 2009;41(2):426–34.
Peyrot N, Thivel D, Isacco L et al. Do mechanical gait parameters explain the higher metabolic cost of walking in obese adolescents? J Appl Physiol. 2009
• Peyrot N, Morin JB, Thivel D, et al. Mechanical work and metabolic cost of walking after weight loss in obese adolescents. Med Sci Sports Exerc. 2010;42(10):1914–22. Although a relatively small sample, the results from this study suggest that gait changes can explain at least part of the improved walking economy after weight loss. Future studies that explore these mechanical changes will provide insights into metabolic cost of walking in weight-reduced individuals.
Heglund NC, Willems PA, Penta M, Cavagna GA. Energy-saving gait mechanics with head-supported loads. Nature. 1995;375(6526):52–4.
Minetti AE, Formenti F, Ardigo LP. Himalayan porter’s specialization: metabolic power, economy, efficiency and skill. Proc Biol Sci. 2006;273(1602):2791–7.
Burdett RG, Skrinar GS, Simon SR. Comparison of mechanical work and metabolic energy consumption during normal gait. J Orthop Res. 1983;1(1):63–72.
Kawakami Y, Muraoka T, Ito S, et al. In vivo muscle-fiber behavior reveals significant contributions of tendon elasticity in stretch-shortening cycle. Med Sci Sports Excer 2000: 32(S57).
Zelik KE, Kuo AD. Human walking isn’t all hard work: evidence of soft tissue contributions to energy dissipation and return. J Exp Biol. 2010;213(Pt 24):4257–64.
McGoey BV, Deitel M, Saplys RJ, Kliman ME. Effect of weight loss on musculoskeletal pain in the morbidly obese. J Bone Joint Surg Br. 1990;72(2):322–3.
Ehlen KA, Reiser 2nd RF. and Browning, RC: Energetics and biomechanics of inclined treadmill walking in obese adults. Med Sci Sports Exerc. 2011;43(7):1251–9.
Russell EM, Braun B, Hamill J. Does stride length influence metabolic cost and biomechanical risk factors for knee osteoarthritis in obese women? Clin Biomech. 2010;25(5):438–43.
Lafortuna CL, Maffiuletti NA, Agosti F, Sartorio A. Gender variations of body composition, muscle strength and power output in morbid obesity. Int J Obes Relat Metab Disord. 2005;29(7):833–41.
Hulens M, Vansant G, Lysens R, et al. Study of differences in peripheral muscle strength of lean versus obese women: an allometric approach. Int J Obes Relat Metab Disord. 2001;25(5):676–81.
Maffiuletti NA, Agosti F, Marinone PG, et al. Changes in body composition, physical performance and cardiovascular risk factors after a 3-week integrated body weight reduction program and after 1-y follow-up in severely obese men and women. Eur J Clin Nutr. 2005;59(5):685–94.
Maffiuletti NA, Jubeau M, Munzinger U, et al. Differences in quadriceps muscle strength and fatigue between lean and obese subjects. Eur J Appl Physiol. 2007;101(1):51–9.
Maffiuletti NA, Jubeau M, Agosti F, et al. Quadriceps muscle function characteristics in severely obese and nonobese adolescents. Eur J Appl Physiol. 2008;103(4):481–4.
Choquette S, Bouchard DR, Doyon CY. Relative strength as a determinant of mobility in elders 67–84 years of age. a nuage study: nutrition as a determinant of successful aging. J Nutr Health Aging. 2010;14(3):190–5.
Himes CL, Reynolds SL. Effect of obesity on falls, injury, and disability. J Am Geriatr Soc. 2012;60(1):124–9.
Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–81.
Dunlop DD, Song J, Semanik PA, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis Rheum. 2011;63(11):3372–82.
Hootman JM, Macera CA, Ainsworth BE, et al. Epidemiology of musculoskeletal injuries among sedentary and physically active adults. Med Sci Sports Exerc. 2002;34(5):838–44.
Syed IY, Davis BL. Obesity and osteoarthritis of the knee: hypotheses concerning the relationship between ground reaction forces and quadriceps fatigue in long-duration walking. Medical Hypotheses. 2000;54(2):182–5.
Delp SL, Anderson FC, Arnold AS, et al. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Trans Biomed Eng. 2007;54(11):1940–50.
Disclosure
Conflicts of interest: R.C. Browning: has received grant support from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Browning, R.C. Locomotion Mechanics in Obese Adults and Children. Curr Obes Rep 1, 152–159 (2012). https://doi.org/10.1007/s13679-012-0021-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-012-0021-z