Abstract
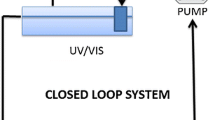
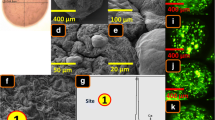
In recent studies, we designed multi-compartmental microcapsules as a platform for the targeted oral delivery of lipophilic drugs in an animal model of type 2 diabetes (T2D). Probucol (PB) is a highly lipophilic, antihyperlipidemic drug with potential antidiabetic effects. PB has low bioavailability and high inter-individual variations in absorption, which limits its clinical applications. In a new study, the bile acid, taurocholic acid (TCA), exerted permeation enhancing effects in vivo. Accordingly, this study aimed to design and characterize TCA-based PB microcapsules and examine the effects of TCA on the microcapsules’ morphology, stability, and release profiles. Microcapsules were prepared using the polymer sodium alginate (SA). Two types of microcapsules were produced, one without TCA (PB-SA, control) and one with TCA (PB-TCA-SA, test). Microcapsules were studied in terms of morphology, surface structure and composition, size, drug contents, cross-sectional imaging (using microtomography (Micro-CT) analysis), Zeta potential, thermal and chemical profiles, rheological parameters, swelling, mechanical strength, and release studies at various temperature and pH values. The production yield and the encapsulation efficiency were also studied together with in vitro efficacy testing of cell viability at various glucose concentrations and insulin and TNF-α production using clonal-mouse pancreatic β-cells. PB-TCA-SA microcapsules showed uniform structure and even distribution of TCA within the microcapsules. Drug contents, Zeta potential, size, rheological parameters, production yield, and the microencapsulation efficiency remained similar after TCA addition. In vitro testing showed PB-TCA-SA microcapsules improved β-cell survival under hyperglycemic states and reduced the pro-inflammatory cytokine TNF-α while increasing insulin secretions compared with PB-SA microcapsules. PB-TCA-SA microcapsules also showed good stability, better mechanical (p < 0.01) and swelling (p < 0.01) characteristics, and optimized controlled release at pH 7.8 (p < 0.01) compared with control, suggesting desirable targeted release properties and potential applications in the oral delivery of PB in T2D.







Similar content being viewed by others
References
Al-Salami H, Kansara H, King J, Morar B, Jayathilaka B, Fawcett PJ, et al. Bile acids: a bitter sweet remedy for diabetes. N Z Pharm J. 2007;27(10):17–20.
Calasan J, Al-Salami H, Mikov M. Bile acids and probiotics could help treating diabetes. Febs Journal. 2012;279:267.
Negrulj R, Mooranian A, Al-Salami H. Potentials and limitations of bile acids in type 2 diabetes mellitus: applications of microencapsulation as a novel oral delivery system. J Endocrinol Diabetes Mellitus. 2013;1(2):49–59.
Berger E, Haller D. Structure-function analysis of the tertiary bile acid TUDCA for the resolution of endoplasmic reticulum stress in intestinal epithelial cells. Biochem Biophys Res Commun. 2011;409(4):610–5.
Beilke LD, Aleksunes LM, Holland RD, Besselsen DG, Beger RD, Klaassen CD, et al. Constitutive androstane receptor-mediated changes in bile acid composition contributes to hepatoprotection from lithocholic acid-induced liver injury in mice. Drug Metab Dispos Biol Fate Chem. 2009;37(5):1035–45.
Sievanen E. Exploitation of bile acid transport systems in prodrug design. Molecules. 2007;12(8):1859–89.
Mikov M, Boni NS, Al-Salami H, Kuhajda K, Kevresan S, Fawcett JP. Pharmacokinetics and hypoglycaemic effect of 3 alpha, 7 alpha-dihydroxy-12-oxo-5beta-cholanate (MKC) in diabetic rat. Febs J. 2006;273:210.
Mikov M, Boni NS, Al-Salami H, Kuhajda K, Kevresan S, Golocorbin-Kon S, et al. Bioavailability and hypoglycemic activity of the semisynthetic bile acid salt, sodium 3alpha,7alpha-dihydroxy-12-oxo-5beta-cholanate, in healthy and diabetic rats. Eur J Drug Metab Pharmacokinet. 2007;32(1):7–12.
Al-Salami H, Butt G, Fawcett JP, Tucker IG, Golocorbin-Kon S, Mikov M. Probiotic treatment reduces blood glucose levels and increases systemic absorption of gliclazide in diabetic rats. Eur J Drug Metab Pharmacokinet. 2008;33(2):101–6.
Mikov M, Al-Salami H, Golocorbin-Kon S, Skrbic R, Raskovic A, Fawcett JP. The influence of 3alpha,7alpha-dihydroxy-12-keto-5beta-cholanate on gliclazide pharmacokinetics and glucose levels in a rat model of diabetes. Eur J Drug Metab Pharmacokinet. 2008;33(3):137–42.
