Abstract
Introduction
Atopic dermatitis (AD) is a chronic, pruritic skin disease caused by a mixture of genetic, immunological, and environmental factors, characterized by periods of inflammation and remission. In Latin America (LA), the prevalence of AD ranges up to 25% in children and 1–3% in adults. The natural history of the disease for most patients is that AD goes into remission in adolescence and adult life. Only 10–30% of patients continue to have symptoms of the disease in adulthood. There are patients (3–4%) who have the onset of AD during adolescence or after adulthood. Those with limited access to healthcare services, such as diagnosis and treatment, have increased difficulties coping with AD. Healthcare disparities are a complex topic that include social, political, racial/ethnic, and geographical factors. Publications about healthcare disparities in AD in LA are scarce. As a result, recognizing and resolving healthcare inequalities is critical to improving the treatment and quality of life (QoL) of individuals with AD.
Methods
A panel of Latin American experts in dermatology and allergies was provided with a series of relevant questions to address before a multiday conference. During this conference, the entire group discussed and edited each narrative through numerous drafts and rounds of discussion until they reached a consensus.
Results
This paper examines the barriers to equal access to care and recommends realistic actions to overcome them. Inadequate disease knowledge, cultural and linguistic barriers, stigmatization, maldistribution of resources, absence of local clinical practice guidelines, arduous patient journey, and limited consultation time were identified as causes of health inequality.
Conclusions
Among the suggested solutions are enhanced education for healthcare professionals, patients, and the general public, a focus on underprivileged communities, telemedicine and telementoring, translators, multidisciplinary teams, and local living clinical practice guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Healthcare disparities are a multifaceted issue that include socioeconomic, political, ethnic/racial, and regional factors |
Publications about healthcare disparities in atopic dermatitis (AD) in Latin America (LA) and other parts of the world are scarce, and identifying and addressing healthcare disparities is critical to improving the care and quality of life (QoL) of patients with AD |
To create this narrative review, a panel of pediatric allergists and dermatologists were convened by AHF and spent 3 days reviewing the literature and discussing their real-world experience to address barriers for health equity in AD and suggest steps to overcome them |
Many factors impact QoL for people with atopic dermatitis, and the impact is greater for those who are less educated, earn less money, and live in poorer neighborhoods |
The authors propose collaborative networks among LA countries, local living guidelines, extension programs from colleges that interact with people who have cultural or language barriers, fostering patient education programs, and using technology, specifically telemedicine, to reach patients to reduce health disparities in LA |
Introduction
Atopic dermatitis (AD) is a chronic, pruritic, multifactorial, and heterogeneous inflammatory skin disease involving genetic, immunological, and environmental factors, characterized by periods of exacerbation and remission. AD occurs predominantly in childhood but can also affect adults, and the disease is not limited to patients of a specific gender or ethnicity. A family history of atopic diseases is a strong predictor of AD, indicating that genetic factors play a role in its development [1]. The multifaceted etiology of AD includes defects in the skin barrier, skin dysbiosis, and a dysregulated immune system [2]. About one-third of people with AD also have allergic manifestations like asthma, food allergies, rhinitis, and conjunctivitis [3, 4]. Besides skin lesions, AD is linked to various systemic inflammatory illnesses, sleep disturbances, neuropsychiatric disorders, and increased risk of cardiovascular disease [5, 6].
In Latin America (LA), the prevalence of AD ranges from 5% to 25%. Studies reported that 60–70% of cases develop during the first year of life, and 90% of all cases are diagnosed in the first 5 years. In 2004, the International Study of Asthma and Allergies in Childhood (ISAAC) established the prevalence of AD between 5% and 10% in children aged 6 and 7 years in LA [7]. The natural history of the disease for most patients is that AD goes into remission in adolescence and adult life. However, 10–30% of patients continue to have symptoms of the disease in adulthood, and in some patients (3–4%) the onset of AD is during adolescence or after adulthood. AD prevalence in adults is 1–3% [8,9,10,11].
Healthcare disparity is a complex issue encompassing socioeconomic, political, ethnic/racial, and regional factors. Publications about healthcare disparities in AD in LA and other parts of the world are scarce. Therefore, identifying and addressing healthcare disparities is of utmost importance to improve the care and quality of life (QoL) of patients with AD.
The issue of healthcare disparity has been gaining momentum, likely due to the COVID-19 pandemic, increasing socioeconomic inequality and ethnic/racial tensions around the world. The term “health disparity” was coined in the USA around 1990 and denoted a specific disparity: substandard health in disadvantaged racial/ethnic groups [12]. However, beyond the racial/ethnic and sociopolitical perspective, the Agency for Healthcare Research and Quality (AHRQ) defines healthcare disparities in broader terms as “differences in access to or availability of medical facilities and services, and variation in rates of disease occurrence and disabilities between population groups defined by socioeconomic characteristics such as age, ethnicity, economic resources, or gender and populations identified geographically” [13]. This definition encompasses the complexity of healthcare disparity with its implications and interconnections. This paper aims to examine the barriers to equal access to care for AD in LA and recommend realistic actions to overcome them.
Methods
The Americas Health Foundation (AHF) gathered a panel of six pediatric dermatologists and allergists from Argentina, Brazil, Colombia, Chile, Mexico, and Uruguay. They held a 3-day conference on 20–22 April 2022 to generate proposals for reducing the disparities in access to AD diagnosis and treatment in LA. AHF searched PubMed, MEDLINE, and EMBASE for AD-published allergists and dermatologists in LA. AHF supplemented this search by contacting thought leaders in the LA medical community to ensure that the list appropriately reflected the relevant areas. This manuscript’s authors include all the specialists who attended the conference.
