Abstract
Introduction
Despite advances in treatment options and the management of patients with psoriasis, considerable unmet needs remain. Our objective was to identify ways to elevate the standard of care for patients with psoriasis by combining the perspectives of three important stakeholders: patients, clinicians and payors, and define ‘Calls to Action’ designed to achieve the identified changes.
Methods
Eight themes relevant to elevating the standard of care were identified from an insights-gathering questionnaire completed by all three stakeholder groups. A modified Delphi exercise gained consensus on statements informed by the insights. Statements were then used to inspire ‘Calls to Action’ – practical steps that could be taken to realise the desired changes and elevate the standard of care.
Results
In total, 18 European experts (10 dermatologists, 3 payors and 5 patient representatives) took part in the Delphi process. Consensus was reached on statements relating to all eight themes: improve healthcare systems to better support multidisciplinary team working and digital services, real-world data generation and optimal use, improve patient access, elevate quality-of-life measures as the most important outcomes, involve patients in patient-centred and personalised approaches to care, improve the relevance and reach of guidelines, education, and multistakeholder engagement. ‘Calls to Action’ common to all three stakeholder groups recognised the need to capitalise on the shift to digital healthcare, the need for consistent input into registries to generate real-world evidence to support guideline development, and the necessity of educating patients on the benefits of reporting outcomes to generate real-world data. The enormous quality-of-life burden and psychological impact of psoriasis, as well as the clinical needs of patients must be better understood, including by healthcare commissioners, so that funding priorities are assessed appropriately.
Conclusion
This unique initiative identified a practical ‘Call-to-Action Framework’ which, if implemented, could help improve the standard of care for patients with psoriasis.
Video Abstract (MP4 44777 KB)
Plain Language Summary
Despite improvements in the management of psoriasis, there is room for the standard of care for patients to be improved further. The aim of the ‘Epicensus’ programme is to help realise improvements by bringing together three important stakeholder groups involved in the care of patients with psoriasis: dermatologists, payors and patient representatives. First, unmet needs were explored with these stakeholders and eight themes for change were identified: 1) improve healthcare systems to better support multidisciplinary team working and digital services; 2) optimise real-world data generation and use; 3) improve patient access; 4) elevate quality-of-life measures as the most important outcomes; 5) involve patients in people-centred and personalised approaches to care; 6) improve the relevance and reach of guidelines; 7) education; 8) multistakeholder engagement. Next, a panel of experts representing the three stakeholder groups took part in a consensus process (Delphi) to reach agreement on statements relating to each of the eight themes. The statements describe current problems and what needs to be changed to raise the standard of care for patients with psoriasis. Some of the problems identified are similar to those that existed a decade ago, showing that simply recognising what needs to change is not enough to bring about improvements: action must be taken. Therefore, the Epicensus participants met to produce specific ‘Calls to Action’– practical steps described in this publication that, if put into practice, should contribute to an improvement in the standard of care for patients with psoriasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The treatment, care and management of patients with psoriasis remains suboptimal. |
The Epicensus programme was designed to establish the current state of care from a uniquely multistakeholder perspective (dermatologists, payors and patient representatives). |
A consensus exercise identified areas and aspects of care that need improving. |
The results revealed that despite advances in treatment options and the management of patients with psoriasis, some unmet needs and barriers to improvements in the standard of care identified a decade ago still exist. |
The aim of Epicensus is to effect positive change, and here we report ‘Calls to Action’ based on the consensus statements that, if implemented, should elevate the standard of care and therefore make progress towards optimal management of patients with psoriasis. |
Digital Features
This article is published with digital features, including a video abstract, infographic and plain language summary, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.23599077.
Introduction
Psoriasis, an immune-mediated, chronic inflammatory disease primarily affecting the skin and causing scaling, pain, itching and burning, is now widely accepted to be systemic in nature with manifestations beyond the skin [1, 2]. Patients with psoriasis can experience serious comorbidities including psoriatic arthritis (PsA), cardiometabolic syndrome, inflammatory bowel disease and psychological disorders [1,2,3,4,5].
Psoriasis is complex, requiring multidisciplinary, personalised care [4, 6,7,8]. Combined dermatology and rheumatology clinics can successfully improve the diagnosis and management of challenging cases and enable early detection and treatment of PsA [9]; however, this remains a significant practice gap [10, 11]. It has been suggested that the multidisciplinary team (MDT) approach should be the norm rather than the exception, potentially expanding beyond dermatology, rheumatology and gastroenterology [4]. Indeed, a study is currently recruiting to explore whether an interdisciplinary combined clinic (including nurses and psychologists) is more effective than usual siloed care [12, 13]. Furthermore, the coronavirus disease 2019 (COVID-19) pandemic has highlighted inadequacies in infrastructure and inequities in healthcare access [14]. Clinical pathways have had to adapt to continue to provide care for patients [15].
Despite advances in treatment options [16] and management [17], substantial unmet needs remain [6, 18, 19]. The physical and psychological multi-morbidities continue to exert far-reaching, negative consequences on patients and society including stigmatisation, work absenteeism, relationship difficulties and increasing out-of-pocket healthcare costs [2, 20,21,22]. Patients with psoriasis and physical or psychological comorbidities experience an increased clinical burden, worse quality of life (QoL) and greater economic burden than those without comorbidities [2]. Healthcare costs associated with psoriasis increase over time as the disease progresses [23], and compared with matched controls, patients with psoriasis experience higher healthcare costs and a greater negative impact on income and employment [24]. Disease burden is also affected by plaque location. Visible plaques and plaques in sexually-sensitive areas [2, 25] and plaques on the hands, feet or genitalia increase work absenteeism [21]. Low patient–physician concordance regarding satisfaction with psoriasis management often occurs [26] and is associated with increased disease symptoms and severity and reductions in QoL and work productivity [27].
