Abstract
Introduction
Generalized pustular psoriasis (GPP) is a rare, severe, and potentially life-threatening systemic and chronic autoinflammatory disease characterized by sterile, neutrophilic pustules. The standard of care for GPP varies by region, with limited information and experience of flares and their treatment. Our aim was to establish current unmet needs in GPP by better understanding the natural history of GPP, examining how dermatologists diagnose GPP and GPP flares, and establishing the range and adequacy of GPP treatment options currently prescribed by dermatologists.
Methods
Eligible dermatologists (N = 29) completed a 28-question structured survey, covering ten themes, ranging from GPP diagnostic criteria to GPP symptoms and treatment.
Results
All dermatologists stated that pustules were necessary to diagnose a GPP flare. The most frequently reported triggering factors for GPP were steroid withdrawal (64%), infection (58%), and stress (50%). Most dermatologists indicated that available treatment options for GPP flares were adequate “most” (79%) or “all” (14%) of the time. Despite this reported adequacy, 38% of dermatologists reported that it was at least “somewhat common” for a flare to require hospitalization. Furthermore, 72% of dermatologists indicated that treatments were too slow to control flares, and 66% indicated that treatments did not adequately prevent new flares at least “sometimes”.
Conclusion
This survey suggests that there are key features of GPP flares, and could initiate discussion around forming consensus guidelines for diagnosis and management. While the results suggest that moderately effective therapies may exist, the need for GPP-specific treatments remains.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Twenty-nine dermatologists with a history of treating patients with generalized pustular psoriasis (GPP) took part in a survey examining GPP diagnostic criteria, the natural history of GPP, and current GPP treatment options and their perceived adequacy. |
Overall, dermatologists agreed on a number of criteria for the diagnosis of GPP, and indicated that current treatments were too slow to control flares and did not adequately prevent new GPP flares. |
These results may help to inform a consensus guideline for GPP diagnosis and management. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13615151.
Introduction
Generalized pustular psoriasis (GPP) is a rare, severe, and potentially life-threatening systemic and chronic skin disease [1,2,3]. There is a lack of consensus over the precise diagnostic criteria that define GPP, and multiple subtypes have been proposed, ranging from the acute ‘von Zumbusch’ form to the milder ‘annular’ form [3, 4]. Nonetheless, in many patients, GPP is characterized by relapsing and remitting flares that consist of a disseminated skin rash with sterile neutrophilic pustules [2, 3, 5]. GPP is a distinct entity from plaque psoriasis and can occur independently from or in association with plaque psoriasis [2]. The severity of GPP flares varies between patients [1], and symptoms can last for several months. GPP can occur at any age, although it is less common in pediatric patients [3]. Despite treatment, most patients have residual disease post-flare [3, 6].
GPP causes significant morbidity and, in some cases, mortality [2, 3]; infectious, metabolic, cardiac, liver, respiratory, and neurological comorbidities have been reported [6]. Common triggers for flares include withdrawal of systemic steroids, certain medications, infections, stress, and pregnancy [1, 6]. Mortality rates as a direct result of GPP range from 3 to 25% [6,7,8]. However, GPP is rare, with global prevalence estimates being as low as 1.76/million [9], and while the prevalence of GPP in the USA is not well characterized, it is thought to be less than 1/10,000.
Despite the notable burden of disease for patients with GPP, its rarity means that standard of care varies by region due to the limited information available and lack of experience of flares and their treatment. There is a paucity of published data on the treatment of flares and post-flare disease activity [10], and while there are published overviews of the treatment of pustular psoriasis, they are outdated and are only considered to be recommendations [11]. There are no approved therapies for GPP in the USA or EU, and where biologic therapies are approved, their approval is based on small, open-label trials [12]. Currently, there is no cure for GPP [3].
To improve and build upon the limited consensus data and guidelines on GPP [5, 11, 13], we conducted a survey of dermatologists from the USA and Canada participating in the Corrona Psoriasis Registry with the aim to better characterize GPP. The Corrona Psoriasis Registry is a multicenter, observational disease-based registry that contains longitudinal data from both patients who are enrolled in the registry with a dermatologist-confirmed diagnosis of psoriasis, and their treating dermatologists, collected during routine clinical encounters using Corrona Registry surveys. The objectives of this survey were to better understand the natural history of GPP, how dermatologists diagnose GPP and acute GPP flares, the treatment options for GPP currently prescribed by dermatologists and their perceived adequacy, and to establish the challenges faced and unmet needs in the treatment of GPP.