The authors researched AD through PubMed, MEDLINE, and EMBASE. “Treatment,” “diagnosis,” “quality of life,” “patient journey” in combination with “Latin America,” “atopic dermatitis,” “inequity,” and “health disparities” were searched with dates ranging from 01/01/2016 until 2/10/2022. The articles identified were in English, Portuguese, and Spanish. Literature and research from LA were prioritized.
AHF prepared specific questions to address health inequities that restricted access to AD diagnosis and treatment in LA and allocated one to each panel member. Individual panel members submitted written responses to their questions on the basis of the literature and their knowledge. During the 3-day meeting, the panel scrutinized and modified each account through multiple debate rounds until all panelists agreed. The panel unanimously endorsed the recommendations on the basis of the facts obtained, professional opinion, and personal experience. The completed paper was sent to the panel for evaluation and approval after the conference. The authors maintain editorial control over the paper’s content. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Impact on Quality of Life (QoL) for Patients with Atopic Dermatitis
Neuropsychological and Emotional Impact
The symptoms associated with AD, pruritus being the most common, profoundly impact the QoL of patients and their caregivers, affecting sleep quality and impairing school and work productivity. Anxiety, depression, ADHD, suicidal ideation, and sleep deficit disorder are just a few neuropsychological symptoms patients with AD can experience. [14, 15].
Economic Impact
The economic impact of AD is directly related to disease severity. There are considerable disparities in LA regarding drug costs and healthcare access [16]. In Colombia, Mexico, and Peru, the expenses per patient in 2021 for topical treatment, systemic steroids, absenteeism, laboratory tests, and medical appointments ranged from US $443.00 to US $6360.50, not including biological treatments or immunosuppressants [17].
Environmental Factors
Climate and geography in LA are variable, with broad temperature and humidity ranges, and recent evidence shows that climate change may influence AD prevalence and severity [10, 18]. Air pollution, factory emissions, and water hardness have been associated with an increased frequency of AD and other allergic diseases [19, 20]. Children living near factories in Buenos Aires, Argentina, were twice as likely to have AD [21, 22].
Discussion
Ways to Improve QoL
Guidelines in Place to Aid Healthcare Professionals
Despite advances in our understanding of the pathogenesis of AD and the introduction of new treatments, managing this disease remains a challenge for both patients and doctors. To this day, AD is a disease that continues to have multiple names and many diagnostic and severity criteria. It is not surprising that AD care and treatment standards vary widely.[23,24,25] This variability has led experts worldwide to emphasize the need to harmonize AD diagnosis, outcome measures, treatments, and other topics, resulting in an upsurge of consensus meetings, reports, and clinical practice guidelines (CPGs) [26, 27]. In recent years, the quantity of CPGs has led to the generation of systematic reviews of AD CPGs to evaluate their quality, similarities, discrepancies, and applicability [26]. These reviews have shown that “not all guidelines are created equal,” and many have divergent recommendations, suffer from bias, lack applicability, and have recommendations that are not evidence based.
LA has not been an exception to increased AD research and development [17]. Several CPGs exist in the region for diagnosing and treating AD, including a multinational guideline by the Latin America Allergy, Asthma and Immunology Society (SLAAI), and national guidelines in Mexico, Colombia, Argentina, and Brazil [28,29,30,31,32,33].
Lack of consistent guideline implementation results in underestimation or overestimation of AD diagnosis. Although all guidelines recommend topical steroids as the primary symptomatic treatment for AD, researchers discovered that, particularly in managing children, primary care physicians (PCPs) and their caregivers had a fear of corticosteroids (corticophobia) negatively affecting the control of AD symptoms [34]. Researchers reported that PCPs provided heterogeneous care for AD; for example, many performed unnecessary food restrictions, impacting children’s nutrition [35].
Access to Therapeutics
Health disparities disproportionately affect patients in underserved groups, and these disparities are linked to economic, environmental, and social disadvantages. Physicians’ academic training may not always consider the characteristics of disadvantaged racial and ethnic groups. [36] More robust educational opportunities are needed to fully equip trainees with tools to recognize and develop effective strategies to reduce the burden of health disparities. The segregation of groups by race, culture, or geographic location generates limitations in access to the healthcare system, and restricted access seems to result in more severe forms of the disease [37, 38].
AD management should follow a comprehensive, stepwise approach tailored to disease severity. First-line management involves educational programs, psychosocial support, appropriate skincare, avoidance of triggers, antimicrobials, antiseptics, topical corticosteroids (TCS), and other agents such as topical calcineurin inhibitors (TCI). Second-line management includes phototherapy, especially ultraviolet (UV) A and narrowband ultraviolet B (NBUVB), and intensive topical treatment. Most AD cases are controlled by limiting exacerbating factors, maintaining proper skin care, and using topical treatments [28, 30, 33, 39,40,41,42]. However, for severe or non-respondent disease, systemic immunosuppressants, biologics, and inhibitors of Janus kinases (JAK) may be needed. As more effective, targeted treatments emerge, correct diagnosis and an appropriate assessment of severity are essential to determining the best strategies for control.
Skin Care Measures
Appropriate skin care is essential for all patients with AD [28, 30, 33, 39, 41,42,43]. Regular moisturizer use increases skin hydration [44,45,46] and may reduce the dose of antiinflammatory treatments, such as TCS, required for disease control [46, 47]. Soap substitutes, including synthetic detergents (syndets) with neutral or acidic pH and mild surfactants, minimize the damage to skin proteins and lipids induced by regular alkaline soaps [48, 49]. However, in some countries in LA, skin care products such as emollients and soap substitutes are not regularly covered by the healthcare system (Table 1a).
Topical Antiinflammatory Therapy
TCS are considered the mainstay of antiinflammatory therapy in AD, especially in managing acute flare-ups, but also in proactive, intermittent use as maintenance therapy. However, the availability of TCS may be limited in LA countries, particularly in public healthcare (Table 1a).
