Abstract
The prevalence of cardiac cachexia in chronic heart failure is approximately 5% to 15% and 18-month mortality rates can reach 50%. Treatment with angiotensin-converting enzyme inhibitors and beta-blockers may confer some benefit but no proven therapy exists. We tested the effects of an oral nutritional supplement in cachectic patients with heart failure. This was a prospective, randomized, double-blind, placebo-controlled pilot study which randomized 29 patients to a high-caloric (600 kcal) high-protein (20 g) oral nutritional supplement or placebo for a duration of 6 weeks in addition to the patients’ usual food intake. At baseline, 6 weeks, and 18 weeks, we measured body weight, quality of life, body composition, heart function, laboratory parameters, and exercise performance. Edema-free body weight increased in 19 of 20 patients receiving intervention at 6 weeks and in 17 of 19 patients at 18 weeks with an average weight gain of 2.0 ± 1.7 kg (3.1 ± 2.4%, p = 0.0001) and 2.3 ± 3.1 kg (3.6 ± 4.7%, p = 0.007) at 6 and 18 weeks, respectively. Most of the weight gain was fat tissue with an absolute gain of 1.5 ± 1.7 kg (p = 0.003) and 1.6 ± 2.7 kg (p = 0.008). A significant improvement in quality of life and decrease in serum levels of tumor necrosis factor-α were observed (p < 0.05 for both). We demonstrated the feasibility of oral nutritional supplement in cachectic patients with heart failure and significant clinical benefit in terms of body size and body composition, laboratory parameters, and quality of life (www.clinicaltrials.gov identifier NCT00654719).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
During the natural progression of heart failure (HF), a number of pathophysiological alterations lead to derangements in metabolic and inflammatory systems [1, 2, 3, 4, 5]. From a clinical perspective, whole body wasting and weight loss develop, which may eventually engender cachexia [6, 7]. The prevalence of cardiac cachexia in chronic HF is approximately 5% to 15% depending on its diagnostic criteria and HF severity [8]. With mortality rates of up to 50% at 18 months (in patients with at least 7.5% weight loss and a body mass index <24.0 kg/m2), the prognosis is grave and worse than that of most cancers [9]. Previous studies in patients with chronic HF demonstrated that treatment with angiotensin converting enzyme (ACE) inhibitors reduced the risk of weight loss [10] and treatment with beta-blockers induced modest gain in edema-free weight [11]. There, however, is no specific therapy for cachexia [12].
Nutritional aspects of the disease have not been studied in details thus far; however, it is generally believed that insufficient intake of protein and calorie may not necessarily cause cardiac cachexia but may maintain its progression or interfere with its correction [13]. Indeed, resting energy expenditure is increased in patients with this perturbation [14], but, total daily energy expenditure is reduced [15]. A number of clinical–experimental approaches have been tested including inhibition of cellular mechanisms of wasting, reduction of energy expenditure, and increase in energy supply, but no major benefit has been observed [16]. More practical approaches with oral nutritional supplements, either alone or in conjunction with other adjunct measures, have proven beneficial in some other chronic disease states [17, 18, 19, 20], but to the best of our knowledge oral nutritional interventions have not been tested in the setting of HF cachexia.
We have performed a prospective, randomized, double-blind, placebo-controlled pilot study to assess the effects of high-calorie high-protein diets in addition to normal food supply in patients with chronic HF and cachexia. We hypothesized that a high-calorie high-protein oral nutritional supplementation has beneficial effects on patients with established cardiac cachexia, manifested by modest gain in edema-free dry weight and through changes in plasma cytokine profile and lipoproteins as well as improved health-related quality of life.
