Abstract
Erlotinib (Tarceva®) is a drug used for the treatment of non-small cell lung cancer in patients with epidermal growth factor receptor (EGFR) mutations. Since EGFR is expressed in the skin, EGFR inhibitors commonly develop cutaneous side effects such as acneiform eruption, paronychia, telangiectasias, and abnormal eyelash growth. A 56-year-old man and a 46-year-old man visited the dermatology clinic complaining of yellowish papuloplaques and acneiform eruption on the face. They had been treated with erlotinib for lung cancer. Since patients using EGFR inhibitors are increasing, physicians should be aware that xanthomatous change can occur in severe acneiform eruptions after erlotinib treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients using EGFR inhibitors are increasing, and physicians should be aware that xanthomatous change can occur in severe acneiform eruptions after erlotinib treatment. |
Severe skin rash in patients may not be a worrying factor regarding treatment outcome. |
Xanthomatous lesions spontaneously cleared as the acneiform eruptions improved, and active treatment may not be necessary for perifollicular xanthoma lesions after erlotinib therapy. |
Introduction
Epidermal growth factor receptors (EGFR) activation is important in several cell functions, such as cell proliferation, differentiation, and angiogenesis. Thus, EGFR are important in the progression and development of many solid tumors. EGFR is overexpressed in approximately 80% of colorectal cancers and up to 93% of non-small cell lung cancers. So, for patients refractory or intolerant to chemotherapy, it is an important target structure in tumor management. Erlotinib is an oral tyrosine kinase inhibitor that targets the EGFR. It has been highly effective in the management of non-small cell lung cancer and pancreatic cancer that is resistant to chemotherapy.
During cancer treatment using EGFR blockade, many cutaneous side-effects are encountered because EGFR is also expressed in normal epidermis, the outer root sheath of the hair follicles, sebaceous glands, and sweat glands [1]. Reports show that, within 3 weeks of starting erlotinib, 75% of patients developed skin reactions [2, 3]. The most frequent skin lesion is acneiform eruption, but pruritus, xerosis, paronychia, periungual granuloma, telangiectasia, hair changes, and hyperpigmentation are also known [4,5,6]. Herein, we report two cases of yellowish papular eruption accompanied by typical acneiform skin eruption that occurred after erlotinib treatment.
Case
Patient 1
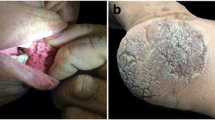
A 56-year-old man visited the dermatology clinic complaining of pruritic acneiform rash. He was diagnosed with non-small cell lung cancer (stage IB) and bone metastasis. He had started taking erlotinib (Tarceva®), and 7 days after commencing treatment, he developed intense pruritic acneiform rash on his face, and subsequently yellow papules also appeared on both cheeks. On physical examination, inflammatory papulopustules and papules with distinct yellowish papular eruption were noticed on both cheeks (Fig. 1A, B). Laboratory test results were within normal range, and the lipid panel did not show any signs of dyslipidemia. Skin biopsy from the yellowish papular lesion showed foamy histiocytes around the hair follicles with lymphocyte infiltration around the hair follicles and blood vessel (Fig. 2A, B). The patient continued erlotinib (Tarceva®) treatment, and the skin lesions gradually improved without any active treatment (Fig. 3A, B).
Patient 2
A 46-year-old man diagnosed with non-small cell lung cancer (stage IVA) and liver metastasis visited the dermatology clinic after aggravation of some pruritic acneiform rash on his scalp. The lesions appeared a few days after starting erlotinib (Tarceva®). On physical examination, inflammatory papulopustules and papules with crusted plaques were noticed on his face and scalp. Also, yellowish papular eruption was noticed on both cheeks (Fig. 4). Laboratory test results were within normal range, except for elevated liver enzymes due to liver metastasis. Lipid panel did not show any signs of dyslipidemia. The patient was reluctant to receive a biopsy and was treated based on clinical findings. The acneiform eruption and seborrheic dermatitis-like eruption improved after being treated with minocycline 100 mg/day, and the perifollicular xanthoma lesions also improved without further treatment (Fig. 5).