Methods
Study Criteria
The Corrona GPP dermatologist survey was a descriptive, cross-sectional survey conducted to compile feedback from dermatologists on GPP and its treatment. Dermatologists in the Corrona Psoriasis Registry who were identified as likely to be currently treating patients with GPP were invited to participate in the survey. Invited dermatologists who had treated adult patients (age ≥ 18 years) with GPP within the past 5 years were eligible to participate in the survey. Dermatologists must have been at an active clinical center as of 10 September 2019 (N = 448) to be included, as identification of patients with pustules was based on registry data extracted on that date. While dermatologists were only required to have treated one patient in the Corrona Registry with generalized pustules in order to be eligible for survey participation, they were asked to report on all patients with GPP they had treated in the past 5 years, regardless of whether those patients were included in the Corrona Registry. The survey asked dermatologists to exclude patients with juvenile pustular psoriasis, localized forms of pustular psoriasis (i.e., palmoplantar pustulosis and acrodermatitis continua of Hallopeau), acute generalized exanthematous pustulosis, or pustulation restricted to psoriatic plaques.
The survey included 28 multiple choice questions across ten themes that explored GPP flare onset and diagnosis, flare frequency and duration, treatment of flares, treatment of residual disease, and dermatologists’ overall experience of managing patients with GPP (summarized in Table 1; the full survey is available in Electronic Supplementary Material [ESM] Table S1).
Data Collection
Dermatologists who fulfilled the study criteria outlined above (N = 32) were invited to participate in an online survey hosted on SurveyMonkey (ESM Table S1). Personalized links were used to track which dermatologists had completed the survey for follow-up and payment purposes. Following the first SurveyMonkey email, non-responders received daily email reminders through to the end of 1 week. After the first week, personalized follow-up emails and telephone calls from Corrona, LLC (Waltham, MA, USA) were initiated. Dermatologists were compensated for completing the survey.
Analyses
The frequencies of all responses were recorded, and a subgroup stratification of GPP dermatologists whose patients experienced flares frequently (≥ two times per year) versus less frequently (zero–one time per year) was carried out.
Compliance with Ethics Guidelines
Studies conducted by Corrona are covered under the Corrona PsO Registry IRB. However, the Corrona regulatory body concluded that this survey did not meet the definition of human subject research, and therefore did not require specific approval.
Results
Of the 32 invited dermatologists, two reported that they had not treated a patient with GPP in the past 5 years and so were not invited to participate further. Of the 30 eligible dermatologists, 29 responded (97% eligible response rate), although response rate varied by question (denoted in the tables and figures).
The participating dermatologists had been in practice for a mean of 25.7 (standard deviation 11.1) years, and the majority were board-certified (89.7%) with an MD qualification (93.1%). More participants were male than female (65.5 vs. 34.5%) and most participants worked in private rather than academic clinical settings (72.4%) (see ESM Table S2 for further details on participant demographics). Within the past 5 years, 21 participants had treated at least three patients with GPP; of those, 11 had treated ≥ five patients with GPP.
Diagnosis of GPP Flares
All dermatologists stated that pustules were necessary to diagnose a GPP flare, with the next most cited criteria being worsening of skin lesions (83%) and erythema (76%). The responses for other diagnostic criteria are reported in Table 2.
Natural History of GPP
Most dermatologists (69%) estimated that their patients had an average of zero or one GPP flare per year, while 28% estimated that their patients had an average of two to three flares per year (see Fig. 1). Over half of dermatologists (55%) reported that their patients’ flares typically last 2 to < 4 weeks, while 41% reported that flares typically last 1–3 months (see Fig. 1). The most common criteria for flares to be considered resolved were few to no pustules (83% of dermatologists), reduced to no erythema (83%), and minimal to no skin lesions (66%). The typical time to resolution of skin lesions was most commonly reported as 2 to < 4 weeks for pustules (52%), 1–3 months for erythema (48%), and 1–3 months for scaling (59%). Full responses for flare frequency, duration, and time to symptom resolution are captured in Fig. 1.
The most common triggering factors for GPP were cited by dermatologists as steroid withdrawal (“often” or “very often”, 64%), infection (“often” or “very often”, 58%), and stress (“often” or “very often”, 50%) (for the full results, see Table 3).
The Severity and Chronicity of GPP
Over a third of dermatologists (38%) reported that it was at least “somewhat common” for a flare to require hospitalization, while 21% reported that it was “very common” or “always required”. The most common durations of hospitalization were reported as 3–4 and 5–8 days (43 and 29% of dermatologists, respectively). Post-flare, 83% of dermatologists indicated that patients still had residual disease, with dermatologists most commonly citing the symptoms minimal skin scaling (76%), minimal skin lesions (66%), and reduced erythema (66%).
