Abstract
The influenza virus generally causes damage to epithelial cells of respiratory tract and infection of cells with this virus often results in cell death with apoptotic characteristics. Reports are available implicating influenza virus as a causative agent of chromosomal aberrations in cells and culture. The objective of this study was to analyze the process of cell death caused by influenza virus (A/Udorn/317/72, H3N2) infection in cultured HeLa cells by electron microscopy and comet assay. The apoptotic study was performed using light microscopy electron microscopy and comet assay to observe the changes in cell morphology and DNA fragmentation. HeLa cells, infected with influenza virus were harvested at various time periods to observe the ultrastructural changes. This infection gave rise to nuclear fragmentation and chromatin condensation accompanied by chromosomal DNA fragmentation into oligonucleosomes. The pattern of comet assay revealed that the apoptosis occurred due to fragmentation of the DNA of the cells which reached the maximum level at 36 h post infection. Ultrastructural study showed extensive chromatin condensation and nuclear fragmentation which are the characteristic features of apoptosis.
Similar content being viewed by others
Introduction
The influenza virus is major human pathogen and is well known for the worldwide pandemics and epidemics [9, 10]. The virus predominantly infects and damage epithelial cells of respiratory tract and often results in cell death with apoptotic characteristics. Infection of epithelial cells and lymphocytes has been shown to induce apoptosis in vitro [6, 14, 17, 24]. Infection with virulent influenza (H5N1) virus was also shown to induce lymphopenia and lymphocyte apoptosis in vivo [8, 25, 26]. Apoptosis also plays an important role in the pathogenesis of many infectious diseases, including those caused by viruses, bacteria and prions [1, 15, 20]. The mechanisms of virus-induced cell damage which is followed by cell death are not well understood [23]. Apoptosis induced by influenza viruses has been shown in a variety of cell lines [21, 29, 30]. Several viral factors, including M1, NS1, and NA proteins, have been reported to be related to apoptosis induction [13, 16, 30]. It has been observed that extensive budding of the virus particles on the membrane surface of the infected cells may cause cellular damage. However, cellular degeneration may be observed even with incomplete replication of the virus in cultured HeLa cells [5, 9]. Influenza A/Udorn (H3N2) virus infection results in apoptotic cell death of HeLa cells suggesting that viral replication is not the direct cause of cell lysis. In previous study we have reported that zinc supplementation was found to prevent apoptosis induced by influenza virus in HeLa cells [22]. Cell death may occur via the major morphologically and biochemically distinct mode called apoptosis which is considered to be a physiological process involved in normal tissue turnover which occurs during embryogenesis, ageing and turnout regression [28]. Apoptotic cells undergo several complex morphological changes, including development of fragmented nuclei, extensive chromatin condensation and loss of cell volume. Recent studies have indicated that many viruses carry genes, like NS1 and NA, which directly influence the apoptotic ability of their host cell thus changing the view about significance of apoptosis in determining the outcome of virus infections [14].
DNA fragmentation is a biochemical marker and hallmark of apoptosis. Apoptotic DNA cleavage generally proceeds in two stages, first producing large 50–300 kb fragments, and later oligonucleosomal pieces which create the characteristic DNA ladder. The infection of MDCK cells with Influenza A strain (A/Turkey/Ontario/7732/66) at various time intervals showed cellular DNA fragmentation [6].
In this study, we characterized the process of cell damage caused by influenza virus infection in cultured HeLa cells, and found that it induced fragmentation of chromosomal DNA into oligonucleosomes and also caused nuclear fragmentation due to chromatin condensation, suggesting that the cell death induced by influenza virus infection occurred through apoptosis. Further the confirmation of DNA fragmentation was done by neutral comet assay. The study provided a better insight into the role of apoptosis in the pathogenesis of influenza virus infection.
