Abstract
Context
Abdominal obesity (AO) is a definitive link between cardiometabolic complications and metabolic syndrome (MetS). Many traditional and novel anthropometric indices have been identified to determine AO, and their relationship to MetS has been investigated. However, whether these indices are useful in a clinical setting is unknown. Moreover, the cut-off points for these indices to determine MetS have yet to be defined among Southern-Indian adults.
Aims
We aimed to evaluate the cut-off values and clinical efficacy of novel anthropometric indices in identifying MetS and its components.
Materials and methods
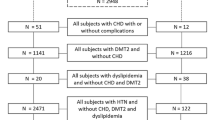
Subjects (n = 202) were recruited and then grouped into cases (MetS = 106) and controls (healthy = 96). We measured anthropometric data and assayed glycemic and lipid profiles. Using these, we computed a-body shape index (ABSI), abdominal volume index (AVI), body adiposity index (BAI), body roundness index (BRI), conicity index (CI), lipid-accumulation product (LAP), visceral adiposity index (VAI) and waist-triglyceride index (WTI) from published equations.
Results
Compared to the control group, all the novel anthropometric indices were noticeably higher in both male and female subjects of the MetS group. The area under the curve values (AUCs) demonstrated that BRI, CI, AVI, and WTI had superior detection power in identifying MetS, and the AUCs varied upon stratification by gender. BRI was strongly associated with the highest odds of having MetS (OR 66.03).
Conclusions
The optimal cut-off and AUC values attained for BRI, CI, AVI, and WTI have a clinical approach in identifying MetS and its components. The efficacy of these indices to identify MetS differed by gender.
Similar content being viewed by others
References
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74(10):e177-232.
Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005;28(7):1769–78.
Eckel RH, Alberti KG, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2010;375(9710):181–3.
Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol. 2008;28(4):629–36.
Zafar U, Khaliq S, Ahmad HU, Manzoor S, Lone KP. Metabolic syndrome: an update on diagnostic criteria, pathogenesis, and genetic links. Hormones. 2018;17(3):299–313.
Moreira GC, Cipullo JP, Ciorlia LA, Cesarino CB, Vilela-Martin JF. Prevalence of metabolic syndrome: association with risk factors and cardiovascular complications in an urban population. PLoS One. 2014. https://doi.org/10.1371/journal.pone.0105056.
Saklayen MG. The global epidemic of metabolic syndrome. Curr Hypertens Rep. 2018;20:12.
Bhowmik B, Afsana F, Siddiquee T, Munir SB, Sheikh F, Wright E, et al. Comparison of the prevalence of metabolic syndrome and its association with diabetes and cardiovascular disease in the rural population of Bangladesh using the modified National Cholesterol Education Program Expert Panel Adult Treatment Panel III and International Diabetes Federation definitions. J Diabetes Investig. 2015;6(3):280–8.
Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATP III and IDF definitions in Asian Indians: the Chennai Urban Rural Epidemiology Study (CURES-34). Diabetes Metab Res Rev. 2007;23(2):127–34.
Prasad DS, Kabir Z, Dash AK, Das BC. Prevalence and risk factors for metabolic syndrome in Asian Indians: a community study from urban Eastern India. J Cardiovasc Dis Res. 2012;3(3):204.
Venugopal V, Dongre AR, Saravanan S. Prevalence and determinants of metabolic syndrome among the rural adult population of Puducherry. Indian J Community Med. 2019;44(1):21–5. https://doi.org/10.4103/ijcm.IJCM_132_18.
Shin J-A, Lee J-H, Lim S-Y, Ha H-S, Kwon H-S, Park Y-M, et al. Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. J Diabetes Investig. 2013;4(4):334–43.
Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28(6):1039–49.
Cai L, Lubitz J, Flegal KM, Pamuk ER. The predicted effects of chronic obesity in middle age on medicare costs and mortality. Med Care. 2010;1:510–7.
World Health Organization. Obesity: preventing and managing the global epidemic. World Health Org Tech Rep Ser. 2000;894:1–253.
Kang SM, Yoon JW, Ahn HY, Kim SY, Lee KH, Shin H, Choi SH, Park KS, Jang HC, Lim S. Android fat depot is more closely associated with metabolic syndrome than abdominal visceral fat in elderly people. PLoS One. 2011. https://doi.org/10.1371/journal.pone.0027694.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13:275–86.
Ma CM, Lu N, Wang R, Liu XL, Lu Q, Yin FZ. Three novel obese indicators perform better in monitoring the management of metabolic syndrome in type 2 diabetes. Sci Rep. 2017;7:9843.
Costa EC, Sa JC, Soares EM, Lemos TM, Maranhao TM, Azevedo GD. Anthropometric indices of central obesity how discriminators of metabolic syndrome in Brazilian women with polycystic ovary syndrome. Gynecol Endocrinol. 2012;28:12–5.
Motamed N, Sohrabi M, Poustchi H, Maadi M, Malek M, Keyvani H, et al. The six obesity indices, which one is more compatible with metabolic syndrome? A population-based study. Diabetes Metab Syndr. 2017;11(3):173–7.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity. 2013;21(11):2264–71.
Liu B, Liu B, Wu G, Yin F. Relationship between body-roundness index and metabolic syndrome in type 2 diabetes. Diabetes Metab Syndr Obes Targets Ther. 2019;12:931–5.
WHO. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452.
