Abstract
Introduction
Alopecia areata (AA) can negatively affect quality of life (QoL) and is associated with increased prevalence of anxiety and depression (vs people without AA). This study compared physician-assessed and patient self-rated severity of AA in a European sample and described the patient-reported burden of AA stratified by physician-assessed severity.
Methods
Real-world data were collected from the Adelphi Real World AA Disease Specific Programme™, a retrospective point-in-time cross-sectional survey of dermatologists and their adult patients with AA in five European countries (France, Germany, Italy, Spain, UK). Physicians provided clinical data and an AA severity assessment, according to their own definition of ‘mild’, ‘moderate’ and ‘severe’. Patients were invited to provide their perception of AA severity and completed patient-reported outcome (PRO) questionnaires, including Skindex-16 for AA (Skindex-16 AA), EuroQol-5-dimension questionnaire 5-level (EQ-5D-5L), Hospital Anxiety and Depression Scale and the Work Productivity and Activity Impairment Questionnaire.
Results
Data for 2083 patients were collected by 239 physicians; 561 of these patients completed PRO questionnaires. In 78.5% of cases with available data (N = 549), there was alignment between patient and physician-rated AA severity (severity was rated higher by physicians in 15.7% of cases, by patients in 5.8% of cases). Data from all PRO instruments showed an increase in patient-reported burden and work and activity impairment with increasing physician-rated AA severity. For the Skindex-16 AA, the Emotions scale had the worst scores; anxiety/depression was the EQ-5D-5L dimension with the highest percentages of patients reporting any perceived problem.
Conclusions
These data highlight the significant impact that AA can have beyond hair loss, especially for patients with severe AA. There was substantial physician–patient alignment on severity assessment. Higher physician-rated AA severity was associated with higher levels of patient-reported disease burden, including anxiety and depression, and work and activity impairment. These data may help inform appropriate treatment strategies.
Plain Language Summary
Alopecia areata (AA) can negatively affect quality of life and is associated with increased prevalence of anxiety and depression (vs people without AA). This study used surveys of adult patients with AA in Europe and their dermatologists to compare how doctors and patients assess AA severity. We also looked at how patients rate the overall burden and broader effects of AA (not just hair loss) according to whether their doctor classed their AA as ‘mild’, ‘moderate’ or ‘severe’. Data for 2083 patients were collected by 239 doctors; 561 patients completed questionnaires about their AA and its potential effects on their quality of life, mental health and ability to work or perform other activities. In 78.5% of cases (from 549 patients with both patient and doctor-rated severity), patients and their doctors agreed on the same AA severity category (mild, moderate or severe). However, in 15.7% of cases, doctors rated AA severity as being higher than reported by the patient, and in 5.8% of cases the patient classed their AA as being more severe than reported by the doctor. Data from patient questionnaires showed that the burden associated with AA was higher in patients with more severe AA (as per their doctor’s own definition of severity); anxiety/depression was the most commonly reported problem related to quality of life. This study highlights the significant impact that AA can have beyond hair loss, especially for patients with severe AA. Information from this study may help to inform appropriate treatment strategies for people with AA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Alopecia areata (AA) can negatively affect quality of life (QoL) but only a small number of studies have investigated the level of agreement between patients and physicians in evaluating AA severity. |
Cross-sectional surveys that gain input directly from patients offer the opportunity to evaluate the association between patient-reported outcomes (PROs) and clinician-reported outcomes. |
This real-world study using data from a large number of participants in the Adelphi Real World AA Disease Specific Programme™, a retrospective point-in-time cross-sectional survey of European dermatologists and their adult patients with AA, aimed to evaluate how physician-assessed and patient self-rated severity of AA compare and describe the patient-reported burden of AA stratified by physician-assessed severity. |
What was learned from the study? |
Data from all PRO instruments used (Skindex-16 adapted for AA [Skindex-16 AA], EuroQol-5-dimension 5-level [EQ-5D-5L] questionnaire, Hospital Anxiety and Depression Scale and the Work Productivity and Activity Impairment Questionnaire) showed an increase in patient-reported burden with increasing physician-rated AA severity; emotions (Skindex-16 AA [mean scores 35.9 for mild, 42.5 for moderate, 56.2 for severe AA]) and anxiety/depression (EQ-5D-5L [44.3% of patients with mild, 49.1% moderate, 66.5% with severe AA reporting any perceived problem]) were the most adversely affected aspects. |
These data highlight the significant impact that AA can have beyond hair loss, especially for patients with severe AA; there was 78.5% physician–patient alignment on AA severity assessment. |
Introduction
Alopecia areata (AA) is an immune-mediated condition that causes non-scarring hair loss [1]. AA-associated hair loss can range from one or several patches to complete scalp and body hair loss. However, AA has broader impacts beyond hair loss; like other dermatological conditions, it can negatively affect quality of life (QoL) and is associated with increased prevalence of anxiety and depression compared with people without AA [2,3,4].