Discussion
Acneiform eruption is one of the most common cutaneous side effects that occur after EGFR inhibitor treatment. Unlike common acne, there are no comedones involved and patients may have pruritic symptoms. The pathomechanism of skin reactions that occur after EGFR inhibitor treatment is not fully established. EGFR-targeted therapies may unblock cutaneous chemokine production, which may affect the immune system, resulting in leukocyte chemotaxis and skin infiltration [7]. It may also inhibit EGFR signaling on epidermal and adnexal epithelium [6]. Increased apoptosis, altered keratinocyte differentiation, enlarged hair follicles, keratin plugs, thinning of the stratum corneum, and inflammatory cell infiltration are some histological features of EGFR-induced skin reactions [8]. In our case, the perifollicular xanthomatous skin reaction of yellowish papules was associated with a typical EGFR inhibitor-induced acneiform skin reaction. In acneiform eruptions, destructive ascending folliculitis accompanied by rupture of the acroinfundibulum occurs, and the inflammatory process continues until the affected follicular sebaceous units are completely destroyed. Accumulation of macrophages is required during resorption of the destroyed epithelial tissue and sebaceous glands, which ultimately results in a histiocytic and partly xanthomatous clearing reaction. This xanthomatous clearing reaction may cause the clinically distinctive, yellowish appearance [1].
Differential diagnosis for our patient may include diffuse normolipemic plane xanthoma (DNPX) and Favre–Racouchot syndrome (FRS). DNPX forms symmetric yellowish-orange plaques involving the periorbital region, neck, upper trunk, buttocks, and flexures. It may be associated with multiple myeloma and monoclonal gammopathy or another lymphoproliferative disorder [9]. Histologic findings show cluster of foamy histiocytes in the superficial dermis between the collagen fibers, and variable numbers of lymphocytes, Touton giant cells, and foamy histiocytes can be seen [9]. Unlike perifollicular xanthomas, the lesions are neither perifollicular localized nor predominately present on the cheeks. FRS is characterized by presence of large, open, black comedones on diffuse yellowish hue, usually distributed symmetrically on the temporal and periorbital areas. Histologic features of FRS show multiple comedones filled with keratinous material, dilatation, and hyperkeratosis of the follicular infundibulum and epidermal cyst formation. Evidence of significant solar elastosis is present with signs of epidermal atrophy and basophilic degeneration of the upper dermis [10]. Although our patients’ lesions were distributed on sun-exposed areas, the histologic finding did not show any solar damage, nor cysts or comedones.
Our case showed that not only EGFR-blocking monoclonal antibody treatment such as panitumumab or cetuximab but also low-molecular-weight tyrosine kinase inhibitor erlotinib can cause perifollicular xanthomas. Similar to a case described by Eames et al. [1], the perifollicular xanthomatous skin reaction of yellowish papules began as or was accompanied by a typical EGFR inhibitor-induced acneiform skin reaction. Thus, severe early-onset acneiform eruption may be a predisposing factor in patients with xanthomatous change after EGFR treatments. When xanthomas are associated with underlying hyperlipidemia, medical treatment may be considered. In cases where medical treatment does not help, patients may undergo surgery, laser, or cryosurgery. Laser treatments with pulsed dye laser, erbium-YAG laser, and Q-switched Nd-YAG laser have been reported to be effective [11, 12]. However, in our patients, the xanthomatous lesions gradually cleared as the acneiform eruptions improved, thus active treatment may not be necessary for perifollicular xanthoma lesions after erlotinib therapy.
