Abstract
Introduction
The BRCA1 protein makes mammary stem cells differentiate into mature luminal and myoepithelial cells. If a BRCA1 mutation results in a differentiation block, an enlarged stem cell component might be present in the benign tissue of BRCA1 mutation carriers, and these mammary stem cells could be the origin of BRCA1 related breast cancer. Since ALDH1 is a marker of both mammary stem cells and breast cancer stem cells, we compared ALDH1 expression in malignant tissue of BRCA1 mutation carriers to non-carriers.
Methods
Forty-one BRCA1 related breast cancers and 41 age-matched sporadic breast cancers were immunohistochemically stained for ALDH1. Expression in epithelium and stroma was scored and compared.
Results
Epithelial (P = 0.001) and peritumoral (P = 0.001) ALDH1 expression was significantly higher in invasive BRCA1 related carcinomas compared to sporadic carcinomas. Intratumoral stromal ALDH1 expression was similarly high in both groups. ALDH1 tumor cell expression was an independent predictor of BRCA1 mutation status.
Conclusion
BRCA1 related breast cancers showed significantly more frequent epithelial ALDH1 expression, indicating that these hereditary tumors have an enlarged cancer stem cell component. Besides, (peritumoral) stromal ALDH1 expression was also more frequent in BRCA1 mutation carriers. ALDH1 may therefore be a diagnostic marker and a therapeutic target of BRCA1 related breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Germline mutation carriers of the BRCA1 gene locus harbor a high cumulative risk of developing breast and ovarian cancer of 57% and 40% by age 70, respectively [1]. BRCA1 related breast cancer shows a distinct histopathological and immunohistochemical phenotype. It has been shown to be more often of the ductal or medullary types, of high grade and to show a high mitotic activity index (MAI) and necrosis [2–4]. These tumors usually do not express the estrogen (ER) and progesterone receptors (PR) and are almost always HER-2/neu negative (“triple negative”) [2, 3]. At the gene-expression level these tumors cluster together with the basal-like subgroup [5]. BRCA1 seems to play an important role in DNA repair in a common pathway with BRCA2 [6]. Increasing evidence indicates that BRCA1 is necessary for mammary stem cell differentiation, a function that could explain its tissue-specificity [7–10].
Stem cells play a role in repopulating the breast at several points in the human female lifespan. These primitive cells facilitate rapid expansion and regression in puberty and pregnancy, and during the menstrual cycle. In recent studies mammary stem cells have been isolated, by evaluation of specific characteristics like multipotency, the ability to undergo both symmetrical and asymmetrical divisions and being long-lived, slow cycling cells [11, 12].
A hierarchy of epithelial cells does not only seem to be present in the normal mammary gland, but in tumors as well. Al-Hajj et al. showed that only a small subpopulation of all cells in a tumor could be serially passaged, indicative of their tumor initiating capacity. These cells share many characteristics with stem cells, and are therefore denoted cancer stem cells (CSC) [13]. These CSCs could be important therapy targets, due to their tumor initiating capacity and being therapy resistant.
Several markers have been identified for the selection of human (cancer) stem cells, of which Aldehyde dehydrogenase 1 (ALDH1) is among the most widely studied ones. ALDH1 is a cytosolic detoxifying enzyme responsible for the oxidation of (retin)aldehydes into retinoids [14], which has been put forward as a marker of both normal human mammary stem cells and breast cancer stem cells. Human mammary cells selected for increased ALDH1 activity had the broadest lineage differentiation potential and highest growth capacity in a xenograft model, indicating that the ALDH1 positive cell population is enriched for mammary stem cells. Furthermore, it was shown that the ALDH1 positive population showed high tumorigenic capacity through serial passages, in contrast with the ALDH1 negative population [15]. The exact function of ALDH1 in (mammary) stem cells remains largely unknown, but it is thought to play a role in cellular differentiation, mainly through the retinoid signaling pathway [16].