2 Methods
2.1 Study design and participants
This was a prospective, randomized, double-blind, placebo-controlled pilot study in the Silesian Center for Heart Diseases, Zabrze, Poland. Patients aged 18–80 years with stable HF New York Heart Association (NYHA) functional class II–IV, left ventricular ejection fraction (LVEF) ≤30% and on a stable medication for at least 4 weeks, attending the out-patient clinic, were screened for edema-free weight loss >7.5% over a period of at least 6 months. Patients with signs of acute inflammatory processes, cancer, or severe chronic renal failure (serum creatinine >250 μmol/l) were excluded. A total of 29 subjects met the inclusion criteria and were eligible for randomization. All were on standard medical therapy for HF including ACE inhibitors, beta-blockers, spironolactone, and/or diuretics. The study protocol complied with the principles outlined in the Declaration of Helsinki. It was reviewed and approved by the Ethics Committee of the Silesian Medical University (Katowice, Poland) and all participants provided written informed consent before inclusion. This study was registered under the unique identifier NCT00654719 at www.clinicaltrials.gov.
2.2 Randomization and intervention
Upon enrolment, patients were randomized in a 3:1 fashion to receive either a high-caloric, high-protein oral nutrition or a matching placebo for 6 weeks. Randomization was performed blindly by the pharmacy department of the Silesian Center for Heart Diseases. No physician and investigator involved in clinical care or any laboratory assessment was aware of the patients’ assignments until study completion at 18 weeks. All patients were instructed to continue with their normal diet during the 6 weeks of intervention. Patients in the intervention arm consumed additional 600 kcal per day as a commercially available formulation NutriDrink® (proteins 20 g, carbohydrates 72 g, fat 26 g; Nutricia Inc. Numico, Amsterdam, The Netherlands—see Table 1), divided into two equal doses given between main meals in order to avoid appetite suppression. Patients in the placebo arm consumed matching placebo (12 kcal/day) of similar taste and consistency to assure for appropriate blinding.
2.3 Data collection
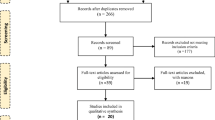
Patients were assessed at baseline, after 6 weeks of treatment and 12 weeks after treatment (18 weeks from study begin). The study protocol is outlined in Fig. 1. At each time point, we performed the following assessments: (1) body weight was measured under identical conditions and using the same weighing scale (B150L, Redwwag, Zawiercie, Poland); (2) quality of life using the Minnesota Living with Heart Failure Questionnaire (MLHFQ) in which higher values indicate lower quality of life; (3) body composition was measured using dual X-ray absorptiometry (DEXA) with a pencil beam Lunar DRX-L device, (General Electric, Brussels, Belgium); (4) serum level of inflammatory markers and lipoproteins; (5) LVEF by an echocardiogram (Sonos-3000 Hewlet-Packard Ultrasound Scanner; Hewlet-Packard, Andover, MA, USA); and (6) exercise capacity by 6-min walking-test and peak oxygen consumption during exercise testing using Vmax-229 ergospirometry platform (SensorMedics, Yorba Linda, CA, USA)
2.4 Laboratory measures
Blood samples were drawn at each visit after an overnight fast from an antecubital vein and after 15 min of rest in a semisupine position. Upon blood collection, blood samples were centrifuged, and plasma and serum aliquots were immediately frozen at −70°C. Cytokines were measured from serum samples using high sensitivity test kits purchased from R&D Systems Europe, (Abingden Oxon, UK). The lower limits of sensitivity were 0.106 pg/mL for tumor necrosis factor-α (TNFα), 0.77 pg/mL for soluble TNFα receptor (TNFR-1), 0.6 pg/mL for soluble TNFR-2. Plasma cholesterol, triglycerides, low-density lipoprotein (LDL), and high density lipoprotein (HDL) cholesterol were measured using commercially available reagents provided by Roche Diagnostics, Basel, Switzerland.
2.5 Statistical analysis
This was a pilot study with a randomization scheme favoring allocation to active therapy to enable therapeutic support for as many patients as possible. Due to the pilot character of the study, the possible imbalances between the study groups and the small size of the placebo group (and potential of mitigated power), the primary analyses were restricted to the patients in the active intervention group who completed 6 weeks therapy. The main purpose of the placebo group was to keep investigators and patients uncertain about the treatment allocation. Primary outcome measures were edema-free body weight and health-related quality of life. Secondary outcome measures were body composition, serum levels of inflammatory markers and lipoproteins, LVEF, and exercise capacity. Data are presented as mean value ± standard deviation or as mean value ± standard error of mean (SEM). Student t test for paired and unpaired samples, Wilcoxon signed rank test and Mann–Whitney U test were used as appropriate. Nominal variables were compared using the Chi-square test or Fisher’s exact test as appropriate. A p value <0.05 was considered significant. Statistical comparisons were carried out using Statistica v 6.0 (StatSoft Inc. Tulsa, OK, USA).