The management of AA may differ according to the clinical presentation and the impact of the disease on patient [1]. Dermatologists traditionally relied on the off-label use of various treatments, such as topical, intralesional and systemic glucocorticoids, conventional immunosuppressants and contact immunotherapy [1, 5]. In 2022, baricitinib became the first therapy approved by the European Medicines Agency and the US Food and Drug Administration (FDA) for the treatment of adults with severe AA [6, 7]. This was followed by FDA approval of ritlecitinib in 2023 for the treatment of severe AA in people aged ≥ 12 years [8].
Determination of the severity of AA is important since it informs therapeutic decision-making and can aid evaluation of clinical response and prognosis [1]. However, there is no unique definition of AA disease severity. The extent of scalp hair loss is generally considered as the driver for defining severity, although additional features have been proposed, such as the location, pattern and duration of hair loss, as well as emotional and QoL impacts of AA [9].
Previous studies have assessed the relationship between AA severity and disease burden, with conflicting results, for example, according to the definition of severity, the instruments used as well as whether severity was assessed by the patient or physician [2, 10,11,12,13,14,15,16]. Increased physician-rated severity of scalp hair loss was associated with greater impairment in QoL as measured by the Dermatology Life Quality Index (DLQI) in a study conducted in patients with mild and severe AA [15]. Conversely, no statistical correlation was observed between the Severity of Alopecia Tool (SALT) and total DLQI scores in another study [16]. A non-linear relationship was even reported between the Skindex-16 adapted for AA (Skindex-16 AA), a hair-specific QoL instrument, and patient-assessed severity of scalp hair loss in a large survey where patients with 0% and/or 95–100% missing scalp hair showed less impact on QoL than those with 1–94% scalp hair loss [17]. Only a small number of studies have investigated the level of agreement between patients and physicians in evaluating AA severity [10,11,12,13]. In a study conducted in patients with AA and other dermatological conditions, the physician global assessment of disease severity tended to be lower than the patient global assessment [10]. Another study that included patients with AA and other types of hair loss disorders showed that patients may rate their hair loss as more severe than dermatologists. Furthermore, patient-assessed severity of hair loss was strongly correlated with Skindex-16 scores, while physician-rated severity was not [11]. Similar results have been recently published, reinforcing that physician assessment of scalp hair loss might not be predictive of QoL in AA [13]. Finally, a study conducted in Japan compared physician- and patient-rated severity based on their own definition and found a moderate level of physician–patient alignment on disease severity rating [12]. Interestingly, greater physician-assessed overall disease severity was significantly associated with greater patient-reported burden of AA.
The aim of our study was to evaluate how physicians’ and patients’ assessments of AA severity compare and to describe the patient-reported burden of AA stratified by physician-assessed severity, using data from a large population of patients in Europe.
Methods
Study Design and Participants
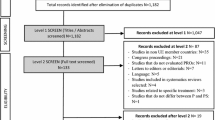
This study used data from the Adelphi Real World AA Disease Specific Programme™ (DSP), collected in France, Germany, Italy, Spain and the UK between October 2021 and June 2022. DSPs are large point-in-time cross-sectional studies based on physician and patient surveys that collect real-world data and aim to describe current clinical practice, symptom prevalence and patients’ perception of their health state and QoL across a range of chronic conditions [14].