Materials and Methods
Virus and Infection of HeLa Cells
HeLa cells were obtained from NCCS Pune, India and cultivated in either 35-mm cell culture dishes or 25-cm2 culture flasks [3] (Greiner, Germany) with Eagle’s minimal essential medium (Sigma, USA) containing 10% fetal bovine serum (Sigma, USA) and antibiotics (100 U/ml penicillin, 100 μg/ml streptomycin, 0.25 mg/ml Fungizone, 50 μg/ml gentamicin; all from Bio Whittaker, USA) at 37°C in a 5% CO2 incubator [4]. A pathogenic strain of influenza virus (IV), A/Udorn/317/72 (H3N2), obtained from CDC, Atlanta in lyophilized form was originally propagated in embryonated chicken eggs and further grown in cultured HeLa cells. When HeLa cell cultures were 85 ± 90% confluent, the cultures were pretreated with 199 medium (Sigma, USA) and inoculated with influenza virus at a multiplicity of infection of approximately ten, 50% tissue culture infectious doses (TCID50) per cell for 45 min at 37°C. Control HeLa cells were mock infected with 199 medium alone. The mock and IV-infected HeLa cells were incubated at 37°C in 199 medium with 0.25% BSA (Sigma, USA) and 2 μg/ml TPCK-trypsin (Sigma, USA) for various times before analysis. The amount of virus released into the culture medium was determined by haemagglutination test and PFU assays.
PFU Enumeration
Virus particles in HeLa cell culture suspensions following IV infection were quantified by PFU enumeration using standard procedures [12]. Briefly, confluent monolayers of Madin Darby Canine Kidney cells were incubated with the culture supernatants collected at various time points after virus infection serially diluted in PBS containing 1% bovine serum albumin for 1 h at room temperature. The cells were then overlaid with Eagle’s minimal essential medium supplemented with 0.2% bovine serum albumin, 0.1% DEAE Dextran, 1 μg trypsin/ml and 0.8% agar, and maintained in a humid atmosphere containing 5% CO2 for 3 days. The agar media were then removed and the cells were fixed with 5% formalin solution and stained with 0.03% methylene blue solution. Visualized plaques were counted and the virus titer was expressed as log10 p.f.u./ml.
Morphological Evaluation of Influenza Virus Infected HeLa Cells
Haematoxylin and Eosin
Monolayers of HeLa cells were obtained on slides and infected with the virus. After 24 h incubation, the experiment was terminated and the slides were stained with Haematoxylin and Eosin, dried at room temperature and mounted in DPX. The morphological changes in the infected cells were compared with those of uninfected HeLa cells.
Electron Microscopy
Monolayer of HeLa cells were pelleted 24 h post-infection (p.i.), washed in PBS and fixed with Karnovsky’s fixative (4% paraformaldehyde and 1% glutaraldehyde) overnight. The fixed cells were then submitted for Transmission Electron Microscopy (TEM) to the All India Institute of Medical Sciences, at the Department of Electron Microscopy, and a detailed study of the ultra structural changes occurring during influenza A virus infection was conducted [27].
DNA Fragmentation Assay (by Neutral Comet Assay)
Treatment of Cell Culture
Monolayer of HeLa cells was prepared in tissue culture bottles and infected with the pathogenic strain of influenza A virus at an m.o.i. of 10. The experiment was terminated at various points of time, i.e. 0, 6, 18, 24, 36 h, respectively.
The cells were obtained by scraping the surface of tissue culture bottle gently with the help of a cell scraper, without decanting the growth medium. The suspended cells were collected in a centrifuge tube and centrifuged at 2000 rpm for 10 min. Cells were then washed twice with cold PBS and then re-suspended in 70% ethanol solution at a concentration of 1 × 106 cells/ml. Following this the cells were incubated for 30 min on ice for fixing the cells.
Comet Assay
A simple modification of the original neutral assay developed by Ostling and Johanson was used. At various time points after treatment with virus, cells were mixed with prewarmed 0.75% ultra-low gelling agarose (BDH Electran, BDH Laboratory Supplies, Poole, England; 44415 2G) and layered on microscopic slides precoated with 0.1% agarose. After incubation at 4°C to allow the formation of agarose gel, lysis was carried out by submerging the slides in lysis buffer (2.5% sodium dodecylsulfate, 1% sodium sarcosinate, and 25 mM ethylene-diaminetetraacetic acid, pH 9.5) for 15 min at 25–30°C. Slides were washed for 5 min in distilled water at 10°C and electrophoresed (90 mM Trizma base, 90 mM boric acid, and 2.5 mM ethylene-diaminetetra-acetic acid, pH 8.3) at 2 V/cm for 5 min at 10°C. Comets were stained with propidium iodide (25 IM in phosphate buffered saline) after rehydration of slides in distilled water for 5 min and observed under an Olympus BX60 fluorescence microscope (Olympus Optical Co., Tokyo, Japan) [19].