3 Results
A total of 29 subjects were enrolled into the study: 23 were started on oral nutritional support and six received placebo. Patients were similar for age, sex, weight, body mass index, HF etiology, co-morbidities, and medication for HF (Table 2). No patient was lost to follow-up and most tolerated the oral nutritional supplement. One patient withdrew consent after 1 week of intervention. Three patients died during the first 6 weeks (nutrition arm, 2; placebo arm, 1) and one patient on nutritional supplementation died after 14 weeks. Among the six subjects in the placebo group, we did not observe any significant effect on outcome measures. In patients receiving oral nutritional supplement, however, significant effects were observed which are reported below.
Edema-free body weight increased in 19 out of 20 patients receiving intervention at 6 weeks and in 17 out of 19 at 18 weeks. An average weight gain was 2.0 ± 1.7 kg (3.1 ± 2.4%) at 6 weeks (p = 0.0001) and 2.3 ± 3.1 kg (3.6 ± 4.7%) at 18 weeks (p = 0.007)—Fig. 2. According to DEXA scanning (Table 3), most of the weight gain was fat tissue. Absolute gain in fat tissue was 1.5 ± 1.7 kg (9.7 ± 12.7%) at 6 weeks (p = 0.003) and 1.6 ± 2.7 kg (10.0 ± 18.2%) at 18 weeks (p = 0.008) and was present in 16 out of 19 patients. Lean tissue mass also increased after 6 weeks (p = 0.019) but the effect was not maintained at 18 weeks.
Results of assessments for body weight (a), quality of life (b), TNFα (c), and total cholesterol (d) in patients with chronic HF and cachexia receiving nutritional support for 6 weeks and being assessed at baseline (N = 23), week 6 (N = 20) and week 18 (N = 19). Numbers and bars represent mean value ± SEM
Self-reported quality of life as measured by MLHFQ improved in all patients and the effect was preserved throughout the study (Fig. 2). A constant increase in distance walked in 6 min was observed (average increase of 61 m) whereas the peak VO2 during treadmill exercise testing and LVEF did not change significantly (Table 4). Patient subjective perception of HF as assessed by NYHA class was better in nine subjects with a significant overall effect: 2.8 ± 0.1 vs. 2.4 ± 0.1, p = 0.008. Compared to baseline, none of patients experienced worsening of NYHA class at any time point.
Oral nutritional supplement did not induce changes in serum sodium, uric acid, and albumin concentrations. There was a constant reduction of TNFα, soluble TNF-R1, and TNF-R2 levels throughout the study and the decrease was significant at 18 weeks when compared to baseline (Fig. 2 and Table 4). The serum lipoproteins total cholesterol and LDL cholesterol increased in 13 and 14 patients, respectively. From baseline to 18 weeks, a significant increase in serum lipoprotein concentration was observed (Fig. 2 and Table 4). Safety profile of oral nutritional supplement was comparable to placebo and no major clinical complications were recorded—Table 5.
4 Discussion
To our knowledge, this is the first interventional trial evaluating the effect of an oral nutritional supplement in cachectic patients with HF. The results of this pilot study suggest that 6 weeks of high-calorie high-protein nutritional support may have beneficial effects on dry body weight, body composition, and quality of life. We also demonstrated increases in serum lipoproteins and a reduction in serum TNFα levels.