For the AA DSP, dermatologists were identified from public lists of healthcare professionals and were invited to participate in the study if they were involved in treatment decisions for AA and had at least seven consultations per month with adult patients with AA. Participating physicians were requested to recruit at least seven patients consulting with mild (n = 1), moderate (n = 3) and severe (n = 3) AA, consecutively, until the severity quota had been reached. For each patient, physicians completed a patient record form. Patients were aged ≥ 18 years with current physician-diagnosed AA and were not participating in a clinical trial at the time of the survey. Disease severity was determined by the dermatologists as requested in the survey question, ‘What is/was your overall assessment of the severity of AA symptoms in this patient based on your own definition of the terms mild, moderate and severe?’
Data Collection
The DSP fulfils the definition of a market research survey under the European Pharmaceutical Marketing Research Association (EphMRA) Code of Conduct and is therefore conducted to market research rather than clinical guidelines [18]. Market research surveys are exempt from requiring Institutional Review Board (IRB) approval; however, the Western IRB conducted a methodological review of the AA DSP and provided an exemption. The DSP was conducted in compliance with the International Council for Harmonisation Declaration of Helsinki. Each respondent provided freely given, specific and informed consent to take part in the DSP and for the processing of their personal data. All data provided by physicians and patients were anonymised. Physicians were compensated for their participation according to fair market research rates.
For each patient recruited, physicians provided demographics and clinical characteristics (AA-related or not). At the time of their consultation, recruited patients were invited to fill in a voluntary patient self-completion form (PSC) independently of the physician. Data collected using the PSC included the patients’ assessment of their current disease severity (i.e. mild, moderate or severe), based on their own subjective perception of their AA, and of the burden associated with AA using several patient-reported outcome (PRO) questionnaires.
PROs used in this study were the Skindex-16 AA, the EuroQol-5-dimension-5-level questionnaire (EQ-5D-5L), the Hospital Anxiety and Depression Scale (HADS) and the Work Productivity and Activity Impairment Questionnaire (WPAI).
The Skindex-16 AA measured the effects of AA on patients’ QoL [19]. The instrument reports three scales, Symptoms, Emotions and Functioning, and comprises 16 Likert-scaled questions asking patients how bothersome particular aspects of their AA have been over the past week; patient responses range from ‘Never bothered’ to ‘Always bothered’. Each domain score ranges from 0 to 100, with higher scores indicating a greater burden of AA on the patient.
The EQ-5D-5L is a standardised measure of general health status that comprises a visual analogue scale (VAS) and a short questionnaire [20]. The VAS records respondents’ self-rated health scores, ranging from 0 (worst) to 100 (best imaginable state of health). The descriptive component includes five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression [21]. Each dimension has five levels, ranging from no problems to extreme problems. The EQ-5D-5L index score is generated from the responses provided for the descriptive component and ranges from 0 to 1, with higher scores indicating better health status. The EQ-5D-5L index scores reported in this manuscript were derived from the UK value set [22].
The HADS was used to measure symptoms of anxiety (HADS-A) and depression (HADS-D) [23]. It is comprised of seven questions for anxiety and seven questions for depression, with the two sub-scales scored separately. Each sub-scale score ranges from 0 to 21, with scores of 0–7 being considered normal, 8–10 borderline abnormal and 11–21 abnormal.
The WPAI assessed the effect of AA on work productivity (employed respondents only) and regular activities (all respondents) over the past 7 days [24]. The WPAI consists of six questions and four scores are derived: absenteeism (percentage of work time missed due to AA), presenteeism (percentage of reduced productivity while at work), work productivity loss (score that combines absenteeism and presenteeism) and activity impairment (percentage of impairment in regular activities performed outside of work). Each score ranges from 0 to 100, with greater scores indicating greater impairment. The translated AA General Health versions of the WPAI Version 2.0 were used in this study [25].
Statistical Analysis
Demographics, clinical characteristics and PROs were analysed descriptively according to physician-assessed severity of AA (i.e. mild, moderate and severe). Continuous variables were described using mean and standard deviation (SD). Categorical variables were reported as the frequency and percentage within each category. Concordance between patient and physician ratings of AA severity was assessed using Kappa analysis, a measure of interobserver reliability. A kappa statistic with a value of 1 indicates perfect agreement between pairs of ratings, while a value of zero indicates a level of agreement equivalent to chance. For intermediate kappa values, interpretation ranges from < 0.0 (i.e. poor) to 0.81–1.00 (i.e. almost perfect) [26]. Statistical tests were conducted to determine whether differences in PROs between physician-reported severity groups were statistically significant, with p < 0.05 considered significant (p values were not multiplicity controlled). Analysis of variance F-test was used for continuous variables and Kruskal-Wallis was used for ordinal variables. For each analysis, data were reported as observed. Where answers were not stated for patient-reported data, these patients were removed from the descriptive analysis. All analyses were conducted using Stata Version 17 [27].