As mentioned above, a novel function subscribed to BRCA1 is the regulation of mammary stem cell differentiation. An association between BRCA1 and stem cells was first suspected because of the basal phenotype of BRCA1 related tumors which resembles that of primitive mammary cells, implying that BRCA1 related tumors might originate in stem cells [17]. In vitro experiments have shown that ectopic overexpression of BRCA1 increases differentiation, whereas reduction of endogenous BRCA1 impairs differentiation [8]. Knockdown of BRCA1 in primary breast epithelial cells leads to accumulation of cells expressing ALDH1 and a decrease in ER positive cells expressing luminal epithelial markers. Furthermore, in the normal tissue of BRCA1 mutation carriers, clusters of ALDH1 positive cells have been described that were ER negative and showed loss of heterozygosity (LOH) of BRCA1. These results indicate that BRCA1 might indeed serve as a stem cell regulator in the mammary epithelium and that the stem cell pool in the normal tissue of BRCA1 mutation carriers might be enlarged [9], although our own results contradicted this [18]. If the origin of BRCA1 related cancer lies in this pool of stem cells, we would expect characteristics of this stem cell population like ALDH1 to be reflected in BRCA1 related breast cancers. In this study we therefore evaluated ALDH1 expression in invasive breast carcinomas of BRCA1 mutation carriers in comparison with cancers of non-carriers.
2 Methods
2.1 Study population
An invasive carcinoma group composed of 41 BRCA1 germline mutation carriers was age-matched with a control group, aiming at a maximum age difference of 5 years between case and control. We excluded all cases that mentioned a strong family history of breast cancer in the pathology report and all cases of which cumulative breast cancer risk exceeded 30% based on family history [19], but included patients that were referred to Clinical Genetics because of the young age of onset only and tested negative for BRCA1/2 mutations. This control group is further denoted “sporadic”. Anonymous use of redundant tissue for research purposes is part of the standard treatment agreement with patients in our hospitals [20]. Clinical data were retrieved from the pathology report and patient files. MAI was assessed as before [21]. Growth pattern was classified as expansive if pushing margins were observed in >50% of the tumor circumference, and otherwise as infiltrative [22].
2.2 Immunohistochemistry
Immunohistochemical analysis was carried out on 4-μm sections. All stainings were performed on full slides to avoid false negatives due to tumor heterogeneity. For all stainings, slides were deparaffinized in xylene and rehydrated in decreasing ethanol dilutions. Endogenous peroxidase activity was blocked with a buffer containing peroxide, followed by antigen retrieval. A cooling off period of 30 min preceded incubation with the primary antibody. Primary antibodies used, incubation time and the method of antigen retrieval are summarized in Table 1. In the case of EGFR we followed the protocol of the Pharm Dx kit. For all other antibodies, detection was done with a poly HRP anti Mouse/Rabbit/Rat IgG (ready to use; Powervision, Immunologic, Immunovision Technologies, Brisbane, California, USA). Peroxidase activity was developed with diaminobenzidin, except for ALDH1 for which we used Nova Red (Vector laboratories, Burlingame, USA). Slides were finally lightly counter-stained with hematoxylin and mounted. In between steps, slides were washed in PBS. Appropriate negative and positive controls were used throughout.
Staining for ER, PR, HER-2/neu, cytokeratin 5/6 (CK5/6) and epidermal growth factor receptor (EGFR) was performed to classify tumors into molecular subtypes as was described by Carey et al. This classification defines subtypes as follows: luminal A (ER+ and/or PR+ and HER2−), luminal B (ER+ and/or PR+ and HER2+), HER2 subtype (HER2+, ER− and PR−) and basal-like (ER−, PR−, HER2−, CK5/6+ and/or EGFR+). When a tumor was negative for all five markers it was denoted “unclassified” [23]. This sub-classification is used as the immunohistochemical surrogate of the subgroups detected by hierarchical clustering of gene-expression analysis of breast cancers [5].
2.3 Scoring of immunohistochemistry
Scoring was performed by two observers (MRHvV, PJvD) blinded to BRCA1 mutation status. For ER and PR the percentage of positive nuclei was estimated, and cases with >10% of stained cells were considered positive, according to the Dutch guidelines [24]. HER-2/neu was scored according to the DAKO system, considering only 3+ cases as positive. EGFR and CK5/6 were reported positive if clear membranous [25], respectively cytoplasmic staining [26] was seen.