Treatment Options for GPP
To treat a GPP flare, the majority of dermatologists reported being “somewhat likely” or “very likely” to use the non-biologic treatments cyclosporine (85%, n = 28) and either acitretin or isotretinoin (56%, n = 29). Dermatologists also reported being “somewhat likely” or “very likely” to use the biologic treatments infliximab (53%, n = 28), ixekizumab (52%, n = 29), adalimumab (41%, n = 29), and secukinumab (41%, n = 29). When treating GPP flares, the most commonly endorsed symptoms for initiating, switching, or adding a treatment (non-biologic or biologic) were worsening skin lesions (97%, n = 29) and pustules (90%, n = 29).
Outside of a flare, dermatologists reported being “somewhat likely” or “very likely” to use topical steroids (83%, n = 29), secukinumab (62%, n = 29), ixekizumab (62%, n = 29), and adalimumab (56%, n = 29) to treat residual disease. The full responses from dermatologists on their use of biologic and non-biologic treatments for GPP flares and residual disease are given in Table 4.
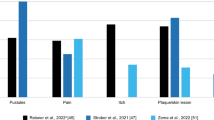
Perceived Adequacy of the Current Treatment Options
Most dermatologists indicated that existing treatment options for all flare frequencies are adequate “most” (79%) or “all” (14%) of the time, and 83% reported that treatments for residual disease for all flare frequencies are adequate “most of the time” (Fig. 2). However, 67% of GPP dermatologists whose patients flare frequently (≥ two times per year, n = 9) indicated that treatments “often” did not adequately prevent new flares, while the majority reported inadequacy at least “sometimes” (Fig. 3). In addition, 83% of dermatologists indicated that patients still had residual symptoms post-flare, while 72% considered available treatment options to be too slow to control flares “sometimes”, “often”, or “very often”, regardless of flare frequency (Fig. 3).
Discussion
The aims of this study were to explore the natural history of GPP, understand physicians’ diagnostic criteria for GPP flares, and examine common treatments for GPP and their perceived adequacy by dermatologists. There was a clear consensus on the criteria for diagnosis of a GPP flare, with all dermatologists citing pustules as necessary, and the majority also citing worsening skin lesions and erythema. Most respondents reported that patients had zero to one GPP flares per year, with flares typically lasting up to 3 months, and residual symptoms commonly taking up to 3 months to resolve. Responses from dermatologists participating in this survey suggest that immunosuppressants and topical retinoids remain common treatments for GPP, despite limited evidence demonstrating their efficacy in pustular disease [14, 15]. Current treatment methods were broadly perceived by dermatologists as being adequate, even though most respondents reported that patients had residual symptoms post-flare.
Challenges Facing the Treatment of GPP and Unmet Needs
These data suggest that fast-acting and long-lasting treatments for GPP are lacking: the most common duration of hospitalization was reported as 3–8 days, and GPP flares were reported to last up to 3 months. Furthermore, flare prevention was reported as “often a challenge” by 67% (n = 6) of dermatologists whose patients had an average of ≥ two flares per year. As most patients still have residual symptoms post-flare, current treatments for both GPP flares and chronic (post-flare) disease are often inadequate. The lack of GPP-specific approved therapies in the USA remains a barrier to effective treatment; practitioners may be unwilling to use potentially effective therapies (e.g., biologics) that are not indicated specifically for GPP. Therefore, there is a need for targeted therapies that directly address the pathophysiology of GPP, so that control of both flares and long-term disease is more easily attainable.
Limitations of the Current Study
A notable limitation of this study is that dermatologists were only asked to consider certain types of GPP; treated patients met inclusion criteria if they had generalized pustules, but no further specific history was collected. However, GPP is often described has having at least two clinical forms: ‘von Zumbusch’ or acute GPP, which is characterized by severe erythroderma, and ‘annular’ or subacute GPP, which has milder systemic symptoms [3, 4]. Furthermore, GPP can originate from multiple causes: a patient may have inherited GPP, or developed GPP acutely, but temporarily, due to the withdrawal of steroids or another psoriasis treatment [2, 11, 16, 17]. The Corrona Registry does not distinguish between these subtypes of GPP, but it is possible that patients with different subtypes have distinct histories and treatment requirements. This could be reflected in the slightly paradoxical results of dermatologists’ apparent overall satisfaction with current treatments, despite the clearly unresolved disease symptoms for many patients. This emphasizes the fact that while this study represents the first step toward better understanding of GPP, it does not capture the patient’s perspective on disease burden. Finally, these data are based on a sample of only 29 dermatologists, which limits the widespread application of the results.