When TCS are not well tolerated or in locations such as the face or neck, TCI (e.g., tacrolimus and pimecrolimus) may be prescribed. TCI has proven efficacy in AD in active and proactive treatment. [50,51,52] Like TCS, the availability of TCI may be restricted in some LA countries, especially in public healthcare. (Table 1a).
Treatment for Moderate-to-Severe AD
Upscaling to phototherapy or systemic agents is indicated if the condition does not respond to topical treatment.
Phototherapy
Phototherapy is recommended as second-line or adjuvant therapy in patients with moderate-to-severe AD, especially in adults and older children.[53] The best efficacy was NBUVB (311–313 nm) and UV A-1 (340–400 nm) [54,55,56].
Phototherapy is not easily accessible in LA, and there is limited equipment availability, primarily due to high costs. This office-based therapy is only offered in some public hospitals and private centers, and it is often not convenient for those patients who live far away from a phototherapy facility (Table 1a).
Systemic Immunosuppressant Agents
Third-line treatments for moderate-to-severe AD include cyclosporine, methotrexate, azathioprine, and mycophenolate mofetil [43, 57]. When prescribing systemic immunosuppressant agents (SIS), many variables must be considered, including comorbidities and baseline laboratory results. SIS are associated with potentially severe adverse effects and require strict clinical and laboratory monitoring. Therefore, candidates for systemic therapy must be carefully selected. Sharing information about treatment efficacy and potential side effects with the patient and caregivers is also very important. Appropriate indication and follow-up for SIS require considerable time, which may limit their use. In addition, the high cost of some of these agents [57] may limit their use in some LA countries, especially in public hospitals and rural healthcare facilities (Table 1b).
Biologics and Small-Molecule Therapies
Several emerging therapies show efficacy and short-term safety that are potentially superior to traditional SIS. Systemic biologic therapy, like dupilumab and other agents, as well as small-molecule agents, such as JAK inhibitors, are appropriate in moderate and severe AD to improve disease response and QoL and limit disease progression [58, 59].
Dupilumab is available in several countries in LA, but in some of them it is not approved for AD or not approved for pediatric use. Similarly, only a few LA nations have approved JAK inhibitors, and their high expense further limits who has access to them. Also, most healthcare systems require an objective instrument to quantify disease to access high-cost medications. This is an additional limitation because most physicians in LA are not trained in applying AD scoring methods [28]. The accessibility to new and expensive therapies for AD, and their impact on the healthcare systems in LA, will have to be addressed.
Access to PCPs and Specialists if Necessary
Two objectives in the clinical management of AD are achieving clinical control and preventing complications. These objectives are achieved with adequate patient access to health networks [60, 61]. PCPs are usually trained to diagnose and treat the most prevalent diseases in their clinical practice. So, they rely on specialists, especially for severe or difficult-to-treat cases.
Access to AD specialists in LA appears to be limited [62]. Factors affecting access include lack of specialists, high patient volume, time constraints, economic barriers, lack of patient knowledge to consult about AD, or PCPs’ lack of awareness of AD. Difficulty accessing specialists becomes a barrier to controlling AD, which hurts patient treatment. A better understanding of the causes of this access issue could be the first step to proposing practical solutions.
Barriers Leading to Health Disparity and Lower QoL in People with AD.
Barriers to Specialist Access
Our extensive literature search in Spanish, Portuguese, and English yielded just eight papers on barriers to accessing the healthcare system in LA, none of which were specific to AD. Despite this, the identified papers provided insight into possible access barriers to AD specialists. Access to the healthcare system in Latin American countries is diverse and uneven [63]. In some countries, registration with the national health system is mandatory, so 100% of the population has at least a primary healthcare network to access regardless of income [64]. In other Latin American countries, registration is not required [64].
Most LA countries have a mixed (public and private) healthcare system. Depending on the country, public access to a specialist involves meeting several requirements, generating access inequality between populations [63].
In all countries in LA, access to specialists by private practice is available [63] but in some countries, the public healthcare system (PHS) allows access to PCPs and specialists only upon referral. In contrast, in others, the PHS has additional restrictions on access to specialists, for example, only in medical emergencies [16] As most countries in LA have a low or medium per capita income, patient cost is often a barrier to correct AD management[65].
Sometimes cultural, geographic, and social characteristics impede access to healthcare. Although countries such as Brazil and Colombia have a public healthcare network, its use varies according to whether the person lives in a rural or urban area [66, 67]. Access to healthcare centers in rural areas is a challenge, presumably due to centers being more distant and patients needing to take additional unpaid time off from work with added travel expenses. Some ethnic groups in closed communities seem to have less confidence in the medical treatments offered by the state, especially among the native communities that are abundant in LA and prefer to use traditional medicine [68,69,70]. In addition, language and cultural barriers exist in certain communities because the needs or the way of approaching the problem may differ from what the treating physician has in mind [71].
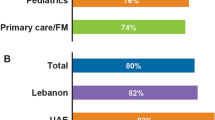
One of the panelists surveyed allergists and dermatologists from LA in a convenience sample taken between March and April 2022 to better understand their perception of AD management in Latin American countries. An overwhelming majority of those surveyed (98.3%) did not believe PCPs or first points of contact are sufficiently trained to diagnose AD and recognize appropriate referral situations. About one-third of those surveyed (35%) perceived that there are insufficient allergists and dermatologists to cover the demand for patients with AD in LA.
According to reports from allergy and dermatology societies in LA, the number of specialists per 100,000 inhabitants was highly variable [17], with dermatologists ranging from 1.2 in Mexico to almost 9.2 in Uruguay, while allergists ranged from 0.2 in Peru to 5.7 in Argentina. These heterogeneous results are partly due to the lack of training in medical schools in some countries.