Since no consensus exists for ALDH1 scoring, we scored both stromal and epithelial expression. Both intensity and percentage of intratumoral epithelial ALDH1 positive cells were evaluated in invasive carcinomas. Intensity was scored as 0 (absent), 1 (weak), 2 (moderate) or 3 (strong). H-scores reflecting the overall epithelial ALDH1 staining were calculated by multiplying the intensity score with the percentage of positive cells. A tumor was regarded positive if the H-score was 1 or above. The intensity of intratumoral stromal expression was scored from 0–4 as above in malignant tissues. The presence of peritumoral stromal overexpression was scored separately as present or absent.
2.4 Statistics
Discrete variables were compared by Chi-square test and Fisher’s exact test and odds ratios (OR) were calculated with 95% confidence intervals (95% CI). Normality of continuous data was tested by Kolomogorov-Smirnov test and groups were then compared by Students-T test or Mann-Whitney U test for normally distributed and non-parametric data, respectively.
In the case of comparisons between continuous and discrete variables, correlation coefficients were calculated. When features were associated (P < 0.10) with both BRCA1 mutation status and the presence of ALDH1 staining, bivariate statistical analysis of these possible confounders took place by calculating ORs stratified for specific subgroups (corrected by Mantel-Haenszel procedure). In addition, multivariate analysis by means of logistic regression for all significant features was performed. All statistical analyses were performed using SPSS 15.0.
3 Results
3.1 Baseline characteristics of the study cohort
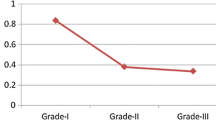
The baseline characteristics of the cohort of patients with invasive carcinomas are summarized in Table 2. Ductal carcinoma was the most prominent histological subtype accounting for 75.6% to 80.5% of tumors in the hereditary and sporadic groups, respectively. In the BRCA1 related group the frequency of medullary and metaplastic carcinomas was higher, whereas (ducto)lobular carcinoma were more frequent in the sporadic group. In the sporadic group tumors were most frequently of the luminal A type (73.2%). Basal-like subtype was only present in 19.5% of the non-carriers, in contrast with BRCA1 mutation carriers among whom basal-like subtype was the most prominent subtype (70.7%) (P < 0.0005; OR 9.97; 95% CI 3.58–27.80). In both groups tumors were most often of high grade, but grade 3 tumors were more frequent in BRCA1 related tumors (75.6%) compared to sporadic tumors (58.5%) (P = 0.10; OR 2.20; 95% CI 0.85–5.65). This is consistent with the median MAI, which was also significantly higher in the BRCA1 group (22.0) compared to the sporadic group (14) (P = 0.007). Median tumor size was slightly higher in the sporadic group (2.5 cm) compared to the group of mutation carriers (1.9 cm) (P = 0.04). A trend for more frequent negative nodal status was seen in the BRCA1 group (70.7%) compared to the sporadic group (46.9%)(P = 0.05). An expansive growth pattern was significantly more often present in BRCA1 related tumors (52.5%) compared to sporadic controls (23.7%) (P = 0.009). Further, BRCA1 related tumors were more frequently negative for HER-2/neu (n.s), ER (P < 0.0005) and PR (P < 0.0005).
3.2 ALDH1 expression in invasive carcinomas
ALDH1 expression in tumors showed wide variation, ranging from weak to very strong expression and from only a few positive cells, to a diffuse staining pattern in a high percentage of positive cells (Fig. 1). Similar to benign tissue, both stromal and epithelial cells expressed ALDH1[18]. Epithelial ALDH1 expression was distributed randomly over the tumor. However, for stromal expression a specific peritumoral staining pattern was seen in some cases. Data on epithelial and stromal expression are shown in Table 3.