Barriers to optimal care include the discrepancies between the heterogeneous patient population encountered in clinical practice and the uniform population enrolled in clinical trials [28, 29], and healthcare system differences including waiting times and variation in the availability of and access to advanced therapies including biologics and small molecules.
To alleviate the sustained burden, an elevation in the standard of care (SoC) is warranted but the range of unmet needs suggests that changes to achieve this would be multifaceted. A study by the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) and KPMG identified and explored areas in which care for patients with PsA could be improved and improvement indicators were defined [30]. Similarly, the aim of the Epicensus programme was to identify ways in which the SoC could be elevated from the perspective of three important stakeholders: patients, clinicians and payors. Here, we report a Delphi exercise performed to gain an up-to-date consensus on key themes related to elevating the SoC for patients with psoriasis from a unique, multistakeholder perspective. Having identified these areas, we also report ‘Calls to Action’ inspired by the consensus statements, which are designed to bring about the identified changes.
Methods
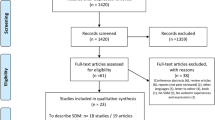
The Epicensus programme is a pan-European, multistakeholder initiative aimed at elevating the SoC for patients with psoriasis. By bringing together clinicians (dermatologists), payors and patient representatives, a broad picture of the current state of care was generated to inform how this could be elevated from the different stakeholder perspectives. The participating stakeholders are shown in the supplementary material. The goal was to generate ‘Calls to Action’ that, if implemented, could improve the overall SoC. The first phase of the programme was a questionnaire (see the electronic supplementary material) designed to gather insights around psoriasis care and changes needed to improve it, which was completed by all stakeholder groups. Responses were collated, analysed qualitatively and eight key themes relevant to elevating the SoC were identified (Table 1). This informed the second phase: a Delphi exercise to achieve consensus agreement on statements arising from the insights. Consensus was defined as ≥ 75% selecting ‘agree’ or ‘strongly agree’. Since the objective was to gain multistakeholder consensus, but the stakeholders were not equal in number, individual votes were weighted so that each stakeholder group had an equal impact on the overall percentage calculated. To progress towards an elevation in the standard of care, the third phase was a multistakeholder meeting in which ‘Calls to Action’, inspired by the consensus statements, were developed to achieve the improvements (Fig. 1). The electronic supplementary material contains further detailed information on the programme including the participants’ backgrounds (Table S1) and the Delphi voting.
A flow chart to show the phases of the Epicensus programme. A large pool of stakeholders completed the questionnaire to gain as broad a perspective as possible. The number of stakeholders who completed the Delphi exercise was smaller but included some individuals new to the programme to test agreement with the statements with additional participants. SoC standard of care
Results
Respondents
One of the three payors only took part in the third Delphi e-survey while one clinician was unable to take part in the third Delphi e-survey. Therefore, 17 stakeholders answered each question except where an answer was omitted by one stakeholder and the percentage agreement was calculated out of 16 responses. The weighting used to calculate the consensus agreement was adjusted accordingly.
Consensus Statements and ‘Calls to Action’
Statements, percentage consensus agreement, and ‘Calls to Action’ common to all stakeholder groups are presented in the Tables. Statements used to inspire ‘Calls to Action’ are highlighted alongside the corresponding ‘Calls to Action’. These tables are complemented by and should be read in conjunction with the further information and responses to open-ended questions included in the ‘discussion points’ below for each theme. ‘Calls to Action’ that were common to only two groups are presented in the electronic supplementary material (Table S2). This manuscript is formed of the opinions of the authors themselves. There was no need to collect any type of patient data. Hence, the approval of an Ethics Committee was not required. Consent was obtained from all participants as they were contracted by UCB Pharma to take part in this programme.
Discussion Points
Improve Healthcare Systems to Better Support MDT Working and Digital Services (Table 2)
Consensus Statements and Open-Ended Questions
Consensus was achieved on all statements except one. Initial disagreement around the focus on mental health was resolved by modifying the statement to clarify that it should be one of the aims of an MDT approach. The composition of the MDT is discussed below (see ‘Improve the relevance and reach of guidelines’).
Open-ended questions on the topic of ‘digital healthcare’ revealed different interpretations of the term. It encompasses a broad range of activities as indicated by the penultimate consensus statement in Table 2. Stakeholders felt that teleconsultations and virtual consultations cannot fully replace face-to-face appointments; they must complement each other. While telephone consultations can be convenient, frequently constituting perfectly adequate follow up, virtual ‘Facetime’-style appointments are not always an improvement, proving awkward for physicians and patients alike if more intimate areas are involved. Appropriate patients for digital healthcare were identified as those comfortable with the technology (‘tech-savvy’), whose disease status is appropriate (e.g. stable) as well as those for whom travel is difficult (e.g. living in rural areas). Less suitable patients are usually older, unfamiliar with the technology or with disabilities or conditions (e.g. dementia) that prevent them from using digital media, as well as newly diagnosed patients or those with unstable disease. However, it was felt that these patients are in the minority and that sometimes it is stakeholders, not patients, who fail to embrace the digital shift.