Results
Morphological Study
Virus infected HeLa cells 24 h p.i. was observed for morphological alterations by light microscopy after staining with Haematoxylin and Eosin. In contrast to uninfected cells, the infected cells exhibited extensive condensation of chromatin into several dense masses and compaction of cytoplasm associated with cytoplasmic vacuolization (Fig. 1a, b). A few infected cells also showed slightly swollen cytoplasm with less staining than that of uninfected cells but without remarkable chromatin condensation.
Electron Microscopy
Ultrastructural analysis of the infected HeLa cells on TEM revealed changes typical of apoptosis. The Fig. 2a and b shows an extensive shrinkage and vacuolization of the cytoplasm. Dense masses of cytoplasm were observed due to degradation of structural proteins (Fig. 2c, d). Further, chromatin condensation, nuclear fragmentation, and compaction of chromatin under the nuclear membrane were also observed (Fig. 2e, f).
Electron micrograph of influenza A virus-infected HeLa cells. Ultrastructural analysis of infected HeLa cells by TEM at 8200× (a) and 1450× (b) showing extensive Shrinkage and Vacuolization of Cytoplasm, 4200× (c) and 2900× (d) showing dense masses of cytoplasm and compaction of chromatin, 5400× (e, f) showing chromatin condensation, nuclear fragmentation and compaction of chromatin under the nuclear membrane
Comet Assay
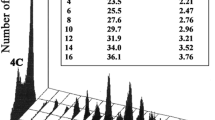
DNA fragmentation is a biochemical marker and hallmark of apoptosis. Thus, a confirmation of the occurrence of apoptosis due to influenza A virus infection was done by DNA fragmentation by neutral comet assay. The assay revealed the formation of three different types of comets, namely type A, B, C depending on the relative size of the comet head and tail (Fig. 3a). The type A comet indicated the initiation of fragmentation, with a large head and a bulging tail separated by a narrow “neck” region. Further progression of fragmentation resulted in a distinct type B comet with a larger tail and a smaller, circular head region. The type C comet had constantly diminishing head and neck regions, and an expanding tail was noted. The assay was performed at various time intervals of 0, 6, 18, 24, 36 h. It was observed that, fragmentation began at 6 h p.i. and classical fragmentation occurred at 36 h p.i. The figure presented showed that Type A and B comets appeared at a high frequency during early time points (0–6 h), whereas type C comets that indicated late stages of fragmentation, was observed after extended treatment (24–36 h) (Fig. 3b).
a Microscopic view of different types of comets observed after influenza virus infection during comet assay. b Microscopic evaluation of images from HeLa cells treated with Influenza A/Udorn/256/72 (H3N2) virus for different durations (0–36 h) show type A (blue arrow), B (green arrow), and C (pink arrow) comets reflecting progressive stages of DNA fragmentation. Images were acquired with a 10× objective
Discussion
A current challenge in the field of influenza A viral pathogenesis is to understand how virus infection leads to specific tissue damage and disease or death of the host. To address this question, apoptosis was examined as a potential mechanism of cell death during influenza A virus infection. The assumption was based on a few previous studies which have shown that all mammalian and avian influenza A strains induce apoptotic death of cultured cell lines as well as that of tissues in infected animals [2, 7]. However, the cellular signals leading to apoptosis are varied and may depend on the viral strain and the cell type. The influenza virus M1, NS1, and NA proteins have been reported to be related to apoptosis induction [13, 16, 30]. Also the importance of HA in apoptotic cell death in vitro is further supported by recent findings showing that the HA of the 1918 pandemic influenza virus enhances mortality in mice [11, 18, 26].