Results
Patient Demographics and Clinical Characteristics (as Reported by Physicians)
A total of 239 physicians provided data on 2083 patients (mild AA n = 299; moderate AA n = 936; severe AA n = 848), of whom 561 completed a PSC and were included in this study. Most PSCs (61.0%) were completed by patients from Germany, followed by Spain (26.6%). The overall mean ± SD age of patients who completed a PSC was 34 ± 11 years, 44% were female and 74% were employed (full or part time) at the time of the survey (Table 1).
The mean time since AA diagnosis was slightly longer for patients with physician-assessed severe AA (2.9 years) than for patients with moderate (2.4 years) or mild AA (2.3 years; Table 1). Disease progression was judged by physicians as uncontrolled (i.e. stable or worsening) in 40.8%, 57.6% and 74.3% of patients with mild, moderate and severe AA, respectively. The mean number of current AA-related symptoms increased with disease severity, being 1.3 in patients with mild AA, 2.1 in those with moderate AA and 3.0 in patients with severe AA (Table 1). Scalp hair loss was the primary physician-reported symptom reported across all severity groups (in 70.4% with mild AA, 87.7% with moderate AA and 88.2% with severe AA) (Fig. 1). A higher percentage of patients with severe AA, compared with mild or moderate AA, were currently reported to have hair loss in other areas; the most common locations in the severe group were eyebrows (39.6%), eyelashes (28.3%) and body (22.5%). Concomitant conditions (i.e. medical conditions other than AA) were more frequently reported for patients with moderate or severe AA than for those with mild AA (Table 1).
Agreement Between Physician and Patient on Current Disease Severity
Data for the alignment between patient- and physician-reported severity of AA were available for 549 patients. In 78.5% of cases with available data, there was alignment between patient- and physician-rated severity of AA (Table 2). In 15.7% of cases, the physician reported a higher degree of severity than their patient, and in 5.8% the patient reported higher severity than their physician. This level of agreement was substantial (kappa = 0.67, p < 0.001).
Patient-Reported Outcomes
Skindex-16 AA
Mean Skindex-16 AA scores increased (worsened) with physician-assessed AA severity for each of the three scales, Symptoms, Emotions and Functioning (all p < 0.001; Fig. 2). The Emotions scale had the highest (i.e. worst) scores across severity categories.
Mean (SD) patient-reported Skindex-16 AA scale scores by physician-rated AA severity. Higher scores for Skindex-16 AA indicate greater burden; p values are based on analysis of variance F-test for differences between severity groups. AA alopecia areata, SD standard deviation, Skindex-16 AA Skindex-16 adapted for AA
EQ-5D-5L
Mean EQ-5D-5L VAS and index scores decreased with increasing physician-assessed AA severity, showing poorer overall health status (both p < 0.001; Fig. 3). The levels of perceived problems increased with disease severity in the dimensions of anxiety/depression (p < 0.001), pain/discomfort (p < 0.001) and usual activities (p < 0.001). Anxiety/depression was the dimension with the highest percentages of patients reporting any perceived problem: 44.3% of patients with mild, 49.1% with moderate and 66.5% with severe AA reported feeling anxious and/or depressed on the day of their consultation.
Patient-reported health status (EQ-5D-5L scores) by physician-rated AA severity. a Mean (SD) EQ-5D-5L VAS scores. b Mean (SD) EQ-5D-5L index scores. c EQ-5D-5L descriptive component. Higher EQ-5D-5L VAS and index scores indicate better health; p values are based on analysis of variance F-test (VAS and index scores) or Kruskal-Wallis (descriptive component responses) for differences between severity groups. AA alopecia areata, EQ-5D-5L EuroQoL-5-dimension-5-level questionnaire, SD standard deviation, VAS visual analogue scale
HADS
The proportion of patients with borderline abnormal or abnormal HADS scores (scores ≥ 8) for both anxiety and depression increased with increasing physician-assessed AA severity (both p < 0.001; Fig. 4). This was mostly related to an increase in the percentages of patients with an abnormal score (11–21).