Al-Salami H, Butt G, Tucker I, Golocorbin-Kon S, Mikov M. Probiotics decreased the bioavailability of the bile acid analog, monoketocholic acid, when coadministered with gliclazide, in healthy but not diabetic rats. Eur J Drug Metab Pharmacokinet. 2012;37(2):99–108.
Mikov M A-SH, Golocorbin-Kon G. Potentials and limitations of bile acids and probiotics in diabetes mellitus. 2012;365–402.
Al-Salami H, Butt G, Tucker I, Mikov M. Influence of the semisynthetic bile acid MKC on the ileal permeation of gliclazide in vitro in healthy and diabetic rats treated with probiotics. Methods Find Exp Clin Pharmacol. 2008;30(2):107–13.
Al-Salami H, Butt G, Tucker I, Skrbic R, Golocorbin-Kon S, Mikov M. Probiotic pre-treatment reduces gliclazide permeation (ex vivo) in healthy rats but increases it in diabetic rats to the level seen in untreated healthy rats. Arch Drug Inf. 2008;1(1):35–41.
Al-Salami H, Butt G, Tucker IG, Mikov M. The influence of pre-treatment with probiotics on the in vitro ileal permeation of the antidiabetic drug gliclazide, in healthy and diabetic rats. Drug Metab Rev. 2008;40:81–2.
Al-Salami H, Grant B, Ian T, Mikov M. The influence of probiotics pre-treatment, on the ileal permeation of gliclazide, in healthy and diabetic rats. Arch Drug Inf. 2008;1(1):35–41.
Al-Salami H, Butt G, Tucker I, Fawcett PJ, Golocorbin-Kon S, Mikov I, et al. Gliclazide reduces MKC intestinal transport in healthy but not diabetic rats. Eur J Drug Metab Pharmacokinet. 2009;34(1):43–50.
Mooranian A, Negrulj R, Chen-Tan N, Al-Sallami HS, Fang Z, Mukkur T, et al. Microencapsulation as a novel delivery method for the potential antidiabetic drug, Probucol. Drug Des Dev Ther. 2014;8:1221–30.
Mooranian A, Negrulj R, Chen-Tan N, Al-Sallami HS, Fang Z, Mukkur T, et al. Novel artificial cell microencapsulation of a complex gliclazide-deoxycholic bile acid formulation: a characterization study. Drug Des Dev Ther. 2014;8:1003.
Mooranian A, Negrulj R, Al-Sallami HS, Fang Z, Mikov M, Golocorbin-Kon S, et al. Probucol release from novel multicompartmental microcapsules for the oral targeted delivery in type 2 diabetes. AAPS PharmSciTech. 2014;16(1):45–52.
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. Characterization of a novel bile acid-based delivery platform for microencapsulated pancreatic β-cells. Art Cells Nanomed Biotechnol. 2014;11:1–7.
Mooranian A, Negrulj R, Mathavan S, Martinez J, Sciarretta J, Chen-Tan N, et al. An advanced microencapsulated system: a platform for optimized oral delivery of antidiabetic drug-bile acid formulations. Pharm Dev Technol. 2014;1–8.
Mooranian A, Negrulj R, Mathavan S, Martinez J, Sciarretta J, Chen-Tan N, et al. Stability and release kinetics of an advanced gliclazide-cholic acid formulation: the use of artificial-cell microencapsulation in slow release targeted oral delivery of antidiabetics. J Pharm Innov. 2014;9(2):150–157.
Park K, Ki Lee S, Hyun Son D, Ah Park S, Kim K, Won Chang H, et al. The attenuation of experimental lung metastasis by a bile acid acylated-heparin derivative. Biomaterials. 2007;28(16):2667–76.
Eom JS, Koh KS, Al-Hilal TA, Park JW, Jeon OC, Moon HT, et al. Antithrombotic efficacy of an oral low molecular weight heparin conjugated with deoxycholic asset on microsurgical anastomosis in rats. Thromb Res. 2010;126(3):e220–4.
Fakhoury M, Negrulj R, Mooranian A, Al-Salami H. Inflammatory bowel disease: clinical aspects and treatments. J Inflamm Res. 2014;7:113–20.
Mooranian A, Negrulj R, Mikov M, Golocorbin-Kon S, Arfuso F, Al-Salami H. Novel chenodeoxycholic acid-sodium alginate matrix in the microencapsulation of the potential antidiabetic drug, probucol. An in vitro study. J Microencapsul. 2015:1–9.
Lee E, Kim Y-S, Bae SM, Kim SK, Jin S, Chung SW, et al. Polyproline-type helical-structured low-molecular weight heparin (LMWH)-taurocholate conjugate as a new angiogenesis inhibitor. Int J Cancer. 2009;124(12):2755–65.