Wasting in chronic disease states is on the rise and a strong predictor of poor outcomes including high mortality. Depending on the underlying disease and stage, 10–80% of patients with chronic diseases can develop cachexia [21]. Currently, no definitive remedy exists to correct this fatal condition [1]. Body wasting may be enhanced with inadequate food intake, thus an adequate diet should be a part of daily routine management of chronic conditions. It is therefore surprising that limited experience with simple measures as diet counseling and nutritional support in general and particularly in cardiac patients exists [19]. This may be due to well-established risk factors for development of clinically manifest cardiac disease which include increased body size and elevated serum total/LDL cholesterol that are partially driven by unhealthy diet, i.e., abundant intake of high fat and caloric food. Once chronic disease has developed, the risk factors seem not to be harmful anymore and previously pathological levels confer prognostic benefit. It has been suggested to term this phenomenon reverse epidemiology, and it occurrence extends beyond cardiac disease to fields of renal, pulmonary, musculoskeletal, and malignant disease [22]. Screening for body wasting was further hampered by lack of general definition for cachexia and difficulties to perceive reduction of body weight in obese or severely obese patients as grim prognostic sign. With recently accepted consensus definition of cachexia [23], particularly screening will be possible and we will be able to obtain more reliable epidemiological data. When such information will be at hand, design and conduction of trials to pinpoint questions of interest in cachectic chronic disease patients will be easier.
This study is the first to enter the arena of nutritional support in cachectic HF patients. Although only 600 additional kilocalories per day (20%–25% of recommended daily intake for individual patient) can seem trivial, a significant benefit in terms of body weight and inflammatory system was present. Even more important is the finding that such effect continued or at least persisted after termination of nutritional support and that patients experienced benefit in all measured outcomes. The mechanisms of cachexia are very complex and not entirely understood; therefore we cannot conclude much about mechanistic explanations of our results because this was beyond the study design. Nonetheless, some speculations could be derived in light of previous reports and when interpreting the results in a concise and intelligent manner.
An increase in body weight after only 6 weeks of additional 600 kcal/day in form of commercially available product is clinically very relevant, particularly when accounting for prior average 15 kg weight decrease from body weight when healthy. Weight stability or even weight gain for some are of utmost importance in patients with chronic disease. When body wasting or cachexia are present, a reversal of weight reduction may improve the patients’ prognosis. In this context, treatment with ACE inhibitors seems vital as they have been shown to prevent unintentional weight loss [10]. It is not entirely irrelevant, which body compartment is being wasted and which is being preserved. According to previous findings [1], it seems that lean body mass is associated with better quality of life whereas higher fat content is linked to better survival [24]. Indeed, DEXA scanning in our patients demonstrated clear increase of fat mass and content while lean mass did not change significantly. This in turn could then lead to less evident exercise capacity improvement but the patients were found to be in better clinical condition. Whether this translates into long-term prognostic benefit remains to be investigated.
The reasons of reduced inflammation as documented by decreases in TNFα and its soluble receptors cannot be clearly explained from our data. In general, the higher plasma lipids in our patients might have resulted from increased liver synthesis of lipoproteins, decreased catabolism or both. It was repeatedly shown in healthy humans that increased intake of fats raises plasma cholesterol level, but entirely no data exist as to plasma lipoprotein response to different fat intake in cardiac cachexia. We feel this could be caused by reduced lipoprotein catabolism which could be supported in several ways. Firstly, increased intake of fats could have been associated with enhanced buffering of endotoxins, and as recently demonstrated in healthy humans [25] could have decreased catabolism of lipoproteins. Secondly, oral nutritional supplement might have increased lipids excretion with the bile resulting again in more effective buffering of endotoxins. Thirdly, more frequent stimulation of digestive tract with additional meals could have activated the enteral nervous system to modulate local mucosal immunity toward better protection against bacteria or toxin translocation [26]. Unfortunately, we have not measured levels of endotoxins or any gastric hormones to support such hypothesis. Along with those changes in inflammatory markers, a constant increase of total and LDL cholesterol was observed. In patients with HF, higher total cholesterol is associated with better survival [27]; thus, our findings might bring additional clinical value for cachectic patients. Such response fits well the endotoxin–lipoprotein hypothesis [28] where lipoproteins reduce endotoxin burden through binding and neutralization. Hence, the trigger for inflammatory system is less pronounced and activation threshold is less often reached. In other words, our data suggest that oral nutritional supplement is safe in cardiac cachexia and nutritionally induced lipid changes might be implicated in favorable modification of inflammation. Same mechanisms may also have ancillary effects on patient performance [29] and other metabolic parameters [30, 31, 32].