Proportion of patients with borderline/abnormal HADS Anxiety and Depression scores (scores ≥ 8). HADS data were patient-reported; AA severity levels are as per physician assessment; p values are based on Kruskal-Wallis for differences between severity groups. AA alopecia areata, HADS Hospital Anxiety and Depression Scale
WPAI
Overall, patients’ activity both inside and outside of work showed greater impairment with increasing physician-rated severity of AA (p < 0.001 for presenteeism, activity impairment and overall work impairment; Fig. 5). Across severity groups, work productivity loss was primarily driven by reduced productivity while at work (presenteeism).
Mean (SD) percentage WPAI activity or work impairment due to AA. WPAI data were patient-reported; AA severity levels are as per physician assessment; p values are based on analysis of variance F-test for differences between severity groups. AA alopecia areata, SD standard deviation, WPAI Work Productivity and Impairment Questionnaire
Discussion
This study provides real-world data regarding the burden of AA from a large population of patients in Europe. Our analysis showed that the patient-reported burden of AA increased with physician-assessed disease severity. This may reflect that the physicians’ assessments of disease severity in this study were made according to overall clinical judgment rather than a definition based only on the extent of hair loss and that there was 78.5% concordance observed between physicians and patients for the assessment of disease severity. Physician’s understanding of the full patient burden of AA beyond hair loss is important to ensure the appropriate treatment and support is given.
There is conflicting evidence in the literature on the relationship between severity of hair loss and burden of AA on patients [2, 10,11,12,13,14,15,16]. Previous studies have reported an underestimation of disease severity by physicians and highlighted the need to consider psychosocial factors and QoL [10, 11, 13]. For example, a study that showed poor correlation between Physician Global Assessment and Patient Global assessment data (weighted Cohen’s kappa 0.16 for alopecia) noted the importance of physicians considering the patient’s perception of severity in making treatment decisions and evaluating clinical factors [10]. Interestingly, several studies have also shown that physician-rated severity of scalp hair loss (using the SALT) was not a reliable predictor of QoL impairment in AA [11, 13, 16]. On the other hand, patients’ hair loss severity rating (using a self-administered hair loss severity questionnaire) correlated more strongly with their QoL (using Skindex-16) compared with physicians’ ratings [11]. Some discordance in disease severity assessment was observed in our study, but in 15.7% of cases the severity rating of the patient was lower than that of the dermatologist, while only 5.8% of patients reported a higher degree of severity than their physician. This difference from previous studies might be related to the definition of severity. Similar findings were reported from the AA DSP in Japan, which found a moderate level of agreement between patients and physicians on the overall disease severity (76% of cases, kappa coefficient 0.60, p < 0.001), with higher severity reported by physicians in 15% of cases and by patients in 9% of cases [12]. A recent report highlighted that the relationship between AA severity and its impact is complex and not yet fully understood [17]. In this US survey, a greater QoL impact was reported by people with moderate (21–49%) or large (50–94%) areas of scalp hair loss versus those with those with 95–100% hair loss, possibly suggesting those with nearly all or total scalp hair loss had adapted to living with AA [17].
Our findings of the impact of psychosocial as well as clinical factors on AA severity ratings are in alignment with those previously reported from the AA DSP based on physician clinical judgement in Japan and patient-reported severity in the USA [12, 13], with all three studies showing a greater QoL impact of the emotional aspects of hair loss than physical symptoms. Across the three physician-assessed AA severity groups in the current study, the Symptoms domain was the Skindex-16 AA scale with the lowest scores, indicating less burden than that reported for the other domains. Previous research suggests that physical symptoms of skin discomfort, such as itching or burning, are less commonly reported than psychological burden by patients with AA [28]. Accordingly, the greater impairment observed in the Emotions and Functioning scales of Skindex-16 AA is consistent with the profound emotional and psychological burden reported in the literature for patients with AA [28,29,30].