In this report we have shown morphological confirmation of occurrence of apoptosis using three methods, i.e. light microscopy after staining with Haematoxylin and Eosin, TEM and comet assay. Two types of changes were observed in the infected cells on light microscopy. One was extensive condensation of chromatin into several dense masses and compaction of cytoplasm associated with cytoplasmic vacuolization, characteristic features of apoptosis. A few cells also showed slightly swollen cytoplasm with less staining than that of uninfected cells but without remarkable chromatin condensation. The latter feature might be associated with cellular necrosis which could be due to the incubation for several hours or the pre-apoptotic state.
Staining with Haematoxylin and Eosin and TEM confirmed the occurrence of morphological changes characteristic of programmed cell death in the infected cells. The confirmation of the occurrence of apoptosis due to influenza A virus infection was done by analyzing the DNA fragmentation by neutral comet assay. The assay was performed at various time intervals of 0, 6, 18, 24, 36 h and it was observed that, though the fragmentation began at 6 h p.i. but classical fragmentation occurred only at 36 h p.i.
During the study using neutral comet assay, three different types of comets were observed. Type A comets had a large head separated by a narrow “neck” region from an oval bulging tail that indicated initiation of fragmentation. Type B and C comets had a constantly diminishing head associated with a corresponding expansion of the tail and reflected intermediate and late stages of fragmentation, respectively. Type A and B comets appeared at a high frequency during early time points (0–6 h), whereas type C comets that indicated late stages of fragmentation were observed only after extended treatment (24–36 h). The present study provided a better insight into the role of apoptosis in the pathogenesis of influenza virus infection. The study also provided information about the time of occurrence and sequence of few hallmark events during influenza A virus-induced apoptosis in host cells.
References
Collins M. Potential roles of apoptosis in viral pathogenesis. Am J Respir Crit Care Med. 1955;152:S20–4.
Geoch M, Fellner DP, Newton C. Influenza virus genome consists of eight distinct RNA species. Proc Natl Acad Sci. 1976;73:3045–9.
George VC, Hierholzer JC, Ades EW. Cell culture. In: Brian WJM, Hillar OK, editors. Virology methods manual. London: Academic Press Ltd.; 1996. p. 3–24.
Ha Y, Stevens DJ, Skehel JJ, Wiley DC. H5 avian and H9 swine influenza virus hamagglutinin structures: possible origin of influenza subtypes. EMBO J. 2002;21:865–75.
Henle G, Girardi A, Henle W. A non-transmissible cytopathogenic effect of influenza virus in tissue culture accompanied by formation of non-infectious hemagglutinins. J Exp Med. 1955;101:25–41.
Hinshaw VS, Olsen CW, Dybdahl-Sissoko N, Evans D. Apoptosis: a mechanism of cell killing by influenza A and B viruses. J Virol. 1994;68:3667–73.
Khanna M, Kumar P, Prasad AK. Influenza and its role in apoptosis. Indian J Allergy Appl Immunol. 2001;15:7–12.
Khanna M, Akther N, Srivastava V, Kumar P, Vijayan VK. Biological and epidemiological aspects of influenza virus H5N1 in context of India. Indian J Exp Biol. 2006;44:265–78.
Khanna M, Kumar P, Choudhary K, Kumar B, Vijayan VK. Emerging influenza virus: a global threat. J Biosci. 2008;33:475–82.
Khanna M, Gupta N, Gupta A, Vijayan VK. Influenza A (H1N1) 2009: a pandemic alarm. J Biosci. 2009;34:481–9.
Kobasa D, Takada A, Shinya K, Hatta M, Halfmann P, Theriault S, Suzuki H, Nishimura H, Mitamura K, Sugaya N, Usui T, Murata T, Maeda Y, Watanabe S, Suresh M, Suzuki T, Suzuki Y, Feldmann Y, Kawaoka Y. Enhanced virulence of influenza A viruses with the haemagglutinin of the 1918 pandemic virus. Nature. 2004;431:703–7.
Kurokawa M, Imakita M, Kumeda CA, Yukawa TA, Kakkon ShirakiK. Suppressed interleukin-1 production responsive to interferon and alleviated influenza infection in mice. J Tradit Med. 1996;13:201–9.