Conclusions
The survey results suggest some consensus regarding dermatologists’ opinions on the clinical presentation of GPP and the nature/frequency of GPP flares. However, our findings also delineate a paradox in satisfaction with current treatments for GPP flares. While most dermatologists indicated that GPP flare treatments were adequate, they also report that the time to response was slow and that many patients had residual symptoms post-flare. The present lack of GPP-specific treatments may have affected dermatologists’ reported satisfaction with current treatments: there are no other effective alternatives, and dermatologists may view the currently available treatments as better than no treatment at all. The results do indicate that the use of plaque psoriasis therapies provide some benefits for patients with GPP, but unmet needs clearly remain; specifically, a better approach to the use of currently available therapies, and the development of novel therapies that safely control GPP flares long term.
The results of this study are expected to improve current clinical practice by contributing to the establishment of treatment guidelines for GPP. GPP flares appear to have common diagnostic criteria, including the presence of pustules, worsening skin lesions, and erythema; these results could initiate a discussion around forming consensus guidelines for diagnosis. Furthermore, we hope that these results will help to foster education regarding how experienced dermatologists use currently available therapies, as well as investigation into future effective therapies for GPP.
References
Umezawa Y, Ozawa A, Kawasima T, et al. Therapeutic guidelines for the treatment of generalized pustular psoriasis (GPP) based on a proposed classification of disease severity. Arch Dermatol Res. 2003;295(Suppl 1):S43-54.
Benjegerdes KE, Hyde K, Kivelevitch D, Mansouri B. Pustular psoriasis: pathophysiology and current treatment perspectives. Psoriasis (Auckl). 2016;6:131–44.
Ly K, Beck KM, Smith MP, Thibodeaux Q, Bhutani T. Diagnosis and screening of patients with generalized pustular psoriasis. Psoriasis (Auckl). 2019;9:37–42.
Guerreiro de Moura CA, de Assis LH, Góes P, et al. A case of acute generalized pustular psoriasis of von Zumbusch triggered by hypocalcemia. Case Rep Dermatol. 2015;7:345–51.
Navarini AA, Burden AD, Capon F, et al. European consensus statement on phenotypes of pustular psoriasis. J Eur Acad Dermatol Venereol. 2017;31:1792–9.
Choon SE, Lai NM, Mohammad NA, Nanu NM, Tey KE, Chew SF. Clinical profile, morbidity, and outcome of adult-onset generalized pustular psoriasis: analysis of 102 cases seen in a tertiary hospital in Johor. Malaysia Int J Dermatol. 2014;53:676–84.
Ryan TJ, Baker H. The prognosis of generalized pustular psoriasis. Br J Dermatol. 1971;85:407–11.
Zelickson BD, Muller SA. Generalized pustular psoriasis. A review of 63 cases. Arch Dermatol. 1991;127:1339–45.
Augey F, Renaudier P, Nicolas JF. Generalized pustular psoriasis (Zumbusch): a French epidemiological survey. Eur J Dermatol. 2006;16:669–73.
Zhou LL, Georgakopoulos JR, Ighani A, Yeung J. Systemic monotherapy treatments for generalized pustular psoriasis: a systematic review. J Cutan Med Surg. 2018;22:591–601.
Robinson A, Van Voorhees AS, Hsu S, et al. Treatment of pustular psoriasis: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2012;67:279–88.
Gooderham MJ, Van Voorhees AS, Lebwohl MG. An update on generalized pustular psoriasis. Expert Rev Clin Immunol. 2019;15:907–19.
Fujita H, Terui T, Hayama K, et al. Japanese guidelines for the management and treatment of generalized pustular psoriasis: the new pathogenesis and treatment of GPP. J Dermatol. 2018;45:1235–70.
Bachelez H. Pustular psoriasis and related pustular skin diseases. Br J Dermatol. 2018;178:614–8.
Johnston A, Xing X, Wolterink L, et al. IL-1 and IL-36 are dominant cytokines in generalized pustular psoriasis. J Allergy Clin Immunol. 2017;140:109–20.
Georgala S, Rigopoulos D, Aroni K, Stratigos J. Generalised pustular psoriasis precipitated by topical calcipotriol cream. Int J Dermatol. 1994;33:515–6.