Anxiety/depression and pain/discomfort were the most affected EQ-5D-5L dimensions across the three physician-assessed AA severity groups, both of which worsened with increasing AA severity. Minimal impact was seen on the other EQ-5D-5L dimensions, which seems consistent with the age of the respondents and the limited physical impact of AA beyond hair loss. A multicentre, cross-sectional study conducted across 13 European countries also reported a significantly greater impact on the depression/anxiety domain among patients with AA, compared with people without a skin disease [31].
The mental health burden of AA was further illustrated by data from the HADS. We observed that the percentage of patients with borderline abnormal or abnormal HADS-A and HADS-D scores increased with physician-assessed AA severity, with the increase according to severity being particularly apparent for abnormal HADS scores. This observation is aligned with the results reported from the AA DSP in Japan [12] and reflects that people with (vs without) AA have a higher risk of experiencing mental health disorders, such as anxiety and depression [3, 30, 32]. HADS data were not collected in the US DSP [13].
The effect of AA on work productivity and daily activities was assessed using the WPAI [24], and findings showed the association between higher physician-assessed AA severity and burden was also accompanied by reduced work productivity and increased daily activity impairment. Similar WPAI results (i.e. reduced productivity and greater impairment with higher physician-assessed AA severity) in patients with AA have also been observed in the USA and Japan [12, 33], although in the US DSP study assessing predictors of QoL this association not observed based on physician-assessed SALT score but greater presenteeism was associated with current patient-rated severe AA [13].
Although this study provides real-world data regarding the symptom, QoL and mental health burden of AA from a large population of patients in Europe, it is subject to the limitations associated with real-world studies, such as the potential for sampling, selection and recall bias. The cross-sectional design and descriptive nature of our study do not allow us to conclude on causality. As physician-assessed AA severity was based on clinical judgement, this may vary between physicians. However, as there is no universally accepted definition of disease severity for AA, we believe this approach should reflect how physicians assess AA severity in real-life clinical practice. Another limitation of this study was that only a quarter of patients provided PRO data, although this still gave a large sample of > 500 patients. The results may also have been influenced by patient and physician characteristics, such as gender, and further research into potentially confounding factors is needed. Finally, due to enrolment challenges, there was a limited number of patients from France, Italy and the UK, with most PSCs completed by patients in Germany (61.0%) and Spain (26.6%), which could limit the generalisability of the study findings to other European countries. Nevertheless, we believe that our results are of interest as similar data were reported in two separate AA DSP studies in the USA and Japan [12, 13], suggesting the burden of AA affects patients globally.
Conclusions
Proper evaluation of AA disease severity and burden on patients is essential to inform appropriate treatment strategies. This large European study found a substantial physician–patient alignment on AA severity assessment. Higher physician-rated disease severity was associated with larger patient-reported disease burden, including greater levels of anxiety and depression, and more pronounced work and activity impairment. These findings highlight the significant impact that AA can have beyond hair loss, especially for patients with severe AA.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lintzeri DA, Constantinou A, Hillmann K, Ghoreschi K, Vogt A, Blume-Peytavi U. Alopecia areata—current understanding and management. J Dtsch Dermatol Ges. 2022;20:59–90.
Muntyanu A, Gabrielli S, Donovan J, et al. The burden of alopecia areata: a scoping review focusing on quality of life, mental health and work productivity. J Eur Acad Dermatol Venereol. 2023. https://doi.org/10.1111/jdv.18926.
Macbeth AE, Holmes S, Harries M, et al. The associated burden of mental health conditions in alopecia areata: a population-based study in UK primary care. Br J Dermatol. 2022;187:73–81.
Toussi A, Barton VR, Le ST, Agbai ON, Kiuru M. Psychosocial and psychiatric comorbidities and health-related quality of life in alopecia areata: a systematic review. J Am Acad Dermatol. 2021;85:162–75.
Messenger AG, McKillop J, Farrant P, McDonagh AJ, Sladden M. British Association of Dermatologists’ guidelines for the management of alopecia areata 2012. Br J Dermatol. 2012;166:916–26.
Baricitnib EU SPC. https://www.ema.europa.eu/en/medicines/human/EPAR/olumiant. Accessed 26 Jul 2023.
Baricitinib US Prescribing Information. https://pi.lilly.com/us/olumiant-uspi.pdf. Accessed 26 Jul 2023.