‘Calls to Action’
Stakeholders agreed that supporting adoption of digital care will involve education, training, collaboration, and support among healthcare professionals (HCPs), payors and patients, not only in how to use the technology, but also to understand the benefits it provides to enhance engagement and support an elevation in the SoC.
Real-World Data (RWD) Generation and Optimal Use (Table 3)
Consensus Statements and Open-Ended Questions
Stakeholders suggested that patients cared most about the effectiveness and sustained efficacy of treatments and QoL followed by the safety and tolerability of treatments and having clear skin. RWD was seen as critical in filling gaps in knowledge left by strict clinical trial inclusion criteria, resulting in a paucity of data in special populations (e.g. elderly, children, pregnant/breast-feeding women, those with cancer or other comorbid diseases).
‘Calls to Action’
Stakeholders advocated the development of national registries. Incentivising clinicians to report RWD consistently or making contribution mandatory, looking for opportunities to engage pharmacists in RWD generation activities, highlighting the importance of real-world evidence (RWE) to all stakeholders and educating patients on the value of RWE so that they proactively provide information were discussed. The need to capture a standard/minimal set of outcomes including patient-reported outcomes (PROs) was noted.
Improve Patient Access (Table 4)
Consensus Statements and Open-Ended Questions
Some stakeholders repeated their view that psychological support does not need to be mandatory; however, it should be available if needed. The right number of experienced staff, MDTs, good levels of funding and reimbursement, flexible prescribing, access to all/innovative medicines and involving patients in decisions were all identified as features of healthcare systems that offer equitable patient access.
‘Calls to Action’
Rapid access to well-informed, equitable care would be supported by ensuring that health-service commissioners better understand the clinical needs of patients with psoriasis, so they reassess funding priorities. Generating evidence of the value of biologics and biosimilars including their cost-effectiveness, especially in the long-term and when adopted early, was considered key to achieving this.
Elevate Quality-of-Life Measures as the Most Important Outcomes (Table 5)
Consensus Statements and Open-Ended Questions
Consensus was reached that QoL measures should be elevated as the most important outcomes and that validated measures and tools to assess QoL exist and should be used consistently. Stakeholders identified the three most valuable measures as the Dermatology Life Quality Index followed by the Psoriasis Disability Index and the Psoriasis Index of QoL from a list of 11 suggestions with the option to add others. While most stakeholders (n = 14/17; 82.4%) agreed that the existing tools effectively and specifically capture all relevant aspects of QoL, a few dermatologists noted that existing tools (except the Patient Benefit Index (PBI)) fail to consider the patient perspective or psychological impact or that the visibility of lesions is not adequately or specifically assessed. While stakeholders acknowledged that the concept of Cumulative Life Course Impairment (CLCI) has potential clinical value, an actual measure to capture it is needed.
‘Calls to Action’
Stakeholders remain motivated to improve upon existing QoL tools possibly by incorporating them into a new, universal tool. Identifying and prioritising the most important existing tools, including those that are most relevant to payors, and agreeing on a consistent method of collecting high-quality data are crucial to address the burden psoriasis places on QoL and elevate the SoC.
Involve Patients in Patient-Centred and Personalised Approaches to Care (Table 6)
Consensus Statements and Open-Ended Questions
All statements relating to patient-centricity achieved 100% consensus, highlighting how critical patient-centricity and patient voice are. However, stakeholders noted that patients must be free to choose if they wish to participate in shared decision-making and their decision respected.
‘Calls to Action’
Stakeholders agreed that patients are uniquely placed to provide valuable information beyond that of their own disease and treatment progress. Their knowledge and experience of healthcare systems could provide information which may be utilised to help elevate the SoC. Establishing standard ways to capture their views is needed.
Improve the Relevance and Reach of Guidelines (Table 7)
Consensus Statements and Open-Ended Questions
Consensus was reached that dermatologists and rheumatologists should share the management of patients with psoriasis depending on disease manifestations. Essential MDT members needed to develop multidisciplinary guidance to support an MDT approach were identified as rheumatologists and dermatologists followed by psychologists, general practitioners, gastroenterologists and cardiologists. Some suggested that additional specialists were unnecessary, while others felt diabetologists/endocrinologists, obstetricians and gynaecologists would provide further valuable input to support guidance and thus improve the relevance and utility of guidelines. Barriers to implementing guidelines were identified as the organisation of the healthcare system (e.g. lack of MDT pathways), complexity of guidelines, the speed with which they are updated in a rapidly changing field and regional differences. Overall, 71% of stakeholders believed that changes at the healthcare system level should be prioritised to realise the most rapid elevation(s) in the SoC, while 29% would prioritise changes at the physician level.
‘Calls to Action’
To improve the relevance and reach of guidelines, a harmonised approach to their development is needed, encompassing all aspects of the disease (psychological, comorbidities etc.) and all patient subgroups (e.g. elderly) while incorporating the patient perspective and experiences and with regular reviews and updates to include clinical and health economic RWD (especially patient-relevant data).
Education (Table 8)
Consensus Statements and Open-Ended Questions
The importance of education was highlighted by 100% consensus for all statements. Suggested education topics are summarised in Table 9.
‘Calls to Action’
The ‘Calls to Action’ reflect the consensus that all stakeholders would benefit from more education and indicate a preference for multistakeholder training and educational initiatives.