In each country in LA, the ideal number of medical specialists depends on several factors. The barriers to access previously discussed mean that some populations cannot access specialists. On the other hand, in countries with a robust healthcare system that makes it easier to overcome these barriers, there will be more patients diagnosed who need to be managed for their AD. Therefore, a higher number of doctors are required to care for them.
Despite significant advances in understanding AD pathophysiology and new drugs and treatments, AD management remains challenging for patients and doctors. Patients with AD and their caregivers are often confused and frustrated by the information they receive from healthcare providers (HCPs) and online sources.
Online surveys in Argentina and Brazil showed that 40% and 80% of patients with AD and their caregivers expressed dissatisfaction with their treatment. Patients complained that doctors do not know how to manage the disease and fail to provide adequate information and emotional support [72].
Socioeconomic Parameters
Income inequality and poverty remain major challenges in LA. The correlation between the prevalence of AD symptoms and socioeconomic status should be interpreted with caution since local data from each center may differ substantially from national data. However, to our knowledge, no studies have addressed this issue in LA.
Nutrition
LA is one of the world regions with the most significant disparities in access to a balanced diet, and deficiencies in specific nutrients could contribute to the pathophysiology of the disease [73]. Healthcare providers restricting common foods generates a nutritional burden for the patient and their caregivers. It should be done only in cases where the relationship of a food with the symptoms is proven [74].
Clinical Practice Guidelines
It is difficult to determine if guidelines are regularly followed in patient treatment across LA or what, if any, standards of care are used in the region. No studies were found assessing the real-world application of current Latin American CPGs of AD. In addition, it is hard to determine whether international CPGs are commonly used instead. Application of the European Task Force on Atopic Dermatitis guidelines in a Colombian population with AD improved AD severity and QoL, and only a minority of patients achieved complete control [75].
Most information on AD from LA can be found in research articles and clinical studies by AD experts and researchers. These authors used international diagnostic and classification criteria and standard treatments recommended in local and international CPGs. Nevertheless, the findings are likely biased toward expert care and do not reflect the standard of care (SoC) received by most of the populations affected by AD.
Specifically, in terms of AD treatments, the rapid development and approval of novel therapies, both topical and systemic, leads to rapid obsolescence of multiple CPGs created even a few years earlier and causes difficulties for experts and scientific societies in publishing updated recommendations.
Guaranteed universal treatment access exists in some parts of LA, such as the Explicit Health Guarantees Law in Chile that legally guarantees universal access to diagnosis and treatment for more than 80 high-burden health problems, regardless of insurance. Unfortunately, it does not include AD.
Combating Health Disparities in AD
Few publications reference the disparities in healthcare in patients with AD in the region [62]. The Atopic Dermatitis Quality of Care (ADQoC) initiative [76] aims to develop a global vision for the standards of care for AD, create a repository of best practice interventions and their implementation, sustain collaboration with a group of experts from different countries and regions, and raise the SoC of patients with AD [76]. They surveyed 32 expert AD care centers worldwide, including hospitals in Brazil, Colombia, and Argentina [76].
The ADQoC initiative findings described barriers to achieving adequate care for patients with AD, including misconceptions about the disease, delayed referral and access to AD specialists, poor patient access to AD treatments, and poor adherence to managing the complexity of AD and its comorbidities [76]. These barriers are aggravated in LA by social inequalities and economic deficiencies. Recommendations were derived from this work to improve SoC, education of doctors and patients, access to specialists, and multidisciplinary work for the joint treatment of associated comorbidities [76].
Living Guidelines
Existing guidelines in LA are quite comprehensive, covering diagnosis, classification, outcome measures, comorbidity, and treatments. Notably, some guidelines (e.g., SLAAI) include comments on particular considerations for the region or country, indicating that local Latin American CPGs may be required to address specific epidemiologic, ethnic, and socioeconomic issues pertaining to AD diagnosis and treatments. Several treatment considerations are noteworthy: for example, the lack of coverage by many healthcare systems of moisturizers and emollient creams for AD treatment.
Some of the CPGs in LA were written before dupilumab, and other novel treatments were approved. Optimization of guideline development would allow updating individual recommendations as new evidence is discovered, creating ‘‘living guidelines’’ that can keep up with rapidly evolving treatments for AD.
Patient Education
AD is a complex problem, and its treatment can often challenge patients and HCPs. Major AD treatment guidelines currently recommend education for patients with AD [40, 41]. It is highly recommended that educational strategies be developed for the community, patients, and caregivers [76]. Different models of educational programs exist worldwide, and their structures depend on social and economic conditions. Educational programs for patients with AD can improve adherence, clinical outcomes, and QoL [77, 78]. Nonprofit organizations and medical societies exist in some countries across LA and can provide support and education for HCPs and patients (Table 2).
Therapeutic education, a patient-centered process wherein the healthcare provider includes the patient and caregiver in treatment decision-making, has a proven valuable in chronic diseases in which treatment adherence is usually suboptimal [79]. In chronic diseases such as AD, the percentage of non-adherence to treatment ranges from 30% to 40% [80]. In some cases, this is due to corticophobia or TCS overuse and inadequate information. Therapeutic education is a way to improve adherence, empower patients, and improve QoL, and is recommended with a high level of evidence [79].
For healthcare systems, patient education reduces the demand for centers and services, providing a cost benefit to the healthcare system and decreasing the direct cost of care and the indirect cost to society [76]. Scientific societies also play an integral role in educating the general public, patients, and medical professionals (Table 2).
Leveraging Telemedicine to Advance Patients’ Access to Information and Specialists
The primary reason for the delay in referring patients to specialists is that PCPs do not recognize the condition, and it is challenging to reach experts [76]. Education is the foundation for PCPs, pediatricians, and dermatologists to understand the disease, make an accurate and timely diagnosis, and provide individualized therapy. Sociodemographic and access to information vary widely within LA and even within the same country.