Ritlectinib US Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215830s000lbl.pdf. Accessed 26 Jul 2023.
King BA, Senna MM, Ohyama M, et al. Defining severity in alopecia areata: current perspectives and a multidimensional framework. Dermatol Ther (Heidelb). 2022;12:825–34.
Tabolli S, Sampogna F, Pagliarello C, Paradisi A, Spagnoli A, Abeni D. Disease severity evaluation among dermatological out-patients: a comparison between the assessments of patients and physicians. J Eur Acad Dermatol Venereol. 2012;26:213–8. https://doi.org/10.1111/j.1468-3083.2011.04038.x.
Reid EE, Haley AC, Borovicka JH, et al. Clinical severity does not reliably predict quality of life in women with alopecia areata, telogen effluvium, or androgenic alopecia. J Am Acad Dermatol. 2012;66:e97-102.
Edson-Heredia E, Aranishi T, Isaka Y, Anderson P, Marwaha S, Piercy J. Patient and physician perspectives on alopecia areata: a real-world assessment of severity and burden in Japan. J Dermatol. 2022;49:575–83.
Senna M, Ko J, Glashofer M, et al. Predictors of QOL in patients with alopecia areata. J Invest Dermatol. 2022;142:2646–50.
Anderson P, Benford M, Harris N, et al. Real-world physician and patient behaviour across countries: disease-specific programmes—a means to understand. Curr Med Res Opin. 2008;24:3063–72.
Abedini R, Hallaji Z, Lajevardi V, Nasimi M, Karimi Khaledi M, Tohidinik HR. Quality of life in mild and severe alopecia areata patients. Int J Womens Dermatol. 2017;4(2):91–4.
Vélez-Muñiz RDC, Peralta-Pedrero ML, Jurado-Santa Cruz F, Morales-Sánchez MA. Psychological profile and quality of life of patients with alopecia areata. Skin Appendage Disord. 2019;5(5):293–8.
Gelhorn HL, Cutts K, Edson-Heredia E, et al. The relationship between patient-reported severity of hair loss and health-related quality of life and treatment patterns among patients with alopecia areata. Dermatol Ther (Heidelb). 2022;12(4):989–97.
European Pharmaceutical Market Research Association. 2022 Code of Conduct. Basel: European Pharmaceutical Market Research Association; 2022. https://www.ephmra.org/sites/default/files/2022-08/EPHMRA%202022%20Code%20of%20Conduct.pdf. Accessed 30 Jan 2023.
Chren M-M, Lasek RJ, Sahay AP, Sands LP. Measurement properties of Skindex-16: a brief quality-of-life measure for patients with skin diseases. J Cutan Med Surg. 2001;5:105–10.
EuroQol Group 2022. EQ-5D-5L—About. https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/. Accessed 25 Apr 2023.
EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy Amst Neth. 1990;16:199–208.
Hernández Alava M, Pudney S, Wailoo A. Estimating the relationship between EQ-5D-5L and EQ-5D-3L: results from an English population study [EEPRU Report]. 2020, University of Sheffield & University of York. https://www.nice.org.uk/Media/Default/About/what-we-do/NICE-guidance/estimating-the-relationship-betweenE-Q-5D-5L-and-EQ-5D-3L.pdf. Accessed 23 May 2023.
Zigmond AS, Snaith RP. The Hospital Anxiety And Depression Scale. Acta Psychiatr Scand. 1983;67:361–70.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–65.
Reilly Associates 2020. WPAI: Alopecia Areata, Version 2.0. Updated January 2020. http://www.reillyassociates.net/WPAI_Translations.html#anchor_513. Accessed 25 Apr 2023.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
StataCorp. Stata statistical software: release 17. College Station: StataCorp LLC; 2021.
Aldhouse NVJ, Kitchen H, Knight S, et al. “‘You lose your hair, what’s the big deal?’ I was so embarrassed, I was so self-conscious, I was so depressed”: a qualitative interview study to understand the psychosocial burden of alopecia areata. J Patient Rep Outcomes. 2020;4:76.
van Dalen M, Muller KS, Kasperkovitz-Oosterloo JM, Okkerse JME, Pasmans SGMA. Anxiety, depression, and quality of life in children and adults with alopecia areata: a systematic review and meta-analysis. Front Med (Lausanne). 2022;29(9):1054898.