4.1 Limitations
Our study with 29 patients has to be seen as a pilot trial in which we wanted to prove the concept as reported for other clinical conditions or situations. There, however, are some caveats to be considered. A relatively high albumin concentration at baseline is, in view of the advanced disease, likely caused by aggressive diuretic treatment. A 3:1 randomization was used to assure for an appropriate blinding and patient assessment during the study rather than for a direct comparison between intervention and placebo arm. With only six patients in the control group, only results in the intervention group could be interpreted as true effect beyond reasonable doubt of effect by chance. We did not follow the caloric and nutritional intake during the study. With commercially available product tested, which however is widely used as a nutritional support in clinical practice, no conclusions can be made about optimal dose and composition of nutritional support.
4.2 Clinical implications
This study demonstrated the feasibility of oral nutritional supplement use in cachectic HF patients and suggests that this may be a beneficial treatment approach in these patients. In clinical practice, a nutritional assessment to screen for malnourished or cachectic patients (or patients at risk) seems warranted. When such individuals are identified, a nutritional support may be appropriate (future studies need to confirm our results). Nutritional therapy likely is particularly relevant in the context of anabolic interventions, like physical exercise and specific anabolic drug therapy (e.g., with testosterone). It, however, remains unknown whether such strategies would confer particular benefits for some patient subgroups (e.g., those with enhanced inflammatory response) and whether response is dose dependent. Before a more general recommendation can be made, large-scale studies addressing the many open issues have to be performed.
References
von Haehling S, Lainscak M, Springer J, Anker SD. Cardiac cachexia: a systematic overview. Pharmacol Ther. 2009;121:227–52.
Rauchhaus M, Koloczek V, Volk HD, Kemp M, Niebauer J, Francis DP, et al. Inflammatory cytokines and the possible immunological role for lipoproteins in chronic heart failure. Int J Cardiol. 2000;76:125–33.
Anker SD, von Haehling S. Inflammatory mediators in chronic heart failure: an overview. Heart. 2004;90:464–70.
von Haehling S, Jankowska EA, Anker SD. Tumour necrosis factor-α and the failing heart: pathophysiology and therapeutic implications. Basic Res Cardiol. 2004;99:18–28.
Anker SD, Rauchhaus M. Insights into the pathogenesis of chronic heart failure: immune activation and cachexia. Curr Opin Cardiol. 1999;14:211–6.
Anker SD, Clark AL, Teixeira MM, Hellewell PG, Coats AJS. Loss of bone mineral in patients with cachexia due to chronic heart failure. Am J Cardiol. 1999;83:612–5.
Anker SD, Sharma R. The syndrome of cardiac cachexia. Int J Cardiol. 2002;85:51–66.
Anker SD, Ponikowski P, Varney S, Chua TP, Clark AL, Webb-Peploe KM, et al. Wasting as independent risk factor for mortality in chronic heart failure. Lancet. 1997;349:1050–3.
Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJ. More ’malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail. 2001;3:312–5.
Anker SD, Negassa A, Coats AJ, Afzal R, Poole-Wilson PA, Cohn JN, et al. Prognostic importance of weight loss in chronic heart failure and the effect of treatment with angiotensin-converting-enzyme inhibitors: an observational study. Lancet. 2003;361:1077–83.
Lainscak M, Keber I, Anker SD. Body composition changes in patients with systolic heart failure treated with beta blockers: a pilot study. Int J Cardiol. 2006;106:319–22.
Springer J, Filippatos G, Akashi YJ, Anker SD. Prognosis and therapy approaches of cardiac cachexia. Curr Opin Cardiol. 2006;21:229–33.
Kalantar-Zadeh K, Anker SD, Horwich TB, Fonarow GC. Nutritional and anti-inflammatory interventions in chronic heart failure. Am J Cardiol. 2008;101(11A):89E–103E.
Poehlman ET, Scheffers J, Gottlieb SS, Fisher ML, Vaitekevicius P. Increased resting metabolic rate in patients with congestive heart failure. Ann Intern Med. 1994;121:860–2.