Expression of ALDH in malignant breast tissues. Left: Breast cancer in a BRCA1 mutated patient showing strong peritumoral stromal (solid arrow) and frequent intratumoral epithelial expression (dashed arrow). Right: Sporadic breast cancer showing no peritumoral stromal and hardly intratumoral epithelial expression
Significantly more tumors showed epithelial ALDH1 expression in the BRCA1 group (78.0%) compared to sporadic breast cancer (41.5%) (P = 0.001). Both the intensity and the percentage of epithelial cells with ALDH1 expression were significantly higher in BRCA1 related breast cancer. In this group, 19.5% showed strong ALDH1 expression, compared to none of the sporadic tumors (P = 0.005). Overall, the median percentage of positive cells was 0.0 in the sporadic group compared to 2.0 in the hereditary group (P = 0.01), and in the cases with ALDH1 expression, the median percentage of positive cells was 10% in the sporadic group compared to 5% in the hereditary group (P = 0.27)
Stromal ALDH1 expression within the tumor was similarly high in both groups (strong expression in 43.9% of sporadic controls and 58.5% in hereditary cases; P = 0.14). However, the peritumoral stroma showed significantly more frequent overexpression in the BRCA1 related group (36.6%) compared to non-carriers (9.8%) (P = 0.001) (Fig. 1).
The presence of peritumoral and epithelial ALDH1 expression did not correlate with each other (P = 0.73; OR 1.21; 95% CI 0.42–3.47) and in multivariate analysis both were independent predictors of BRCA1 mutations status.
3.3 Correlation of ALDH1 with other characteristics
Epithelial ALDH1 expression in tumors correlated significantly with growth pattern (P = 0.02; OR 3.29; 95% CI 1.19–9.09) and younger age (P = 0.05; 95% CI 0.08–9.35). In addition, a trend for correlation with PR negativity (P = 0.06; OR 0.41; 95% CI 0.16–1.04), ER negativity (P = 0.08; OR 0.45; 95% CI 0.18–1.10), basal-like subtype (P = 0.08; OR 2.26; 95% CI 0.91–5.65) and larger tumor size (P = 0.08) was found. Intratumoral stromal ALDH1 expression did not correlate with other characteristics.
Peritumoral ALDH1 overexpression correlated with PR negativity (P = 0.002; OR 0.11; 95% CI 0.02–0.52), ER negativity (P = 0.001; OR 0.13; 95% CI 0.04–0.50), basal-like subtype (P = 0.004; OR 4.87; 95% CI 1.55–15.27) and high MAI (P = 0.009).
Since ER, PR, basal-like subtype and growth pattern were associated with both mutation status and the presence of epithelial ALDH1 expression, we performed stratified analysis for basal-like subtype and growth pattern, and estimated corrected ORs by Mantel-Haenszel procedure. The OR, adjusted for basal-like subtype, was still significant (ORadjusted 5.11; 95% CI 1.64–15.97; P = 0.005) and hardly differed from the crude OR (ORcrude 5.02). The estimated OR adjusted for growth pattern was slightly lower than the crude OR (ORadjusted 3.88; 95% CI 1.41–10.69; P = 0.009), but still significant. ER and PR were not independently analyzed as possible confounders, because they were constituents of basal-like subtype.
To correct for multiple confounders simultaneously, we performed multivariate analysis, by including ALDH1 expression, basal-like subtype and growth pattern in a stepwise logistic regression model. Hereby we estimated the independent predictive value of these factors for mutation status. In multivariate analysis only basal-like subtype (P < 0.0005) and the presence of epithelial ALDH1 expression (P = 0.005) were independent predictors of BRCA1 mutation status, whereas growth pattern was no longer of additional predictive value (P = 0.25).
Since PR, ER, basal-like subtype and MAI correlated significantly with both peritumoral ALDH1 expression and BRCA1 mutation status, we performed univariate and multivariate analysis to exclude confounders as above. The OR adjusted for basal-like phenotype was no longer significant (ORadjusted 2.65; 95% CI 0.77–9.04; P = 0.12), indicating that peritumoral ALDH1 expression and basal-like subtype are not of independent predictive value for BRCA1 mutation status. Because MAI was a continuous variable it was only included in multivariate analysis. In a logistic regression model only basal-like subclass (P < 0.0005), but not peritumoral ALDH1 expression (P = 0.08) and MAI (P = 0.55), was of independent predictive value for BRCA1 mutation status.