Videoconferencing solutions provide both distant training for physicians and real-time or asynchronous patient access to experts. Telemedicine with videoconferencing is the practice of medicine that uses technology to provide treatment from a distance. The widespread implementation of the strategies suggested in Box 1 would assist in reducing inequities in AD care for patients living in locations where experts are few.
Telementoring, successfully used in Argentina for psoriasis and AD, [81, 82] allows for the remote training of doctors. As an immediate consequence, patients can access specialists in the best available clinics without needing to travel to specialized centers. This system allows the treating physician to receive feedback while training in their local area. A mobile application developed in Argentina creates a space where patients can record symptoms, build peer-to-peer networks, schedule appointments, and communicate with their HCPs.
Socioeconomic Impact on Treatment of AD
Access to treatment is very uneven between regions, the different LA countries, and private and public healthcare systems. The development of local living CPGs [30], patient education programs that inform and empower patients, and public policies to improve the distribution of health resources are strategies that can help increase coverage of treatments for AD.
Managing Comorbidities
AD has multiple comorbidities. Multidisciplinary work is essential to carry out a holistic treatment approach: dermatologists, allergists, pediatricians, PCPs, pulmonologists, dieticians, and psychologists, among others, must work together to achieve a comprehensive care approach.
Implementing atopic and multidisciplinary clinics creates spaces that allow for the joint discussion of therapeutic alternatives, saving time for the patient and costs for the healthcare system. We must not neglect mental health since both systemic inflammation and disease burden may cause depression and ADHD.
This paper is a narrative review and thus does not include all available data, although we made every effort to find published articles on this topic. We also recognize that LA is a diverse region with varying needs of different countries and even varying needs within each country. Our panel consisted of pediatric allergists and dermatologists from six of the countries in the region, so this paper cannot address specifics to every country.
Conclusions
LA is a group of heterogeneous countries with various geographical, economical, and cultural conditions. Additionally, the organization of the healthcare system is diverse. The disparity in the access to diagnosis and treatment of AD among Latin American countries is due to factors derived from these differences. In the same country, there may be inequality between the population with higher or lower income, ethnic ancestry, or their place of residence (rural or urban area). Some of these factors can be corrected, and we propose different measures to reduce healthcare disparities in managing AD and thus achieve better disease control with a positive impact on patients and communities in LA. The accessibility to new and expensive therapies for AD, and their influence on the healthcare systems in LA, must be addressed (Fig. 1).
References
Saunes M, Øien T, Storrø O, Johnsen R. Family eczema-history in 2-year-olds with eczema; a prospective, population-based study. The PACT-study, Norway. BMC Dermatol. 2011;11:11.
Werfel T, Allam JP, Biedermann T, Eyerich K, Gilles S, Guttman-Yassky E, et al. Cellular and molecular immunologic mechanisms in patients with atopic dermatitis. J Allergy Clin Immunol. 2016;138(2):336–49.
Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109–22.
González-Mendoza T, Bedolla-Barajas M, Bedolla-Pulido TR, Morales-Romero J, Pulido-Guillén NA, Lerma-Partida S, et al. The prevalence of allergic rhinitis and atopic dermatitis in late adolescents differs according to their gender. Rev Alerg Mex. 2019;66(2):147–53.
Wu LC, Hwang CY, Chung PI, Hua TC, Chen YD, Chu SY, et al. Autoimmune disease comorbidities in patients with atopic dermatitis: a nationwide case-control study in Taiwan. Pediatr Allergy Immunol. 2014;25(6):586–92.
Sánchez J, Sánchez A, Cardona R. Particular characteristics of atopic eczema in tropical environments. The Tropical Environment Control for Chronic Eczema and Molecular Assessment (TECCEMA) cohort study. An Bras Dermatol. 2017;92(2):177–83.
Solé D, Mallol J, Wandalsen GF, Aguirre V. Prevalence of symptoms of eczema in Latin America: results of the international study of asthma and allergies in childhood (ISAAC) Phase 3. J Investig Allergol Clin Immunol. 2010;20(4):311–23.
Silverberg JI, Barbarot S, Gadkari A, Simpson EL, Weidinger S, Mina-Osorio P, et al. Atopic dermatitis in the pediatric population: a cross-sectional, international epidemiologic study. Ann Allergy Asthma Immunol. 2021;126(4):417-28.e2.
Garmhausen D, Hagemann T, Bieber T, Dimitriou I, Fimmers R, Diepgen T, et al. Characterization of different courses of atopic dermatitis in adolescent and adult patients. Allergy. 2013;68(4):498–506.
Sánchez J, Sánchez A, Cardona R. Critical review of ISAAC results for atopic dermatitis in tropical cities. Rev Alerg Mex. 2018;65(4):389–99.
Carrascosa JM. Mexican consensus on the diagnosis and treatment of atopic dermatitis in adolescents and adults. Rev Alerg Mex. 2018;65(Suppl 2):s7–8.
Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014;129 Suppl 2(Suppl 2):5–8.
Agency for Healthcare Research and Quality [Available from: https://www.ahrq.gov/topics/disparities.html.
Cuervo MM, Sanclemente G, Barrera LM. Clinical and sociodemographic features and quality of life in patients with atopic dermatitis who attended dermatology teaching clinics in Medellín. Antioquia Metropolitan Area Biomedica. 2021;41(4):676–91.
Annett RD, Bender BG, Lapidus J, Duhamel TR, Lincoln A. Predicting children’s quality of life in an asthma clinical trial: what do children’s reports tell us? J Pediatr. 2001;139(6):854–61.
Ruano AL, Rodríguez D, Rossi PG, Maceira D. Understanding inequities in health and health systems in Latin America and the Caribbean: a thematic series. Int J Equity Health. 2021;20(1):94.