Toth MJ, Gottlieb SS, Goran MI, et al. Daily energy expenditure in free-living heart failure patients. Am J Physiol. 1997;272:E469–75.
von Haehling S, Doehner W, Anker SD. Nutrition, metabolism, and the complex pathophysiology of cachexia in chronic heart failure. Cardiovasc Res. 2007;73:298–309.
Volkert D, Berner YN, Berry E, Cederholm T, Coti Bertrand P, Milne A, et al. ESPEN Guidelines on Enteral Nutrition: geriatrics. Clin Nutr. 2006;25:330–60.
Cano N, Fiaccadori E, Tesinsky P, Toigo G, Druml W, DGEM (German Society for Nutritional Medicine), et al. ESPEN Guidelines on Enteral Nutrition: adult renal failure. Clin Nutr. 2006;25:295–310.
Anker SD, John M, Pedersen PU, Raguso C, Cicoira M, Dardai E, et al. ESPEN Guidelines on Enteral Nutrition: cardiology and pulmonology. Clin Nutr. 2006;25:311–8.
Kalantar-Zadeh K, Braglia A, Chow J, Kwon O, Kuwae N, Colman S, et al. An anti-inflammatory and antioxidant nutritional supplement for hypoalbuminemic hemodialysis patients: a pilot/feasibility study. J Ren Nutr. 2005;15:318–31.
Morley JE, Thomas DR, Wilson MM. Cachexia: pathophysiology and clinical relevance. Am J Clin Nutr. 2006;83:735–43.
Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol. 2004;43:1439–44.
Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, et al. Cachexia: a new definition. Clin Nutr. 2008;27:793–9.
Cicoira MA, Doehner W, Jankowska WA, Zanolla L, Zardini P, Ponikowski P, et al. Body composition and prognosis in 511 chronic heart failure patients: results from three European centers. Eur J Heart Fail Suppl. 2004;3(Suppl):69.
Hudgins LC, Parker TS, Levine DM, Gordon BR, Saal SD, Jiang XC, et al. A single intravenous dose of endotoxin rapidly alters serum lipoproteins and lipid transfer proteins in normal volunteers. J Lipid Res. 2003;44:1489–98.
Genton L, Kudsk KA. Interaction between enteric nervous system and the immune system: role of neuropeptides and nutrition. Am J Surg. 2003;186:253–8.
Rauchhaus M, Clark AL, Doehner W, Davos C, Bolger A, Sharma R, et al. The relationship between cholesterol and survival in patients with chronic heart failure. J Am Coll Cardiol. 2003;42:1933–40.
Rauchhaus M, Coats AJS, Anker SD. The endotoxin-lipoprotein hypothesis. Lancet. 2000;356:930–3.
Anker SD, Volterrani M, Egerer KR, Felton CV, Kox WJ, Poole-Wilson PA, et al. Tumour necrosis factor alpha as a predictor of impaired peak leg blood flow in patients with chronic heart failure. QJM. 1998;91:199–203.
Leyva F, Anker SD, Egerer K, Stevenson JC, Kox WJ, Coats AJS. Hyperleptinaemia in chronic heart failure. Relationships with insulin. Eur Heart J. 1998;19:1547–51.
Anker SD, Leyva F, Poole-Wilson PA, Kox WJ, Stevenson JC, Coats AJS. Relation between serum uric acid and lower limb blood flow in patients with chronic heart failure. Heart. 1997;78:39–43.
Kovacic D, Marinsek M, Gobec L, Lainscak M, Podbregar M. Effect of selective and non-selective beta-blockers on body weight, insulin resistance and leptin concentration in chronic heart failure. Clin Res Cardiol. 2008;97:24–31.
von Haehling S, Morley JE, Coats AJS, Anker SD (2010) Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachexia Sarcopenia Muscle. doi:10.1007/s13539-010-0003-5
Acknowledgment
The authors of this manuscript certify that they comply with the Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle [33].
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Rozentryt, P., von Haehling, S., Lainscak, M. et al. The effects of a high-caloric protein-rich oral nutritional supplement in patients with chronic heart failure and cachexia on quality of life, body composition, and inflammation markers: a randomized, double-blind pilot study. J Cachexia Sarcopenia Muscle 1, 35–42 (2010). https://doi.org/10.1007/s13539-010-0008-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13539-010-0008-0