Georgala S, Koumantaki E, Rallis E, Papadavid E. Generalized pustular psoriasis developing during withdrawal of short-term cyclosporin therapy. Br J Dermatol. 2000;142:1057–8.
Acknowledgments
We thank the participants of this study. We would also like to thank Christian Thoma for his contributions to the study.
Funding
This study was sponsored by Corrona, LLC and the analysis was funded by Boehringer Ingelheim. Access to study data was limited to Corrona, LLC, and Corrona statisticians completed all of the analysis; all authors contributed to the interpretation of the results. Corrona, LLC has been supported through contracted subscriptions in the past 2 years by AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Eli Lilly and Company, Genentech, Gilead, Janssen, Merck, Novartis, Ortho Dermatologics, Pfizer Inc., Regeneron, and Sun. The journal’s Rapid Service fee was funded by Boehringer Ingelheim.
Medical Writing Assistance
Medical writing support was provided by Imogen Allred, PhD, and Leigh Church, PhD, of OPEN Health Medical Communications, and funded by Boehringer Ingelheim.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
All authors were involved in the conceptual design of this manuscript, drafting and development, and agreement to publish. Data analysis was conducted by Rose Medeiros.
Disclosures
This study design and conduct were the result of a collaborative effort between Corrona, LLC and Boehringer Ingelheim. Bruce Strober reports being an investigator for AbbVie, Dermavant, Corrona, Dermira; speaker for AbbVie, Janssen, Ortho Dermatologics; consultant for AbbVie, Almirall, Amgen, Arena, Aristea Therapeutics, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Dermavant, Dermira, Janssen, LEO Pharma, Eli Lilly, Kyowa Hakko Kirin, Meiji Seika Pharma, Novartis, Pfizer, GlaxoSmithKline, UCB, Sun Pharma, Ortho Dermatologics, Regeneron, Sanofi-Genzyme; Scientific Director for Corrona, LLC. Mark Lebwohl is an employee of Mount Sinai; receives research funds from AbbVie, Amgen, Arcutis Biotherapeutics, AstraZeneca, Boehringer Ingelheim, Celgene, Clinuvel Pharmaceuticals, Eli Lilly, Incyte, Janssen, Kadmon Corporation, LEO Pharma, MedImmune, Novartis, Ortho Dermatologics, Pfizer, SCIderm, UCB, Vidac; consultant for Allergan, Almirall, Arcutis Biotherapeutics, Avotres Therapeutics, BirchBioMed, Boehringer Ingelheim, Bristol-Myers Squibb, Cara Therapeutics, Castle Biosciences, Corrona, Dermavant Sciences, Evelo, Foundation for Research and Education in Dermatology, Inozyme Pharma, LEO Pharma, Meiji Seika Pharma, Menlo, Mitsubishi, NeuroDerm, Pfizer, Promius Pharma/Dr. Reddy’s Laboratories, Theravance Biopharma, Verrica Pharmaceuticals. Nirali Kotowsky, Wendell C. Valdecantos, and Mary Flack are full-time employees of Boehringer Ingelheim. Amanda K. Golembesky reports being employed by Boehringer Ingelheim at the time of the study being conducted, but is currently employed by GlaxoSmithKline. Rachel H. Mackey was an employee of Corrona, LLC at the time of the study being conducted but is currently employed by Premier, Inc. Rose Medeiros is an employee of Corrona, LLC. Leslie R. Harrold is a shareholder and employee of Corrona, LLC.
Compliance with Ethics Guidelines
Studies conducted by Corrona are covered under the Corrona PsO Registry IRB. However, the Corrona regulatory body concluded that this survey did not meet the definition of human subject research, and therefore did not require specific approval.
Data Availability
The Corrona dataset is based on a large US North American multicenter study adhering to a number of institutional review boards, with complex logistics. Patients did not provide consent to raw data sharing during the data collection for this purpose, and the Corrona data-sharing policies do not permit raw data sharing for this purpose. An aggregated limited dataset from the current analyses is available to qualified investigators with an approved protocol. Data requests may be sent to Corrona, represented by Dr. Jeffrey D. Greenberg MD MPH, NYU School of Medicine, New York, NY, USA (e-mail jgreenberg@corrona.org).
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Strober, B., Kotowsky, N., Medeiros, R. et al. Unmet Medical Needs in the Treatment and Management of Generalized Pustular Psoriasis Flares: Evidence from a Survey of Corrona Registry Dermatologists. Dermatol Ther (Heidelb) 11, 529–541 (2021). https://doi.org/10.1007/s13555-021-00493-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-021-00493-0