Khatun Z, Nurunnabi M, Reeck GR, Cho KJ, Lee YK. Oral delivery of taurocholic acid linked heparin-docetaxel conjugates for cancer therapy. J Control Release Off J Control Release Soc. 2013;170(1):74–82.
Negrulj R, Mooranian A, Chen-Tan N, Al-Sallami HS, Mikov M, Golocorbin-Kon S, et al. Swelling, mechanical strength, and release properties of probucol microcapsules with and without a bile acid, and their potential oral delivery in diabetes. Artif Cells Nanomed Biotechnol. 2015;26:1–8.
Shimizu H, Uehara Y, Shimomura Y, Tanaka Y, Kobayashi I. Probucol attenuated hyperglycemia in multiple low-dose streptozotocin-induced diabetic mice. Life Sci. 1991;49(18):1331–8.
Wu R, Zhang W, Liu B, Gao J, Xiao X-Q, Zhang F, et al. Probucol ameliorates the development of nonalcoholic steatohepatitis in rats fed high-fat diets. Dig Dis Sci. 2013;58(1):163–71.
Yamashita S, Matsuzawa Y. Where are we with probucol: a new life for an old drug? Atherosclerosis. 2009;207(1):16–23.
Chang TM. Pharmaceutical and therapeutic applications of artificial cells including microencapsulation. Eur J Pharm Biopharm Off J Arbeitsgemeinschaft Pharm Verfahrenstechnik eV. 1998;45(1):3–8.
Hamaguchi K, Gaskins HR, Leiter EH. NIT-1, a pancreatic beta-cell line established from a transgenic NOD/Lt mouse. Diabetes. 1991;40(7):842–9.
Al-Salami H, Butt G, Tucker I, Mikov M. Influence of the semisynthetic bile acid (MKC) on the ileal permeation of gliclazide in healthy and diabetic rats. Methods Find Exp Clin Pharmacol. 2008;30(2):107–13.
Mooranian A, Negrulj R, Chen-Tan N, Fakhoury M, Arfuso F, Jones F, et al. Advanced bile acid-based multi-compartmental microencapsulated pancreatic beta-cells integrating a polyelectrolyte-bile acid formulation, for diabetes treatment. Art Cells Nanomed Biotechnol. 2014;1–8.
Mooranian A, Negrulj R, Chen-Tan N, Watts GF, Arfuso F, Al-Salami H. An optimized probucol microencapsulated formulation integrating a secondary bile acid (deoxycholic acid) as a permeation enhancer. Drug Des Dev Ther. 2014;8:1673–83.
Mooranian A, Negrulj R, Al-Sallami HS, Fang Z, Mikov M, Golocorbin-Kon S, et al. Release and swelling studies of an innovative antidiabetic-bile acid microencapsulated formulation, as a novel targeted therapy for diabetes treatment. J Microencapsul. 2015;1-8.
Huang X, Brazel CS. On the importance and mechanisms of burst release in matrix-controlled drug delivery systems. J Control Release. 2001;73(2):121-36.
Altaf M. Ionic gelation controlled drug delivery systems for gastric-mucoadhesive microcapsules of captopril. Indian J Pharm Sci. 2008;70(5):655.
Xie HG, Li XX, Lv GJ, Xie WY, Zhu J, Luxbacher T, et al. Effect of surface wettability and charge on protein adsorption onto implantable alginate‐chitosan‐alginate microcapsule surfaces. J Biomed Mater Res A. 2010;92(4):1357–65.
Ajun W, Yan S, Li G, Huili L. Preparation of aspirin and probucol in combination loaded chitosan nanoparticles and in vitro release study. Carbohydr Polym. 2009;75(4):566–74.
Thybo P, Pedersen BL, Hovgaard L, Holm R, Müllertz A. Characterization and physical stability of spray dried solid dispersions of probucol and PVP-K30*. Pharm Dev Technol. 2008;13(5):375–86.
Batta AK, Aggarwal SK, Salen G, Shefer S. Selective reduction of oxo bile acids: synthesis of 3 beta-, 7 beta-, and 12 beta-hydroxy bile acids. J Lipid Res. 1991;32(6):977–83.
Soares J, Santos J, Chierice G, Cavalheiro E. Thermal behavior of alginic acid and its sodium salt. Eclética Quím. 2004;29(2):57–64.
Takka S, Cali AG. Bile salt-reinforced alginate-chitosan beads. Pharm Dev Technol. 2012;17(1):23–9.
Yang Y, Campanella OH, Hamaker BR, Zhang G, Gu Z. Rheological investigation of alginate chain interactions induced by concentrating calcium cations. Food Hydrocoll. 2013;30(1):26–32.