Borzutzky A, Larco JI, Luna PC, McElwee E, Pires MC, Rico Restrepo M, et al. Atopic dermatitis in Latin America: a roadmap to address data collection, knowledge gaps, and challenges. Dermatitis. 2022.
Trikamjee T, Basera W, Botha M, Facey-Thomas HE, Gaunt B, Genuneit J, et al. Associations between environmental dust composition and atopic dermatitis in urban and rural settings. Pediatr Allergy Immunol. 2021;32(5):1013–21.
Urrutia-Pereira M, Guidos-Fogelbach G, Solé D. Climate changes, air pollution and allergic diseases in childhood and adolescence. J Pediatr (Rio J). 2022;98(Suppl 1):S47-s54.
Solis-Soto MT, Patiño A, Nowak D, Radon K. Association between environmental factors and current asthma, rhinoconjunctivitis and eczema symptoms in school-aged children from Oropeza Province–Bolivia: a cross-sectional study. Environ Health. 2013;12:95.
Dei-Cas I, Dei-Cas P, Acuña K. Atopic dermatitis and risk factors in poor children from Great Buenos Aires. Argentina Clin Exp Dermatol. 2009;34(3):299–303.
Danby SG, Brown K, Wigley AM, Chittock J, Pyae PK, Flohr C, et al. The effect of water hardness on surfactant deposition after washing and subsequent skin irritation in atopic dermatitis patients and healthy control subjects. J Invest Dermatol. 2018;138(1):68–77.
Brenninkmeijer EE, Schram ME, Leeflang MM, Bos JD, Spuls PI. Diagnostic criteria for atopic dermatitis: a systematic review. Br J Dermatol. 2008;158(4):754–65.
Silverberg JI, Thyssen JP, Paller AS, Drucker AM, Wollenberg A, Lee KH, et al. What’s in a name? Atopic dermatitis or atopic eczema, but not eczema alone. Allergy. 2017;72(12):2026–30.
Mohan GC, Lio PA. Comparison of dermatology and allergy guidelines for atopic dermatitis management. JAMA Dermatol. 2015;151(9):1009–13.
Arents BWM, van Zuuren EJ, Vermeulen S, Schoones JW, Fedorowicz Z. Global Guidelines in Dermatology Mapping Project (GUIDEMAP), a systematic review of atopic dermatitis clinical practice guidelines: are they clear, unbiased, trustworthy and evidence based (CUTE)? Br J Dermatol. 2022;186(5):792–802.
Schmitt J, Spuls PI, Thomas KS, Simpson E, Furue M, Deckert S, et al. The harmonising outcome measures for eczema (HOME) statement to assess clinical signs of atopic eczema in trials. J Allergy Clin Immunol. 2014;134(4):800–7.
Sánchez J, Páez B, Macías A, Olmos C, de Falco A. Atopic dermatitis guideline. Position paper from the Latin American Society of Allergy, Asthma and Immunology. Rev Alerg Mex. 2014;61(3):178–211.
(AsoColDerma) ACdDyCD. Guía de práctica clínica (GPC) para el diagnóstico y tratamiento de la dermatitis atópica en Colombia [Clinical practice guidelines (CPG) for the diagnosis and treatment of atopic dermatitis in Colombia]. Rev Asoc Colomb Dermatol Cir Dermatol 2020.
Máspero JC, Hugo, editor. Guías para el Diagnóstico y Tratamiento de la Dermatitis Atópica [Guidelines for the Diagnosis and Treatment of Atopic Dermatitis]: Asociación Argentina de Alergia e Inmunología Clínica; 2019.
Rosário N. Updated practical guide on atopic dermatitis - Part I: etiopathogenesis, clinical features, and diagnosis. Joint position paper of the Brazilian Association of Allergy and Immunology and the Brazilian Society of Pediatrics. Arquivos e asma alergia e imunologia. 2017;1:131.
Carvalho VO, Solé D, Antunes AA, Bau AEK, Kuschnir FC, Mallozi MC, et al., editors. Guia prático de atualização em dermatite atópica - Parte II: abordagem terapêutica. Posicionamento conjunto da Associação Brasileira de Alergia e Imunologia e da Sociedade Brasileira de Pediatria2017.
Rincón-Pérez C, Larenas-Linnemann D, Figueroa-Morales M, Luna-Pech J, García-Hidalgo L, Weinmann A, et al. Mexican consensus on the diagnosis and treatment of atopic dermatitis in adolescents and adults. Revista alergia Mexico (Tecamachalco, Puebla, Mexico : 1993). 2018;65 Suppl 2:s8-s88.
Bos B, Antonescu I, Osinga H, Veenje S, de Jong K, de Vries TW. Corticosteroid phobia (corticophobia) in parents of young children with atopic dermatitis and their health care providers. Pediatr Dermatol. 2019;36(1):100–4.
Yrjänä JMS, Bloigu R, Kulmala P. Parental confusion may result when primary health care professionals show heterogeneity in their knowledge, attitudes, and perceptions regarding infant nutrition, food allergy, and atopic dermatitis. Allergol Immunopathol (Madr). 2018;46(4):326–33.
Perry TT, Patel MR, Li JT. Elevating health disparities education among trainees and physicians. J Allergy Clin Immunol Pract. 2022;10(4):918–22.
Tackett KJ, Jenkins F, Morrell DS, McShane DB, Burkhart CN. Structural racism and its influence on the severity of atopic dermatitis in African American children. Pediatr Dermatol. 2020;37(1):142–6.
Silverberg JI. Racial and ethnic disparities in atopic dermatitis. Current Dermatology Reports. 2015;4(1):44–8.
Eichenfield LF, Tom WL, Berger TG, Krol A, Paller AS, Schwarzenberger K, et al. Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol. 2014;71(1):116–32.
Wollenberg A, Barbarot S, Bieber T, Christen-Zaech S, Deleuran M, Fink-Wagner A, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol. 2018;32(5):657–82.