Okhovat J-P, Marks DH, Manatis-Lornell A, Hagigeorges D, Locascio JJ, Senna MM. Association between alopecia areata, anxiety, and depression: a systematic review and meta-analysis. J Am Acad Dermatol. 2023;88:1040–50.
Balieva F, Kupfer J, Lien L, et al. The burden of common skin diseases assessed with the EQ5D™: a European multicentre study in 13 countries. Br J Dermatol. 2017;176(5):1170–8.
Lee S, Lee H, Lee CH, Lee W-S. Comorbidities in alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80:466–77.e16.
Gandhi K, Shy ME, Ray M, Fridman M, Vaghela S, Mostaghimi A. The association of alopecia areata-related emotional symptoms with work productivity and daily activity among patients with alopecia areata. Dermatol Ther (Heidelb). 2023;13:285–98.
Acknowledgements
The authors thank the patients and physicians who participated in this survey.
Medical Writing/Editorial Assistance
Medical writing support was provided by Claire Lavin and Caroline Spencer on behalf of Rx Communications, funded by Eli Lilly and Company.
Funding
The study was funded by Eli Lilly and Company. Eli Lilly and Company also provided funding for the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
All authors (Sergio Vañó-Galván, Ulrike Blume-Peytavi, Paul Farrant, Pascal Reygagne, Erin Johansson, Catherine Reed, Simran Marwaha, Frederick Durand and Bianca Maria Piraccini) contributed to study conception and design. Formal analysis and investigation: Simran Marwaha. Writing—original draft preparation: Erin Johansson, Simran Marwaha, Frederick Durand. All authors (Sergio Vañó-Galván, Ulrike Blume-Peytavi, Paul Farrant, Pascal Reygagne, Erin Johansson, Catherine Reed, Simran Marwaha, Frederick Durand and Bianca Maria Piraccini) contributed to review and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Sergio Vañó-Galván is an advisor for Pfizer and Eli Lilly and Company. Ulrike Blume-Peytavi has served on advisory boards and/or is a consultant and/or is a clinical trial investigator for AbbVie, Amryt, Bayer, Boots Healthcare, Cassiopeia, CeraVe, Concert Pharmaceuticals, Dermocosmétique Vichy, Eli Lilly and Company, Galderma, LEO Pharma, Mayne Pharma Neuroderm, Novartis, Pfizer, Pierre Fabre and Sanofi Regeneron. Paul Farrant is a clinical researcher and advisory board member for Pfizer and an advisor for Eli Lilly and Company. Pascal Reygagne has nothing to declare. Erin Johansson, Catherine Reed, and Frederick Durand are employees and shareholders of Eli Lilly and Company. Simran Marwaha is employee of Adelphi Real World. Bianca Maria Piraccini is an advisor for Almirall, Eli Lilly and Company, ISDIN, Pfizer and Vichy.
Ethical Approval
The Disease Specific Programme (DSP) fulfils the definition of a market research survey under the European Pharmaceutical Marketing Research Association (EphMRA) Code of Conduct and is therefore conducted to market research guidelines rather than clinical guidelines [18]. Market research surveys are exempt from requiring Institutional Review Board (IRB) approval; however, the Western IRB conducted a methodological review of the Alopecia Areata DSP and provided an exemption. The DSP was conducted in compliance with the International Council for Harmonisation Declaration of Helsinki. Each respondent provided freely given, specific and informed consent to take part in the DSP and for the processing of their personal data. All data provided by physicians and patients were anonymised.
Additional information
Prior Presentation: Interim data from this manuscript have been presented in part as a poster at the First Barcelona Hair Meeting, 29 September to 1 October 2022 and as a poster at ISPOR Europe 2022, 6–9 November 2022.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Vañó-Galván, S., Blume-Peytavi, U., Farrant, P. et al. Physician- and Patient-Reported Severity and Quality of Life Impact of Alopecia Areata: Results from a Real-World Survey in Five European Countries. Dermatol Ther (Heidelb) 13, 3121–3135 (2023). https://doi.org/10.1007/s13555-023-01057-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01057-0