4 Discussion
This is the first study to evaluate ALDH1 expression in breast cancers of BRCA1 mutation carriers and to compare it to controls. We show that ALDH1 expression is significantly higher in the epithelium and in the peritumoral stroma in cancers of BRCA1 mutation carriers compared to sporadic controls.
Intratumoral epithelial ALDH1 expression was clearly more present in BRCA1 mutation carriers, implying that this population indeed has an enlarged CSC component. We find a somewhat higher frequency of epithelial expression in the group of sporadic invasive carcinomas (40%), as was described elsewhere (5–26%) [15, 27–29]. This might be explained by the fact that we used age-matching to select our sporadic controls. Hereby we possibly select a more aggressive population then we would get by randomly selecting breast cancers. This is also reflected by the high frequency of grade 3 carcinomas (58.5%) in our sporadic group. An additional problem, when comparing frequencies between studies, is that there is no consensus on the scoring method and the cut-off used for positivity. Most studies score both intensity and percentage of positive cells and use a cut off H >1, like we did, but higher thresholds (likely leading to lower frequencies) have also been applied.
In both our study and literature a correlation between intratumoral epithelial ALDH1 expression and basal-like subtype and ER- and PR-negative receptor status was found [15, 27]. We were unable to verify correlations between ALDH1 in tumors and grade, HER2 overexpressing subtype, CK5/6, CK14, [15] EGFR, p53, TOP2A [28], Ki67 [29] and MAI [30] that were previously described. This is probably due to the fact that we evaluated these characteristics only in a small population (e.g.CK5/6, EGFR) or not at all (e.g.CK14, p53, TOP2A). Furthermore, we found a significant correlation between ALDH1 expression in tumors and expansive growth pattern and younger age of onset.
There is no general consensus on the immunohistochemical definition of threshold for CK5/6 positivity to use. Korsching, E. et al, however, conclude that although a variability of thresholds was used in different studies on CK5/6 expression, they have very similar findings [31]. Therefore, the chosen threshold for CK5/6 positivity seems of little importance for the outcome of our current study.
Rates of strong intratumoral stromal ALDH1 expression were similar to literature [28] and significantly higher in BRCA1 carriers than controls, as was peritumoral stromal expression. Stromal ALDH1 expression is interesting because of its association with BRCA1 mutation status and outcome [28], but is not likely stem cell related, because expression was also found in over 80% of normal stroma tissue of non-carriers. The role of ALDH1 in fibroblasts remains largely unexplored. Our results imply that either BRCA1 is a regulator of stromal ALDH1 expression, or that stromal ALDH1 expression is a physiologic response to (very early) carcinogenetic events.
It is plausible that stromal and epithelial ALDH1 expression reflect different processes in carcinogenesis, since we could not find an association between epithelial and peritumoral stromal ALDH1 expression. This hypothesis is also supported by the seemingly contradictory previous reports on the relation between ALDH1 expression and prognosis. Epithelial ALDH1 expression has been associated with significantly decreased overall [15] and disease free survival, grade and systemic metastasis [32]. In addition, patients with an ALDH1 positive core needle biopsy had a significantly lower rate of pathologic complete response (pCR) after neo-adjuvant chemotherapy [33]. Contradictory with the association between epithelial ALDH1 expression and poor prognosis, intratumoral stromal ALDH1 expression correlated with good prognosis. [28] An explanation for the different effects of stromal and epithelial ALDH1 expression might be found in the biological role ALDH1 plays in processes apart from its potential role in stem cells and cellular differentiation. Both a tumor suppressing and an oncogenic role have been ascribed to retinoic acids (RA), the product of enzymatic conversion of vitamin A by ALDH1. In the presence of functional RA-receptor α (RARα), RA exhibits a growth inhibitory pro-apoptotic role, whereas RA was shown to promote cell growth and survival in the absence of functional RARα [34]. These findings indicate that RA can cause a diversity of effects, both pro- and anti-apoptotic in specific situations, for instance different cell types (e.g. stromal and epithelial cells). This diversity of working mechanisms is in line with the independent associations for stromal and epithelial staining, we find in this study and the contradictory associations with prognosis, found by others.