Lam WY, Tang JW, Yeung AC, Chiu LC, Sung JJ, Chan PK. Avian influenza virus A/HK/483/97(H5N1) NS1 protein induces apoptosis in human airway epithelial cells. J Virol. 2008;82:2741–51.
Lowy RJ. Influenza virus induction of apoptosis by intrinsic and extrinsic mechanisms. Int Rev Immunol. 2003;22:425–49.
Ludwig S, Pleschka S, Wolffm T. A fatal relationship—influenza virus interactions with the host cell. Viral Immunol. 1999;12:175–96.
Morris SJ, Price GE, Barnett JM, Hiscox SA, Smith H, Sweet C. Role of neuraminidase in influenza virus-induced apoptosis. J Gen Virol. 1999;80:137–46.
Nichols JE, Niles JA, Roberts NJ. Human lymphocyte apoptosis after exposure to influenza A virus. J Virol. 2001;75:5921–9.
Pappas C, Aguilar PV, Basler CF, Solorzano A, Zeng H, Perrone LA, Palese P, Garcia-Sastre A, Katz JM, Tumpey TM. Single gene reassortants 17 identify a critical role for PB1, HA, and NA in the high virulence of the 1918 pandemic influenza virus. Proc Natl Acad Sci. 2008;105:3064–9.
Raff MC. Social controls on cell survival and cell death. Nature. 1992;356:397–400.
Roulston A, Marcellus RC, Branton PE. Viruses and apoptosis. Annu Rev Microbiol. 1999;53:577–628.
Schultz Cherry S, Dybdahl Sissoko N, Neumann G, Kawaoka Y, Hinshaw VS. Influenza virus NS1 protein induces apoptosis in cultured cells. J Virol. 2001;75:7875–81.
Srivastava V, Rawall S, Vijayan VK, Khanna M. Influenza A virus induced apoptosis: inhibition of DNA ladering & caspase-3 activity by zinc supplementation in cultured HeLa cells. Indian J Med Res. 2009;129:579–86.
Sweet C, Smith H. Pathogenicity of influenza virus. Microbiol Rev. 1980;44:303–30.
Takizawa T, Matsukawa S, Higuchi H, Nakamura S, Nakanishi Y, Fukuda R. Induction of programmed cell death (apoptosis) by influenza virus infection in tissue culture cells. J Gen Virol. 1993;74:2347–55.
Tumpey TM, Lu X, Morken T, Zaki SR, Katz JM. Depletion of lymphocytes and diminished cytokine production in mice infected with a highly virulent influenza A (H5N1) virus isolated from humans. J Virol. 2000;74:6105–16.
Tumpey TM, Basler CF, Aguilar PV, Zeng H, Solorzano A, Swayne DE, Cox NJ, Katz JM, Taubenberger JK, Palese P, Garcia-Sastre A. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;310:77–80.
Uehara T, Miyawaki T, Ohta K. Apoptotic cell death of primed CD45RO+ T lymphocytes in Epstein-Barr virus-induced infectious mononucleosis. Blood. 1992;80:452–8.
Wyllie AH, Kerr JFR, Currie AR. Cell death: the significance of apoptosis. Int Rev Cytol. 1980;68:251–306.
Zamarin D, Garcia-Sastre A, Xiao X, Wang R, Palese P. Influenza virus PB1-F2 protein induces cell death through mitochondrial ANT3 and VDAC1. PLoS Pathol. 2005;1:e4.
Zhirnov OP, Ksenofontov AL, Kuzmina SG, Klenk HD. Interaction of influenza A virus M1 matrix protein with caspases. Biochemistry. 2002;67:534–9.
Acknowledgements
The author acknowledges the Indian Council of Medical Research (ICMR), New Delhi for providing the Senior Research Fellowship and also Department of Electron microscopy, All India Institute of Medical Sciences for Transmission Electron Microscopy (TEM) studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khanna, M., Ray, A., Rawall, S. et al. Detection of Influenza Virus Induced Ultrastructural Changes and DNA Damage. Indian J. Virol. 21, 50–55 (2010). https://doi.org/10.1007/s13337-010-0004-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13337-010-0004-1