Aoki V, Lorenzini D, Orfali RL, Zaniboni MC, Oliveira ZNP, Rivitti-Machado MC, et al. Consensus on the therapeutic management of atopic dermatitis—Brazilian Society of Dermatology. An Bras Dermatol. 2019;94(2 Suppl 1):67–75.
Antunes AA, Solé D, Carvalho VO, Bau AEK, Kuschnir FC, Mallozi MC, et al. Guia prático de atualização em dermatite atópica - Parte I: etiopatogenia, clínica e diagnóstico. Posicionamento conjunto da Associação Brasileira de Alergia e Imunologia e da Sociedade Brasileira de Pediatria. BJAI. 2017;1(2):131–56.
Wollenberg A, Kinberger M, Arents B, Aszodi N, Avila Valle G, Barbarot S, et al. European guideline (EuroGuiDerm) on atopic eczema: part I—systemic therapy. J Eur Acad Dermatol Venereol. 2022;36(9):1409–31.
Breternitz M, Kowatzki D, Langenauer M, Elsner P, Fluhr JW. Placebo-controlled, double-blind, randomized, prospective study of a glycerol-based emollient on eczematous skin in atopic dermatitis: biophysical and clinical evaluation. Skin Pharmacol Physiol. 2008;21(1):39–45.
Peris K, Valeri P, Altobelli E, Fargnoli MC, Carrozzo AM, Chimenti S. Efficacy evaluation of an oil-in-water emulsion (Dermoflan) in atopic dermatitis. Acta Derm Venereol. 2002;82(6):465–6.
Grimalt R, Mengeaud V, Cambazard F. The steroid-sparing effect of an emollient therapy in infants with atopic dermatitis: a randomized controlled study. Dermatology. 2007;214(1):61–7.
Msika P, De Belilovsky C, Piccardi N, Chebassier N, Baudouin C, Chadoutaud B. New emollient with topical corticosteroid-sparing effect in treatment of childhood atopic dermatitis: SCORAD and quality of life improvement. Pediatr Dermatol. 2008;25(6):606–12.
Mirali S, Fleming P, Lynde CW. Moisturizers and cleansers in the management of skin conditions caused by personal protective equipment and frequent handwashing. Skin Therapy Lett. 2021;26(4):9–13.
Diluvio L, Dattola A, Cannizzaro MV, Franceschini C, Bianchi L. Clinical and confocal evaluation of avenanthramides-based daily cleansing and emollient cream in pediatric population affected by atopic dermatitis and xerosis. G Ital Dermatol Venereol. 2019;154(1):32–6.
Wollenberg A, Reitamo S, Atzori F, Lahfa M, Ruzicka T, Healy E, et al. Proactive treatment of atopic dermatitis in adults with 0.1% tacrolimus ointment. Allergy. 2008;63(6):742–50.
Ruzicka T, Bieber T, Schöpf E, Rubins A, Dobozy A, Bos JD, et al. A short-term trial of tacrolimus ointment for atopic dermatitis. European Tacrolimus Multicenter Atopic Dermatitis Study Group. N Engl J Med. 1997;337(12):816–21.
Reitamo S, Wollenberg A, Schöpf E, Perrot JL, Marks R, Ruzicka T, et al. Safety and efficacy of 1 year of tacrolimus ointment monotherapy in adults with atopic dermatitis. The European Tacrolimus Ointment Study Group. Arch Dermatol. 2000;136(8):999–1006.
Sidbury R, Davis DM, Cohen DE, Cordoro KM, Berger TG, Bergman JN, et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71(2):327–49.
Tintle S, Shemer A, Suárez-Fariñas M, Fujita H, Gilleaudeau P, Sullivan-Whalen M, et al. Reversal of atopic dermatitis with narrow-band UVB phototherapy and biomarkers for therapeutic response. J Allergy Clin Immunol. 2011;128(3):583–93.e1–4.
Garritsen FM, Brouwer MW, Limpens J, Spuls PI. Photo(chemo)therapy in the management of atopic dermatitis: an updated systematic review with implications for practice and research. Br J Dermatol. 2014;170(3):501–13.
Meduri NB, Vandergriff T, Rasmussen H, Jacobe H. Phototherapy in the management of atopic dermatitis: a systematic review. Photodermatol Photoimmunol Photomed. 2007;23(4):106–12.
Drucker AM, Ellis AG, Bohdanowicz M, Mashayekhi S, Yiu ZZN, Rochwerg B, et al. Systemic immunomodulatory treatments for patients with atopic dermatitis: a systematic review and network meta-analysis. JAMA Dermatol. 2020;156(6):659–67.
Simpson EL, Gadkari A, Worm M, Soong W, Blauvelt A, Eckert L, et al. Dupilumab therapy provides clinically meaningful improvement in patient-reported outcomes (PROs): a phase IIb, randomized, placebo-controlled, clinical trial in adult patients with moderate to severe atopic dermatitis (AD). J Am Acad Dermatol. 2016;75(3):506–15.
He H, Guttman-Yassky E. JAK inhibitors for atopic dermatitis: an update. Am J Clin Dermatol. 2019;20(2):181–92.
Abramo L, Cecchini S, Ullmann H. Addressing health inequalities in Latin America: the role of social protection. Cien Saude Colet. 2020;25(5):1587–98.
Silva-Peñaherrera M, Lopez-Ruiz M, Merino-Salazar P, Gómez-García AR, Benavides FG. Health inequity in workers of Latin America and the Caribbean. Int J Equity Health. 2020;19(1):109.
Sanchez J, Cherrez-Ojeda I, Galvan C, Garcia E, Hernández-Mantilla N, Londoño Garcia A, et al. The unmet needs in atopic dermatitis control in Latin America: a multidisciplinary expert perspective. Dermatol Ther (Heidelb). 2021;11(5):1521–40.