Multistakeholder Engagement (Table 10)
Consensus Statements and Open-Ended Questions
Current lack of patient involvement in many industry activities was confirmed. Stakeholders felt industry could best support patient involvement through funding in various forms (unrestricted grants, independent research, reimbursing patients’ time/expertise, sponsoring patient meetings to disseminate research findings, podcasts, publications, symposia for patients as well as training/education). Other suggestions included industry supporting registries and educating patients on the need to report data, supporting patients to help payors understand patient needs, promoting participation of patient research partners (patients who actively participate in research teams alongside and on an equal basis with professional researchers) in activities of groups such as GRAPPA and becoming involved in clinical trial design. However, this should complement but never replace industry support of physicians themselves.
‘Calls to Action’
Patients should be involved at all stages from (research and development) R&D to RWD and RWE generation, so that their knowledge, experience and perspectives can be harnessed to add value. Critical to the success of patient involvement is ensuring that outcomes and data are communicated back to patients appropriately within the local regulatory framework. This will enhance patient engagement and education, desirable factors in narrowing the gap between patients and industry.
Discussion
The ultimate aim of the pan-European Epicensus programme is to elevate the SoC for patients with psoriasis by creating a multistakeholder ‘Call-to-Action Framework’ to stimulate and drive positive change. Local adoption could encourage different stakeholders to collaborate and implement activities that align with the ‘Calls to Action’ to bring about these changes.
Insight gathering identified eight key themes that were explored through a modified Delphi technique. Consensus statements were used to inspire ‘Calls to Action’, developed by each stakeholder group separately but discussed together to find those common to all stakeholder groups. These common ‘Calls to Action’ are summarised in Table 11.
During the COVID-19 pandemic, utilisation of digital healthcare increased and widespread adoption of various technologies accelerated [31]. Stakeholders agreed that capitalising on this shift to digital and wider technology will be key to elevating the SoC for patients with psoriasis by providing additional communication channel options as long as: it is made as widely accessible as possible (for clinicians and patients alike), patients understand its value, and it does not increase clinicians’ workload. This must be a collaborative effort between clinicians, payors and patients to maximise success. Enabling access and upskilling all users of the technologies is essential [31] and requires additional funding. Governance of ‘sensitive’ data is a potential hurdle to implementation.
A coordinated effort to set up or support national registries was a clear ‘Call to Action’. The coordinated development of collaborative databases systematically recording clinically relevant outcomes including PROs was considered key to supporting guidelines and clinical practice. In France, the Transparency Commission integrated data from the national real-life registry of biotherapies (PSOBIOTEQ), using it as the basis for its recommendations in January 2022 to move several biologics from third-line treatments into the second line [32]. Educating patients on the value of RWD and evidence so they proactively contribute is important, but adequate data protection must be in place.
In terms of assessing QoL measures, or more broadly, PROs, stakeholders agreed that existing tools could be used, but visibility of lesions is not adequately or specifically assessed. Given the impact of visible lesions on QoL and work absenteeism [2, 21, 25], this is one obvious omission to address with a new, freely accessible tool.
Giving patients the opportunity to be involved in shared decision-making was seen as important, but shared decision-making in psoriasis needs more research to overcome existing barriers and demonstrate potential benefits [33].
Opinion varied on additional specialists needed in the MDT, possibly reflecting differences between countries. In France, for instance, internists are often consulted when patients present with multi-organ diseases. Guidelines that incorporate input from all relevant parties are likely to be the most beneficial. However, as noted here and previously [34], barriers to their implementation, including incomplete knowledge of guidelines, their complexity, and the complexity of psoriasis itself must be overcome. Literature supports an MDT approach to psoriatic disease management. A report from Portugal showed the many different models of combined dermatology–rheumatology clinics in existence, but further evaluation of obstacles and benefits is needed to optimise care [35]. A working group explored barriers to best practice in PsA, concluding that a fully integrated, collaborative, multidisciplinary, patient-focused approach is required for optimal care [36], and in psoriasis, Eissing and colleagues suggest that addressing related barriers simultaneously is required to effect change [34].
All stakeholders require education on comorbidities; clinicians so they are aware of the full range and consult the appropriate specialists as needed, payors so they understand the broader implications of psoriasis on patients, and the healthcare system and patients so they understand the full extent of their condition. This agrees with a study examining whether patients with psoriasis or PsA recognised that they were being monitored for comorbidities associated with their condition. It concluded that patient education needs to be improved owing to discrepancies between patient responses and physician records about the presence and treatment of comorbidities [37].
Stakeholders agreed that multistakeholder initiatives are beneficial; performing activities in siloes only perpetuates existing knowledge gaps and barriers to collaborative working. Central to this is educating and motivating patients to participate in the widest range of activities, from R&D to clinical trials and beyond, with outcomes and data communicated back to patients. However, while patient advocacy groups (PAGs) have a role in clinical trial design, etc., careful planning is required, as their capacity is limited, and therefore, they are unable to be involved in all initiatives.
The ‘Calls to Action’ span a broad range of areas pertinent to psoriasis care and vary widely in their ease and speed of potential implementation. ‘Calls to Action’ relating to education could be quick to implement. Some aspects of digital healthcare and other technologies are already being utilised and these could be built upon and refined in line with the ‘Calls to Action’. Others, however, including the development of guidelines, may be more complex and time consuming to implement. Initial groundwork may be necessary, for example, to agree upon the specialist input needed as well as consultation with payors to agree upon the data needed to support early adoption of innovative therapies.