Apart from its pure biological interest, our finding that ALDH1 expression characterizes BRCA1 related breast cancer might serve several clinical purposes. ALDH1 could serve as a biomarker for BRCA1 mutation carriers. Easily assessable biomarkers are necessary to recognize hereditary cancers, because they can help to trigger analyzing family history and to decide on mutation testing in patients at borderline risk based on family history only. Tools that help to select patients for screening are needed, since genetic screening is time-consuming and expensive. Further, an established phenotype can help to pin down the pathogenicity of so called “unclassified variant” mutations. Since intratumoral ALDH1 expression was the only characteristic with additive predictive value independent of basal-like phenotype for BRCA1 mutation status, adding ALDH1 to a panel of IHC markers might significantly increase the predictive value of the model.
In addition, ALDH1 might be a possible therapeutic target in breast cancer. CSCs are considered relatively therapy resistant [35]. Several promising ways to target the ALDH1 CSC population have been identified. ALDH1 was first identified to be a marker of hematopoietic stem cells (HSCs). In CD34+CD38- HSCs it was shown that inhibiting ALDH1 signaling increased the stem cell population. This effect could be reversed by administration of exogenous all-trans-retinoic acid (ATRA), which is used on a therapeutic base in patients with acute promyelocytic leukemia (APML) [36]. ATRA stimulates differentiation into mature cells in these patients and treatment with ATRA in addition to chemotherapy significantly improves survival [37]. Its use in the treatment of other (solid) cancers has been limited to date, due to systemic toxicity and the development of resistance during carcinogenesis [38]. Recently it was shown that ALDH1 regulates the differentiation of breast CSC through retinoid signaling in a similar manner as in HSCs [16]. Further, blocking the IL-8 receptor CXCR1 with repertaxin has been shown to deplete the ALDH1 positive CSC population in vitro and to decrease the CSC population in human breast cancer xenografts, retarding tumor growth and reducing metastasis [39]. Both ATRA and repartaxin might enhance the effect of conventional chemotherapy by specifically targeting CSCs and sensitizing these relatively therapy resistant cells. This therapy might be of specific use in BRCA1 related breast cancer, since our results imply that these cancers have an increased ALDH1 positive CSC population.
In conclusion, compared to sporadic controls, ALDH1 positive (cancer stem) cells and peritumoral expression were significantly more frequent in BRCA1 related breast cancer. ALDH1 tumor cell expression was an independent predictor of BRCA1 mutation status. Thereby, ALDH1 might serve as a BRCA1 biomarker and therapeutic target.
References
S. Chen, G. Parmigiani, Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 25, 1329–1333 (2007)
E. Honrado, J. Benitez, J. Palacios, Histopathology of BRCA1- and BRCA2-associated breast cancer. Crit Rev Oncol Hematol 59, 27–39 (2006)
A.L. Bane, J.C. Beck, I. Bleiweiss, S.S. Buys, E. Catalano, M.B. Daly et al., BRCA2 mutation-associated breast cancers exhibit a distinguishing phenotype based on morphology and molecular profiles from tissue microarrays. Am J Surg Pathol 31, 121–128 (2007)
P. van der Groep, A. Bouter, R. van der Zanden, I. Siccama, F.H. Menko, J.J. Gille et al., Distinction between hereditary and sporadic breast cancer on the basis of clinicopathological data. J Clin Pathol 59, 611–617 (2006)