Machado C, Dias de Lima L. Políticas e sistemas de saúde na América Latina: identidade regional e singularidades nacionais. Cadernos de Saúde Pública. 2017;33.
Ferre JC. Economic inequalities in Latin America at the base of adverse health indicators. Int J Health Serv. 2016;46(3):501–22.
Vincens N, Emmelin M, Stafström M. Social capital, income inequality and the social gradient in self-rated health in Latin America: a fixed effects analysis. Soc Sci Med. 2018;196:115–22.
Garnelo L, Parente RCP, Puchiarelli MLR, Correia PC, Torres MV, Herkrath FJ. Barriers to access and organization of primary health care services for rural riverside populations in the Amazon. Int J Equity Health. 2020;19(1):54.
Ferrari G, Guzmán-Habinger J, Chávez JL, Werneck AO, Silva DR, Kovalskys I, et al. Sociodemographic inequities and active transportation in adults from Latin America: an eight-country observational study. Int J Equity Health. 2021;20(1):190.
Ferdinand A, Lambert M, Trad L, Pedrana L, Paradies Y, Kelaher M. Indigenous engagement in health: lessons from Brazil, Chile, Australia and New Zealand. Int J Equity Health. 2020;19(1):47.
Viáfara-López CA, Palacios-Quejada G, Banguera-Obregón A. Ethnic-racial inequity in health insurance in Colombia: a cross-sectional study. Rev Panam Salud Publica. 2021;45: e77.
Mena-Meléndez L. Ethnoracial child health inequalities in Latin America: multilevel evidence from Bolivia, Colombia, Guatemala, and Peru. SSM Popul Health. 2020;12: 100673.
Ogbogu PU, Noroski LM, Arcoleo K, Reese BD Jr, Apter AJ. Methods for cross-cultural communication in clinic encounters. J Allergy Clin Immunol Pract. 2022;10(4):893–900.
Takaoka R, Cicchini T, Aoki V. Creating new solutions for the patient with atopic dermatitis 2014. E41-E p.
Yu Y, Dunaway S, Champer J, Kim J, Alikhan A. Changing our microbiome: probiotics in dermatology. Br J Dermatol. 2020;182(1):39–46.
Sánchez J, Sánchez MR, Macías-Weinmann A, Barreto B, Ensina LF, Uriarte-Obando SA, et al. Systematic review about 10 interventions in dermatitis. A document from the Latin American Society of Allergy, Asthma, and Immunology. Rev Alerg Mex. 2019;66(4):426–55.
Sánchez J, Toro Y, Cardona R. Clinical impact in the real life of guidelines recommendations for atopic dermatitis in a tropical population (TECCEMA cohort). Rev Alerg Mex. 2017;64(3):260–9.
Guttman-Yassky E, Nosbaum A, Simpson E, Weidinger S. Pioneering global best practices in atopic dermatitis: results from the atopic dermatitis quality of care initiative. Clin Exp Dermatol. 2022;47(2):303–11.
Takaoka R, Coelho E. Patient education in atopic dermatitis: why it is needed and how to improve it. Curr Dermatol Rep. 2018;7(4):221–6.
Stalder JF, Bernier C, Ball A, De Raeve L, Gieler U, Deleuran M, et al. Therapeutic patient education in atopic dermatitis: worldwide experiences. Pediatr Dermatol. 2013;30(3):329–34.
Eichenfield LF, Kusari A, Han AM, Barbarot S, Deleuran M, Lio P, et al. Therapeutic education in atopic dermatitis: a position paper from the International Eczema Council. JAAD Int. 2021;3:8–13.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
Mazzuoccolo L, Esposito M, Luna P, Seiref S, Dominguez M, Echeverría C. WhatsApp: a real-time tool to reduce the knowledge gap and share the best clinical practices in psoriasis. Telemedicine and e-Health. 2018;25.
Luna PC, Debernardi ME, Echeverría CM, Angles MV, Mazzuoccolo LD. ECHO project in atopic dermatitis in Argentina: an innovative strategy to reach underserved areas with up to date knowledge, first year of experience. An Bras Dermatol. 2022;97(4):443–7.
Acknowledgements
Funding
Funding for this narrative review was provided by Americas Health Foundation through an unrestricted grant from the Pfizer foundation. The Rapid Service Fee was funded by the unrestricted grant.
Editorial Assistance
We would like to thank Dawn M. Bielawski for editing assistance.
Authorship
All authors contributed to the manuscript draft and reviewed the final paper.
Author contributions
Jorge Sánchez: Wrote original draft, performed formal analysis, reviewed and edited manuscript. Iris-Selva Ale: Wrote original draft, performed formal analysis, reviewed and edited manuscript. Maria Valeria Angles: Wrote original draft, performed formal analysis, reviewed and edited manuscript. Guillermo Guidos Fogelbach: Wrote original draft, performed formal analysis, reviewed and edited manuscript. Angela Marie Jansen: Conceptualized the project, performed formal analysis, reviewed and edited manuscript, performed project administration. Roberto Takaoka: Wrote original draft, performed formal analysis, reviewed and edited manuscript. Arturo Borzutzky: Wrote original draft, performed formal analysis, reviewed and edited manuscript. All authors read and approved the final manuscript.
Disclosures
The co-authors declare no conflicts of interest.
Compliance with Ethics Guidelines
This is a narrative review with no patient information. JS provided unpublished observations from an anonymous survey that was exempt from institutional review board review in the country where it was conducted. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data availability
The only datasets generated during the current study was the informal poll taken by the lead author; these data are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sánchez, J., Ale, IS., Angles, M.V. et al. Healthcare Disparities in Atopic Dermatitis in Latin America: A Narrative Review. Dermatol Ther (Heidelb) 13, 399–416 (2023). https://doi.org/10.1007/s13555-022-00875-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00875-y