Several ‘Calls to Action’ are interconnected. The need for consistent recording of PROs links several themes. It is integral to improving digital healthcare, RWD and RWE generation and input into registries. Digitally upskilled patients consistently collecting PRO data may also contribute to the relevance of guidelines by providing data via registries or other RWE studies. Educational tools and reminders texted to patients improved clinical outcomes, adherence, and the patient–physician relationship in a pilot study [38], suggesting that improving education and digital healthcare could have positive effects. Another study compared a structured, multidisciplinary, patient education programme with usual psoriasis care and found that while QoL and disease severity did not differ between the groups, compared with usual care, the educational intervention improved patient knowledge of psoriasis and patient satisfaction with disease management which, nonetheless, are valuable outcomes [39]. This may lead to patients becoming more knowledgeable, engaged, and motivated to contribute to discussions aimed at improving MDT working and the patient pathway, thereby impacting other ‘Calls to Action’. Improved education and healthcare systems could lead to an improvement in patient access and enable other areas to then be tackled, such as multistakeholder engagement and the relevance and reach of guidelines.
The Epicensus programme has several strengths, notably the inclusion of three key stakeholder groups involved in the care and management of psoriasis: clinicians (dermatologists), payors and patient representatives, and over ten countries across Europe are represented, bringing a truly pan-European perspective. There was input from a large cohort of stakeholders and the opportunity for discussion both within and across stakeholder groups allowed for a unique depth of alignment on the ‘Calls to Action’. Taking place throughout 2021, this initiative has benefited from lessons learned during the COVID-19 pandemic in terms of innovative ways to optimise clinical practice, patient support and care. Limitations include the relatively large number of clinicians, represented solely by dermatologists, compared with the payors and patient representatives (mitigated by establishing a weighted consensus and having a lead from each stakeholder group to ensure equal representation in discussions). The low number of payors also meant that the diversity of European healthcare systems was not comprehensively covered, but extending discussion of the ‘Calls to Action’ to more members of the under-represented stakeholder groups would help to allay this limitation. Not all the consensus statements were discussed at the Consensus Council meetings. For example, appropriate integration of psychological screening or support so it is readily accessible to patients was agreed upon but ‘Calls to Action’ were not generated. A more complete ‘Call-to-Action Framework’ could be established if the remaining statements were used to generate ‘Calls to Action’. Having an industry sponsor can be seen as a limitation, but the questionnaires and Delphi e-surveys were completed by stakeholders independently and the sponsor did not take an active part in the Consensus Council meetings.
Themes highlighted by this initiative align well with other studies. Interviews conducted with dermatology outpatients with psoriasis revealed how the burden of psoriasis beyond the skin is not adequately addressed in consultations, including the psychosocial impact of the disease. The study concluded that patient education to improve knowledge and self-management is necessary and structural changes to dermatology services are needed [40]. Overlap with issues in psoriasis care identified a decade ago include the reach of guidelines, consistent use of assessment tools and improving access to new therapies and ongoing care [41], highlighting the enduring need for action to adequately address long-standing challenges. Results of a German national programme in psoriasis between 2004 and 2017 demonstrated that a coordinated programme targeting specific goals can successfully contribute to better quality of care [42, 43]. A similar systematic approach to determine improvements after implementation of initiatives designed to address the ‘Calls to Action’ presented here would be valuable.
Conclusions
The fact that this programme highlights that areas identified for intervention a decade ago remain unaddressed is a timely wake-up call – simply recognising an area of unmet need is not sufficient to effect change. Practical steps must now be taken to implement change that translates into improvements in the management of patients with psoriasis that contribute to an elevation in the standard of care. Therefore, the hope is that the Epicensus ‘Call-to-Action Framework’ provides the focus and impetus for all stakeholders involved in the care of people with psoriasis to engage in coordinated activities to address the ‘Calls to Action’ and elevate the standard of care. This next stage of the programme will take us nearer our vision of a truly integrated, collaborative, patient-centric approach to psoriasis management where patients are diagnosed early, managed by the right specialists incorporating digital healthcare as appropriate, supported by relevant education, and treated promptly with innovative therapies. In addition, patient-relevant data will be consistently collected using robust, specific tools to generate RWE to inform guidelines that are widely disseminated and followed, elevating the standard of care for patients with psoriasis. This in turn could help alleviate the long-term costs and cumulative life-long burden that this chronic, incurable disease places on healthcare systems and patients.
Change history
09 August 2023
A peer-reviewed video abstract, infographic and plain language summary was retrospectively added to this publication.
References
Boehncke WH. Systemic inflammation and cardiovascular comorbidity in psoriasis patients: causes and consequences. Front Immunol. 2018;9(579):20180405. https://doi.org/10.3389/fimmu.2018.00579.
Griffiths CEM, Jo SJ, Naldi L, et al. A multidimensional assessment of the burden of psoriasis: results from a multinational dermatologist and patient survey. Br J Dermatol. 2018;179:173–181. https://doi.org/10.1111/bjd.16332.
Cohen BE, Martires KJ, Ho RS. Psoriasis and the risk of depression in the US population: national health and nutrition examination survey 2009–2012. JAMA Dermatol. 2016;152:73–9. https://doi.org/10.1001/jamadermatol.2015.3605.
Queiro R, Coto P. Multidisciplinary care for psoriatic disease: where we are and where we need to go. Rheumatology (Oxford). 2017;56:1829–31. https://doi.org/10.1093/rheumatology/kew485.