Although erlotinib-induced acneiform eruption is a relatively common finding, perifollicular xanthoma lesions may not be so common. Severe destruction of the affected follicular sebaceous units followed by histiocytic and xanthomatous clearing reaction may be required for the pathogenesis. Since disease onset, severity, immune response, and pharmacogenetics vary among patients, it may result in different clinical outcomes. However, further investigations are required to clarify these findings. Reports have shown that cutaneous side effects represent a significantly strong predictor of the efficacy of EGFR inhibitors for non-small cell lung cancer treatment [13]. Hence, severe skin rash in patients may not be a worrying factor regarding treatment outcome. To reassure patients and abstain from excessive treatment, physicians should be aware that xanthomatous change can occur in severe acneiform eruptions after erlotinib treatment.
References
Eames T, Kroth J, Flaig MJ, Ruzicka T, Wollenberg A. Perifollicular xanthomas associated with epidermal growth factor receptor inhibitor therapy. Acta Derm Venereol. 2010;90(2):202–3.
Soulieres D, Senzer NN, Vokes EE, Hidalgo M, Agarwala SS, Siu LL. Multicenter phase II study of erlotinib, an oral epidermal growth factor receptor tyrosine kinase inhibitor, in patients with recurrent or metastatic squamous cell cancer of the head and neck. J Clin Oncol. 2004;22:77–85.
Shepherd FA, Rodrigues Pereira J, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005;353:123–32.
Robert C, Soria J-C, Spatz A, et al. Cutaneous side-effects of kinase inhibitors and blocking antibodies. Lancet Oncol. 2005;6:491–500.
Heidary N, Naik H, Burgin S. Chemotherapeutic agents and the skin: an update. J Am Acad Dermatol. 2008;58:545–70.
Hu JC, Sadeghi P, Pinter-Brown LC, Yashar S, Chiu MW. Cutaneous side effects of epidermal growth factor receptor inhibitors: clinical presentation, pathogenesis, and management. J Am Acad Dermatol. 2007;56:317–26.
Segaert S, van Cutsem E. Clinical signs, pathophysiology and management of skin toxicity during therapy with epidermal growth factor receptor inhibitors. Ann Oncol. 2005;16:1425–33.
Segaert S, Taber nero J, Chosidow O, et al. The management of skin reactions in cancer patients receiving epidermal growth factor receptor targeted therapies. J Dtsch Dermatol Ges. 2005;3:599–606.
Marcoval J, Moreno A, Bordas X, Gallardo F, Peyri J. Diffuse plane xanthoma: clinicopathologic study of 8 cases. J Am Acad Dermatol. 1998;39:439–42.
Patterson WM, Fox MD, Schwartz RA. Favre-Racouchot disease. Int J Dermatol. 2004;43:167–9.
Fusade BT. Treatment of xanthelasma palpebrarum by 1064-nm Q-switched Nd:YAG laser: a study of 11 cases. J Dermatol. 2008;158:84–7.
Karsai S, Czarnecka A, Raulin C. Treatment of xanthelasma palpebrarum using a pulsed dye laser: a prospective clinical trial in 38 cases. Dermatol Surg. 2010;36:610–7.
Petrelli F, Borgonovo K, Cabiddu M, Lonati V, Barni S. Relationship between skin rash and outcome in non-small-cell lung cancer patients treated with anti-EGFR tyrosine kinase inhibitors: a literature-based meta-analysis of 24 trials. Lung Cancer. 2012;78(1):8–15.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the diagnosis and conception of the case report. The first draft of the manuscript was written by En Hyung Kim and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
En Hyung Kim, Dong Min Kim and Ji Yeoun Lee declare that they have no conflict of interest.
Compliance with Ethics Guidelines
Our manuscript meets the ethical standards of the Declaration of Helsinki of 1964 and its later amendments. The authors certify that they have obtained all appropriate patient consent forms for the publication of case details and images.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kim, E.H., Kim, D.M. & Lee, J.Y. Perifollicular Xanthoma Occurring in Patients after Erlotinib Treatment. Dermatol Ther (Heidelb) 12, 1281–1286 (2022). https://doi.org/10.1007/s13555-022-00739-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-022-00739-5