Bonino CA, Samorezov JE, Jeon O, Alsberg E, Khan SA. Real-time in situ rheology of alginate hydrogel photocrosslinking. Soft Matter. 2011;7(24):11510–7.
Pamies R, Schmidt RR, Martínez MDCL, Torre JGDL. The influence of mono and divalent cations on dilute and non-dilute aqueous solutions of sodium alginates. Carbohydr Polym. 2010;80(1):248–53.
Legrand J, Dumont E, Comiti J, Fayolle F. Diffusion coefficients of ferricyanide ions in polymeric solutions—comparison of different experimental methods. Electrochim Acta. 2000;45(11):1791–803.
Lalic-Popovic M, Vasovic V, Milijasevic B, Golocorbin-Kon S, Al-Salami H, Mikov M. Deoxycholic acid as a modifier of the permeation of gliclazide through the blood brain barrier of a rat. J Diabetes Res. 2013;2013:598603.
Wu T, Bound MJ, Standfield SD, Gedulin B, Jones KL, Horowitz M, et al. Effects of rectal administration of taurocholic acid on glucagon-like peptide-1 and peptide YY secretion in healthy humans. Diabetes Obes Metab. 2013;15(5):474–7.
Adrian TE, Gariballa S, Parekh KA, Thomas SA, Saadi H, Al Kaabi J, et al. Rectal taurocholate increases L cell and insulin secretion, and decreases blood glucose and food intake in obese type 2 diabetic volunteers. Diabetologia. 2012;55(9):2343–7.
Wu T, Bound MJ, Standfield SD, Jones KL, Horowitz M, Rayner CK. Effects of taurocholic acid on glycemic, glucagon-like peptide-1, and insulin responses to small intestinal glucose infusion in healthy humans. J Clin Endocrinol Metab. 2013;98(4):E718–22.
Fukuda M, Ikegami H, Kawaguchi Y, Sano T, Ogihara T. Antioxidant, probucol, can inhibit the generation of hydrogen peroxide in islet cells induced by macrophages and prevent islet cell destruction in NOD mice. Biochem Biophys Res Commun. 1995;209(3):953–8.
Gorogawa S, Kajimoto Y, Umayahara Y, Kaneto H, Watada H, Kuroda A, et al. Probucol preserves pancreatic beta-cell function through reduction of oxidative stress in type 2 diabetes. Diabetes Res Clin Pract. 2002;57(1):1–10.
Liu JH, Liu DF, Wang NN, Lin HL, Mei X. Possible role for the thioredoxin system in the protective effects of probucol in the pancreatic islets of diabetic rats. Clin Exp Pharmacol Physiol. 2011;38(8):528–33.
Düfer M, Hörth K, Wagner R, Schittenhelm B, Prowald S, Wagner TF, et al. Bile acids acutely stimulate insulin secretion of mouse β-cells via farnesoid X receptor activation and KATP channel inhibition. Diabetes. 2012;61(6):1479–89.
Renga B, Mencarelli A, Vavassori P, Brancaleone V, Fiorucci S. The bile acid sensor FXR regulates insulin transcription and secretion. Biochim Biophys Acta (BBA) - Mol Basis Dis. 2010;1802(3):363–72.
Thomas C, Gioiello A, Noriega L, Strehle A, Oury J, Rizzo G, et al. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 2009;10(3):167–77.
Prawitt J, Caron S, Staels B. Bile acid metabolism and the pathogenesis of type 2 diabetes. Curr Diab Rep. 2011;11(3):160–6.
Houten SM, Watanabe M, Auwerx J. Endocrine functions of bile acids. EMBO J. 2006;25(7):1419–25.
Perez MJ, Briz O. Bile-acid-induced cell injury and protection. World J Gastroenterol WJG. 2009;15(14):1677–89.
Acknowledgments
The authors acknowledge the Australian Postgraduate Award (APA) + Curtin Research Scholarship (CRS) for their support. The authors also acknowledge the CHIRI and the use of laboratory equipment and the scientific and technical assistance of Curtin University Electron Microscope Facility, which has been partially funded by the University, State, and Commonwealth Governments. The authors also acknowledge the Pharmaceutical Technology Laboratory (Curtin School of Pharmacy). The authors are grateful to the Harry Perkins Institute of Medical Research, Centre for Medical Research, University of Western Australia and St. Vincent’s Institute of Medical Research (Victoria) for supplying the NIT-1 β-cells.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mooranian, A., Negrulj, R., Arfuso, F. et al. The effect of a tertiary bile acid, taurocholic acid, on the morphology and physical characteristics of microencapsulated probucol: potential applications in diabetes: a characterization study. Drug Deliv. and Transl. Res. 5, 511–522 (2015). https://doi.org/10.1007/s13346-015-0248-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-015-0248-9