Tillett W, Merola JF, Thaci D, et al. Disease characteristics and the burden of joint and skin involvement amongst people with psoriatic arthritis: a population survey. Rheumatol Ther. 2020;7(617–637):20200722. https://doi.org/10.1007/s40744-020-00221-8.
Griffiths CEM, Armstrong AW, Gudjonsson JE, et al. Psoriasis. Lancet. 2021;397:1301–15. https://doi.org/10.1016/S0140-6736(20)32549-6.
Grine L, de la Brassinne M, Ghislain PD, et al. A Belgian consensus on the definition of a treat-to-target outcome set in psoriasis management. J Eur Acad Dermatol Venereol. 2020;34(676–684):20200102. https://doi.org/10.1111/jdv.16104.
Maul JT, Navarini AA, Sommer R, et al. Gender and age significantly determine patient needs and treatment goals in psoriasis—a lesson for practice. J Eur Acad Dermatol Venereol. 2019;33(700–708):20190115. https://doi.org/10.1111/jdv.15324.
Luelmo J, Gratacos J, Moreno Martinez-Losa M, et al. Multidisciplinary psoriasis and psoriatic arthritis unit: report of 4 years’ experience. Actas Dermosifiliogr. 2014;105(371–377):20131218. https://doi.org/10.1016/j.ad.2013.10.009.
Boehncke WH, Horvath R, Dalkilic E, et al. Association between clinical specialty setting and disease management in patients with psoriatic arthritis: results from LOOP, a cross-sectional, multi-country, observational study. J Eur Acad Dermatol Venereol. 2020;34(2035–2043):20200306. https://doi.org/10.1111/jdv.16251.
Baum EW, Schwartzman S. ALIGN PsA: advancing a multidisciplinary approach in PsA. Semin Cutan Med Surg. 2018;37:S125–34. https://doi.org/10.12788/j.sder.2018.057.
Hjuler KF, Dige A, Agnholt J, et al. Effectiveness of interdisciplinary combined dermatology-gastroenterology-rheumatology clinical care compared to usual care in patients with immune-mediated inflammatory diseases: a parallel group, non-blinded, pragmatic randomised trial. BMJ Open. 2021;11(e041871):20210428. https://doi.org/10.1136/bmjopen-2020-041871.
Clincialtrials.gov. Effectiveness of interdisciplinary care compared to usual care in patients with immune-mediated inflammatory diseases (NCAS-1). Available at: https://clinicaltrials.gov/ct2/show/NCT04200690 (last accessed 01 Mar 2022).
Brahmbhatt DH, Ross HJ, Moayedi Y. Digital technology application for improved responses to health care challenges: lessons learned from COVID-19. Can J Cardiol. 2022;38:279–91. https://doi.org/10.1016/j.cjca.2021.11.014 (20211201).
Tysome JR. Improving clinical practice in ENT: lessons learnt from the COVID-19 pandemic. Clin Otolaryngol. 2021;46:295–6. https://doi.org/10.1111/coa.13720.
Sbidian E, Chaimani A, Afach S, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database Syst Rev. 2020;1:CD011535. https://doi.org/10.1002/14651858.CD011535.pub3 (20200109).
Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80:1073–113. https://doi.org/10.1016/j.jaad.2018.11.058 (20190213).
World Health Organization. Global Report on Psoriasis. 2016. Available at: https://apps.who.int/iris/bitstream/handle/10665/204417/9789241565189_eng.pdf?sequence=1&isAllowed=y (last accessed 14 Mar 2022).
World Health Assembly. Resolution WHA67.9. 2014. Available at: https://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R9-en.pdf (last accessed: 14 Mar 2022).
Armstrong A, Jarvis S, Boehncke WH, et al. Patient perceptions of clear/almost clear skin in moderate-to-severe plaque psoriasis: results of the Clear About Psoriasis worldwide survey. J Eur Acad Dermatol Venereol. 2018;32(2200–2207):20180731. https://doi.org/10.1111/jdv.15065.
Jullien D, Paul C, Shourick J, et al. Psoriasis: frequency and reasons for absenteeism results from a study on 1609 active patients. J Eur Acad Dermatol Venereol. 2021;35:e301–3. https://doi.org/10.1111/jdv.17056 (20201221).
Richard MA, Paul C, De Pouvourville G, et al. Out-of-pocket expenditures in France to manage psoriasis in adult patients: results from an observational, cross-sectional, non-comparative, multicentre study. J Eur Acad Dermatol Venereol. 2021;35:912–8. https://doi.org/10.1111/jdv.17000 (20201208).
Al Sawah S, Foster SA, Goldblum OM, et al. Healthcare costs in psoriasis and psoriasis sub-groups over time following psoriasis diagnosis. J Med Econ. 2017;20:982–90. https://doi.org/10.1080/13696998.2017.1345749 (20170711).
Thomsen SF, Skov L, Dodge R, et al. Socioeconomic costs and health inequalities from psoriasis: a cohort study. Dermatology. 2019;235:372–9. https://doi.org/10.1159/000499924 (20190625).
da Silva N, Augustin M, Langenbruch A, et al. Disease burden and treatment needs of patients with psoriasis in sexually-sensitive and visible body areas: results from a large-scale survey in routine care. Eur J Dermatol. 2020;30:267–78. https://doi.org/10.1684/ejd.2020.3768.