T. Sorlie, R. Tibshirani, J. Parker, T. Hastie, J.S. Marron, A. Nobel et al., Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 100, 8418–8423 (2003)
A.R. Venkitaraman, Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell 108, 171–182 (2002)
M. Kubista, M. Rosner, E. Kubista, G. Bernaschek, M. Hengstschlager, Brca1 regulates in vitro differentiation of mammary epithelial cells. Oncogene 21, 4747–4756 (2002)
S. Furuta, X. Jiang, B. Gu, E. Cheng, P.L. Chen, W.H. Lee, Depletion of BRCA1 impairs differentiation but enhances proliferation of mammary epithelial cells. Proc Natl Acad Sci USA 102, 9176–9181 (2005)
S. Liu, C. Ginestier, E. Charafe-Jauffret, H. Foco, C.G. Kleer, S.D. Merajver et al., BRCA1 regulates human mammary stem/progenitor cell fate. Proc Natl Acad Sci USA 105, 1680–1685 (2008)
E. Lim, F. Vaillant, D. Wu, N.C. Forrest, B. Pal, A.H. Hart et al., Aberrant luminal progenitors as the candidate target population for basal tumor development in BRCA1 mutation carriers. Nat Med 15, 907–913 (2009)
J. Stingl, A. Raouf, P. Eirew, C.J. Eaves, Deciphering the mammary epithelial cell hierarchy. Cell Cycle 5, 1519–1522 (2006)
M. Shackleton, F. Vaillant, K.J. Simpson, J. Stingl, G.K. Smyth, M.L. Asselin-Labat et al., Generation of a functional mammary gland from a single stem cell. Nature 439, 84–88 (2006)
M. Al-Hajj, M.S. Wicha, A. Benito-Hernandez, S.J. Morrison, M.F. Clarke, Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA 100, 3983–3988 (2003)
V. Vasiliou, A. Pappa, D.R. Petersen, Role of aldehyde dehydrogenases in endogenous and xenobiotic metabolism. Chem Biol Interact 129, 1–19 (2000)
C. Ginestier, M.H. Hur, E. Charafe-Jauffret, F. Monville, J. Dutcher, M. Brown et al., ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell 1, 555–567 (2007)
C. Ginestier, J. Wicinski, N. Cervera, F. Monville, P. Finetti, F. Bertucci et al., Retinoid signaling regulates breast cancer stem cell differentiation. Cell Cycle 8, 3297–3302 (2009)
W.D. Foulkes, BRCA1 functions as a breast stem cell regulator. J Med Genet 41, 1–5 (2004)
M.R. Heerma van Voss, P. Van der Groep, J. Bart, E. Van der Wall, P.J. Van Diest, Expression of the stem cell marker ALDH1 in the normal breast of BRCA1 mutation carriers. Br Cancer Res Treat 123, 611–612 (2010)
E.B. Claus, N. Risch, W.D. Thompson, Autosomal dominant inheritance of early-onset breast cancer, Implications for risk prediction. Cancer 73, 643–651 (1994)
P.J. van Diest, No consent should be needed for using leftover body material for scientific purposes. For. BMJ 325(7365), 648–51 (2002). Review
P.J. van Diest, J.P. Baak, P. Matze-Cok, E.C. Wisse-Brekelmans, C.M. van Galen, P.H. Kurver et al., Reproducibility of mitosis counting in 2, 469 breast cancer specimens: results from the Multicenter Morphometric Mammary Carcinoma Project. Hum Pathol 23, 603–607 (1992)
J.E. Armes, A.J. Egan, M.C. Southey, G.S. Dite, M.R. McCredie, G.G. Giles et al., The histologic phenotypes of breast carcinoma occurring before age 40 years in women with and without BRCA1 or BRCA2 germline mutations: a population-based study. Cancer 83, 2335–2345 (1998)
L.A. Carey, C.M. Perou, C.A. Livasy, L.G. Dressler, D. Cowan, K. Conway et al., Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295, 2492–2502 (2006)
Kwaliteitsinstituut voor de Gezondheidszorg CBO, Richtlijn mammacarcinoom, september 2008, http://www.cbo.nl/Downloads/328/rl_mamma_08.pdf, viewed 20/10/2010, 11:45 hr