Fukuyama N, Homma K, Wakana N, Kudo K, Suyama A, Ohazama H, Tsuji C, Ishiwata K, Eguchi Y, Nakazawa H, Tanaka E. Validation of the friedewald equation for evaluation of plasma LDL-cholesterol. J Clin Biochem Nutr. 2008;43(1):1–5.
Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33(4):920–2.
Kahn HS. The lipid accumulation product is better than BMI for identifying diabetes: a population-based comparison. Diabetes Care. 2006;29(1):151–3.
Yang RF, Liu XY, Lin Z, Zhang G. Correlation study on waist circumference-triglyceride (WT) index and coronary artery scores in patients with coronary heart disease. Eur Rev Med Pharmacol Sci. 2015;19(1):113–8.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One. 2012;7(7):e39504.
Guerrero-Romero F, Rodrı́guez-Morán F. Abdominal volume index. An anthropometry-based index for the estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch Med Res. 2003;34(5):428–32.
Farzad S, Fatemeh A, Salehi M, Nojomi M. Association of waist circumference, body mass index and conicity index with cardiovascular risk factors in postmenopausal women. Cardiovasc J Afr. 2012;23(8):442.
Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, Xiang AH, Watanabe RM. A better index of body adiposity. Obesity. 2011;19(5):1083–9.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a non-parametric approach. Biometrics. 1988;1:837–45.
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden Index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J. 2008;50(3):419–30.
Krakauer NY, Krakauer JC. Dynamic association of mortality hazard with body shape. PLoS One. 2014. https://doi.org/10.1371/journal.pone.0088793.
Maessen MF, Eijsvogels TM, Verheggen RJ, Hopman MT, Verbeek AL, de Vegt F. Entering a new era of body indices: the feasibility of a body shape index and body roundness index to identify cardiovascular health status. PLoS One. 2014. https://doi.org/10.1371/journal.pone.0107212.
Wang H, Liu A, Zhao T, Gong X, Pang T, Zhou Y, Xiao Y, Yan Y, Fan C, Teng W, Lai Y. Comparison of anthropometric indices for predicting the risk of metabolic syndrome and its components in Chinese adults: a prospective, longitudinal study. BMJ Open. 2017. https://doi.org/10.1136/bmjopen-2017-016062.
López AA, Cespedes ML, Vicente T, Tomas M, Bennasar-Veny M, Tauler P, Aguilo A. Body adiposity index utilization in a Spanish Mediterranean population: comparison with the body mass index. PLoS One. 2012;7(4):e35281.
Shin KA, Hong SB, Shin KS. Body adiposity index and metabolic syndrome risk factors in Korean adults: a comparison with bodymass index and other parameters. Biomed Sci Lett. 2017;23:57–63.
Kahn HS. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord. 2005;5(1):26.
Mirmiran P, Bahadoran Z, Azizi F. Lipid accumulation product is associated with insulin resistance, lipid peroxidation, and systemic inflammation in type 2 diabetic patients. Endocrinol Metab. 2014;29(4):443–9.
Amato MC, Giordano C, Galia M, et al. Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33(4):920–2.
Wang Y, He S, He J, Wang S, Liu K, Chen X. Predictive value of visceral adiposity index for type 2 diabetes mellitus. Herz. 2015;40(3):277–81.
Chen HY, Chiu YL, Chuang YF, Hsu SP, Pai MF, Yang JY, Peng YS. Visceral adiposity index and risks of cardiovascular events and mortality in prevalent hemodialysis patients. Cardiovasc Diabetol. 2014;13(1):136.
Bermúdez VJ, Salazar J, Añez R, Rivas-Ríos JR, Chávez-Castillo M, Torres W, Núñez V, Mejías J, Wilches-Durán S, Cerda M, Graterol M. Optimal cut-off for visceral adiposity index in a Venezuelan population: results from the Maracaibo City Metabolic Syndrome Prevalence Study. Rev Argent Endocrinol Metab. 2017;54(4):176–83.
Borruel S, Molto JF, Alpanes M, Fernandez-Duran E, Alvarez-Blasco F, Luque-Ramirez M, Escobar-Morreale HF. Surrogate markers of visceral adiposity in young adults: waist circumference and body mass index are more accurate than waist-hip ratio, a model of adipose distribution and visceral adiposity index. PLoS One. 2014. https://doi.org/10.1371/journal.pone.0114112.
Baveicy K, Mostafaei S, Darbandi M, Hamzeh B, Najafi F, Pasdar Y. Predicting metabolic syndrome by visceral adiposity index, body roundness index and a body shape index in adults: a cross-sectional study from the Iranian RaNCD cohort data. Diabetes Metab Syndr Obes Targets Ther. 2020;13:879.
Acknowledgements
We sincerely acknowledge the Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER) for providing us financial assistance in the form of an intramural Ph.D. research grant. Furthermore, we are thankful to all the subjects who participated in this study.
Funding
Funded by Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India. Grant ID: JIP/Res/Intramural/Phs-1/2018-19/98.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This study involved 202 human subjects after seeking approval from the JIPMER Institutional Ethics Committee (Human studies). This approval is valid for 3 years, and the project reference is JIP/IEC/2018/0301.
Informed consent
Prior to participation, all participants were given written and oral informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Endukuru, C.K., Gaur, G.S., Dhanalakshmi, Y. et al. Cut-off values and clinical efficacy of body roundness index and other novel anthropometric indices in identifying metabolic syndrome and its components among Southern-Indian adults. Diabetol Int 13, 188–200 (2022). https://doi.org/10.1007/s13340-021-00522-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-021-00522-5