Griffiths CEM, Augustin M, Naldi L, et al. Patient-dermatologist agreement in psoriasis severity, symptoms and satisfaction: results from a real-world multinational survey. J Eur Acad Dermatol Venereol. 2018;32:1523–9. https://doi.org/10.1111/jdv.14937 (20180713).
Korman NJ, Zhao Y, Pike J, et al. Satisfaction with current psoriasis treatment: misalignment between physician and patient perceptions. Dermatol Online J. 2016;22:20160715.
Cinelli E, Fabbrocini G, Megna M. Real-world experience versus clinical trials: pros and cons in psoriasis therapy evaluation. Int J Dermatol. 2022;61:e107–8. https://doi.org/10.1111/ijd.15644 (20210504).
Masson Regnault M, Castaneda-Sanabria J, Diep Tran MHT, et al. Users of biologics in clinical practice: would they be eligible for phase III clinical studies? Cohort study in the French Psoriasis Registry PSOBIOTEQ. J Eur Acad Dermatol Venereol. 2020;34:293–300. https://doi.org/10.1111/jdv.15878 (20191017).
Helliwell PS, Favier G, Gladman DD, et al. Best-practice indicators in psoriatic disease care. J Rheumatol Suppl. 2019;95:38–45. https://doi.org/10.3899/jrheum.190120.
Golinelli D, Boetto E, Carullo G, et al. Adoption of digital technologies in health care during the COVID-19 pandemic: systematic review of early scientific literature. J Med Internet Res. 2020;22: e22280. https://doi.org/10.2196/22280 (20201106).
The Transparency Commission. Journal officiel électronique authentifié n° 0020 du 25/01/2022. January 2022. Available at: https://www.legifrance.gouv.fr/download/pdf?id=u5ptDq3Zoqs1KEtFiRsvFXbDxD8eaE0g2h-finnZFg0= (last accessed 10 Feb 2022).
Larsen MH, Hagen KB, Krogstad AL, et al. Shared decision-making in psoriasis: a systematic review of quantitative and qualitative studies. Am J Clin Dermatol. 2019;20:13–29. https://doi.org/10.1007/s40257-018-0390-5.
Eissing L, Radtke MA, Zander N, et al. Barriers to guideline-compliant psoriasis care: analyses and concepts. J Eur Acad Dermatol Venereol. 2016;30:569–75. https://doi.org/10.1111/jdv.13452 (20151104).
Mendes-Bastos P, Nero P, Ferreira P, et al. A multidisciplinary approach in psoriatic disease: the different models of dermatology-rheumatology collaborations in Portugal. Acta Reumatol Port. 2021;46:333–41.
Betteridge N, Boehncke WH, Bundy C, et al. Promoting patient-centred care in psoriatic arthritis: a multidisciplinary European perspective on improving the patient experience. J Eur Acad Dermatol Venereol. 2016;30:576–85. https://doi.org/10.1111/jdv.13306 (20150916).
Patel P, Rosen CF, Chandran V, et al. Addressing comorbidities in psoriatic disease. Rheumatol Int. 2018;38:219–27. https://doi.org/10.1007/s00296-017-3895-y (20171128).
Balato N, Megna M, Di Costanzo L, et al. Educational and motivational support service: a pilot study for mobile-phone-based interventions in patients with psoriasis. Br J Dermatol. 2013;168:201–5. https://doi.org/10.1111/j.1365-2133.2012.11205.x (20121213).
Jendoubi F, Balica S, Richard MA, et al. A multicentre randomised controlled study evaluating the effect of a standardised education programme on quality of life, disease severity, and disease knowledge in patients with moderate-to-severe psoriasis: the EDUPSO study. Dermatology. 2021. https://doi.org/10.1159/000520289 (20211209).
Khoury LR, Skov L, Moller T. Facing the dilemma of patient-centred psoriasis care: a qualitative study identifying patient needs in dermatological outpatient clinics. Br J Dermatol. 2017;177:436–44. https://doi.org/10.1111/bjd.15292 (20170504).
Augustin M, Alvaro-Gracia JM, Bagot M, et al. A framework for improving the quality of care for people with psoriasis. J Eur Acad Dermatol Venereol. 2012;26(Suppl 4):1–16. https://doi.org/10.1111/j.1468-3083.2012.04576.x.
Augustin M, Eissing L, Langenbruch A, et al. The German national program on psoriasis health care 2005–2015: results and experiences. Arch Dermatol Res. 2016;308:389–400. https://doi.org/10.1007/s00403-016-1637-8 (20160405).
Langenbruch A, Mohr N, Kirsten N, et al. Quality of psoriasis care in Germany—results from the nationwide health care studies PsoHealth 2004–2017. J Eur Acad Dermatol Venereol. 2021;35:1536–42. https://doi.org/10.1111/jdv.17220 (20210507).
Acknowledgements
The authors would like to thank Anusha Patel for her participation in the Delphi voting, contributions at the Consensus Council meetings and for critical review of the manuscript. They would also like to thank Marcello Pani and David Trigos for their participation in the Delphi voting and contributions at the Consensus Council meetings. In addition, the authors would like to thank the clinicians, payors and patient representatives who completed the questionnaire providing valuable insights to initiate this programme. RBW is supported by the Manchester NIHR Biomedical Research Centre.
Funding
This programme, and the journal’s Rapid Service fee, was funded by UCB Pharma.
Medical Writing and Editorial Assistance
Medical writing and editorial assistance were provided by Laura Harrington PhD, Ogilvy Health UK and funded by UCB Pharma.