P. Van der Groep, A. Bouter, R. Van der Zanden, F.H. Menko, H. Buerger, R.H.M. Verheijen, E. Van der Wall, P.J. Van Diest, Germline BRCA1 mutations and a basal epithelial phenotype in breast cancer. JNCI 96, 712–713 (2004)
P. Van der Groep, P.J. van Diest, F. Menko, J. Bart, E. de Vries, E. van der Wall, Molecular profile of ductal carcinoma in situ of the breast in BRCA1 and BRCA2 germline mutation carriers. J Clin Pathol 62, 926–930 (2009)
S.Y. Park, H.E. Lee, H. Li, M. Shipitsin, R. Gelman, K. Polyak, Heterogeneity for stem cell-related markers according to tumor subtype and histologic stage in breast cancer. Clin Cancer Res 16, 876–887 (2010)
E. Resetkova, J.S. Reis-Filho, R.K. Jain, R. Mehta, M.A. Thorat, H. Nakshatri, S. Badve, Prognostic impact of ALDH1 in breast cancer: a story of stem cells and tumor microenvironment, Breast Cancer Res Treat (2009), Epub ahead of print. Nov 13
K. Morimoto, S.J. Kim, T. Tanei, K. Shimazu, Y. Tanji, T. Taguchi et al., Stem cell marker aldehyde dehydrogenase 1-positive breast cancers are characterized by negative estrogen receptor, positive human epidermal growth factor receptor type 2, and high Ki67 expression. Cancer Sci 100, 1062–1068 (2009)
H. Nalwoga, J.B. Arnes, H. Wabinga, L.A. Akslen, Expression of aldehyde dehydrogenase 1 (ALDH1) is associated with basal-like markers and features of aggressive tumours in African breast cancer. Br J Cancer 102, 369–375 (2010)
E. Korsching et al., Basal carcinoma of the breast revisited: an old entity with new interpretations. J Clin Pathol 61, 553–560 (2008)
E. Charafe-Jauffret, C. Ginestier, F. Iovino, C. Tarpin, M. Diebel, B. Esterni, G. Houvenaeghel, J.M. Extra, F. Bertucci, J. Jacquemier, L. Xerri, G. Dontu, G. Stassi, Y. Xiao, S.H. Barsky, D. Birnbaum, P. Viens, M.S. Wicha, Aldehyde dehydrogenase 1-positive cancer stem cells mediate metastasis and poor clinical outcome in inflammatory breast cancer. Clin Cancer Res. 16(1), 45–55 (2010)
T. Tanei, K. Morimoto, K. Shimazu, S.J. Kim, Y. Tanji, T. Taguchi et al., Association of breast cancer stem cells identified by aldehyde dehydrogenase 1 expression with resistance to sequential Paclitaxel and epirubicin-based chemotherapy for breast cancers. Clin Cancer Res 15, 4234–4241 (2009)
G. Somenzi, G. Sala, S. Rossetti, M. Ren, R. Ghidoni, N. Sacchi, Disruption of retinoic acid receptor alpha reveals the growth promoter face of retinoic acid. PLoS One 2(9), e836 (2007)
T.M. Phillips, W.H. McBride, F. Pajonk, The response of CD24-/low/CD44+ breast cancer-initiating cells to radiation. J Natl Cancer Inst 98, 1777–1785 (2006)
J.P. Chute, G.G. Muramoto, J. Whitesides, M. Colvin, R. Safi, N.J. Chao et al., Inhibition of aldehyde dehydrogenase and retinoid signaling induces the expansion of human hematopoietic stem cells. Proc Natl Acad Sci USA 103, 11707–11712 (2006)
M.S. Tallman, J.W. Andersen, C.A. Schiffer, F.R. Appelbaum, J.H. Feusner, A. Ogden et al., All-trans-retinoic acid in acute promyelocytic leukemia. N Engl J Med 337, 1021–1028 (1997)
R.W. Glynn, N. Miller, M.J. Kerin, 17q12-21—The pursuit of targeted therapy in breast cancer. Cancer Treat Rev. 36(3), 224–9 (2010)
C. Ginestier, S. Liu, M.E. Diebel, H. Korkaya, M. Luo, M. Brown et al., CXCR1 blockade selectively targets human breast cancer stem cells in vitro and in xenografts. J Clin Invest 120(2), 485–97 (2010)
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Heerma van Voss, M.R., van der Groep, P., Bart, J. et al. Expression of the stem cell marker ALDH1 in BRCA1 related breast cancer. Cellular Onc. 34, 3–10 (2011). https://doi.org/10.1007/s13402-010-0007-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-010-0007-3