Author Contributions
All the authors contributed to the Delphi exercise and participated in the Consensus Council meetings and the generation of Calls to Action. The first draft of the manuscript was written by Laura Harrington, PhD, under direction from the authors, and all authors critically reviewed the manuscript for important intellectual content and approved the final draft.
Disclosures
All authors received an honorarium from UCB for participating in the Delphi surveys and the Consensus Council meetings. Jan Koren, Valeria Corazza, Menno A de Rie, and Marius Grosser have no other competing interests to declare. Jo Lambert has received grants/contracts from AbbVie, Almirall, Celgene, Eli Lilly, Janssen-Cilag, LEO Pharma, Novartis, UCB; consulting fees from AbbVie, BMS, Celgene, Eli Lilly, Janssen-Cilag, LEO Pharma, Novartis and UCB; and payment/honoraria for activities such as lectures/presentations/speaker bureaus from AbbVie, Almirall, BMS, Janssen-Cilag, Pifzer and UCB. Simon F Thomsen has received research support from Janssen, LEO Pharma, Novartis and UCB; and has served on advisory boards for Eli Lilly, Janssen, LEO Pharma, Novartis, Pfizer, UCB, Union Pharmaceuticals; and as a speaker for LEO Pharma, Novartis and UCB and has been the recipient of a travel grant to GUF and EADV from Novartis. Helen McAteer has received core funding support, paid to her employer, from Abbvie, Almirall, Amgen, Eli Lilly, Janssen, LEO Pharma, Novartis and UCB; and honoraria, paid to her employer, from Amgen and Novartis. Gabriella Fabbrocini has been principal investigator of clinical trials sponsored by and/or has received personal fees from AbbVie, abiogeny, Almirall, Celgene, Eli Lilly, LEO Pharma, Novartis, Sanofi and UCB. Denis Jullien reports personal fees from UCB, during the conduct of the study; personal fees and non-financial support from Abbvie, personal fees and non-financial support from Janssen-Cilag, personal fees and non-financial support from UCB, personal fees and non-financial support from Novartis, personal fees from Almirall, personal fees and non-financial support from Lilly, personal fees from MEDAC, personal fees from Celgene, personal fees from Bristol Myers Squibb, personal fees from Boehringer Ingelheim, outside the submitted work. Matthias Augustin has received consulting fees from AbbVie, Almirall, Amgen, Biogen, Boehringer Ingelheim, Celgene, Centocor, Eli Lilly, GSK, Hexal, Janssen, LEO Pharma, Medac, Merck, MSD, Mundipharma, Novartis, Pfizer, Sandoz, UCB Pharma and Xenoport. Richard B Warren has received grants/contracts from AbbVie, Almirall, Janssen, Lilly, LEO, Novartis, Pfizer and UCB; consulting fees from AbbVie, Almirall, Amgen, Arena, Astellas, Avillion, Biogen, Boehringer Ingelheim, BMS, Celgene, DiCE, GSK, Janssen, Lilly, LEO, Novartis, Pfizer, Sanofi, Sun Pharma, UNION and UCB; payment/honoraria for activities such as lectures/presentations/speaker bureaus from AbbVie, Almirall, Boehringer Ingelheim, BMS, Celgene, Janssen, Lilly, LEO, Novartis, Pfizer, Sanofi, Sun Pharma and UCB. Elizabeth Lazaridou has received research grants to her department from AbbVie, Genesis Pharma, Janssen, LEO, Lilly, Novartis, Pfizer and UCB; honoraria for activities such as lectures/presentations/speaker bureaus from AbbVie, Genesis Pharma, Janssen, LEO, Lilly, Novartis and UCB; support for attending meetings and/or travel from AbbVie, Janssen, LEO, Lilly and UCB; and has participated on a Data Safety Monitoring Board or Advisory Board for AbbVie, Genesis Pharma, Janssen, LEO, Lilly, Novartis, Pfizer and UCB. Lluís Puig has received grants/support paid to his institution from AbbVie, Almirall, Amgen, Boehringer Ingelheim, LEO Pharma, Lilly, Novartis, Pfizer, Sanofi and UCB; consulting fees from Abbvie, Almirall, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Janssen, Leo-Pharma, Lilly, Novartis, Pfizer, Sandoz, Sanofi, and UCB; and payment/honoraria for activities such as lectures/presentations/speaker bureaus for Janssen, Lilly and Novartis. Loïc Guillevin has served as a consultant for Boehringer Ingelheim, Certara, ESAI, GSK, Lilly, Novartis, Novo Nordisk, Roche, Sanofi, UCB Pharma. Wolf-Henning Boehncke has received payment/honoraria for activities such as lectures, presentations, speaker bureaus and has participated on Data Safety Monitoring Boards/Advisory Boards for AbbVie, Almirall, BMS, Celgene, Janssen, LEO, Lilly, Novartis, Pfizer and UCB.
Compliance with Ethics Guidelines
This manuscript is formed of the opinions of the authors themselves. There was no need to collect any type of patient data. Hence, the approval of an Ethics Committee was not required. Consent was obtained from all participants as they were contracted by UCB Pharma to take part in this programme.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Koren, J., Lambert, J.L.W., Thomsen, S.F. et al. Elevating the Standard of Care for Patients with Psoriasis: ‘Calls to Action’ from Epicensus, a Multistakeholder Pan-European Initiative. Dermatol Ther (Heidelb) 13, 245–268 (2023). https://doi.org/10.1007/s13555-022-00846-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00846-3