Abstract
Background and Objective
Omeprazole is a proton pump inhibitor (PPI) that is used in acid suppression therapy in infants. In this study we aimed to develop a pediatric omeprazole suppository, with good physical and chemical stability, suitable for pharmaceutical batch production.
Methods
The composition of the suppository consisted of omeprazole, witepsol H15 and arginine (L) base. To achieve evenly distributed omeprazole suspension suppositories, the temperature, stirring rate, and arginine (L) base amount were varied. A previously validated quantitative high-performance liquid chromatography–ultraviolet method was modified and a long-term stability study was performed for one year.
Results
Evenly distributed omeprazole suspension suppositories were obtained by adding 100 mg arginine (L) base and pouring at a temperature of 34.7 °C and a stirring speed of 200 rpm. The long-term stability study showed no signs of discoloration and a stable omeprazole content between 90 and 110% over 1 year if stored in the dark at room temperature.
Conclusion
We developed a pediatric omeprazole suppository. This formulation may provide a good alternative to manipulated commercial or extemporaneously compounded omeprazole oral formulations for infants. Clinical studies are needed to establish efficacy and safety in this young population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We report the development of a pediatric omeprazole suppository, by adding witepsol and 100 mg arginine (L) base and pouring at a temperature of 34.7 °C and a stirring speed of 200 rpm. |
The one-year stability study found that the suppositories showed no signs of discoloration and that the omeprazole content remained stable between 90 and 110% if stored in the dark at room temperature. |
1 Introduction
Omeprazole (5-methoxy-2-[(RS)-[(4-methoxy-3,5-dimethylpyridin-2-yl)methyl]sulfinyl]-1H-benzimidazole), a proton pump inhibitor (PPI), inhibits gastric acid secretion by inactivating the H +/K + ATPase molecules of the parietal cell in the stomach mucosa selectively and non-competitively [1]. This effect on the final step of gastric acid formation is dose-dependent and inhibits both basal and stimulated gastric acid secretion. Omeprazole is a lipophilic weak base that decomposes in an acidic environment. To prevent decomposition in the acid environment of the stomach, an enteric coating is used in most oral formulations [1]. This coating is soluble in the alkaline environment of the small intestine and omeprazole is rapidly absorbed in the small intestine and passes into the bloodstream. Peak plasma concentrations occur in adults within 3–6 h and the bioavailability is around 60% after repeated dosing. The plasma half-life of omeprazole is approximately 1 h; however, the anti-secretory effect lasts for a more prolonged time due to irreversible binding to H +/K + ATPase molecules of the parietal cell.
PPIs are used in acid suppression therapy in infants with gastroesophageal reflux disease (GERD) [2]. GERD often occurs in infants with congenital anomalies, such as esophageal atresia (EA) or congenital diaphragmatic hernia (CDH) [3,4,5]. In contrast to adults, however, no commercially registered oral dosage form of omeprazole is available for infants younger than 1 year of age. Due to their small size, infants require a non-standard dose. Based on a small number of pharmacokinetic and clinical studies in infants, the starting dose is 1 mg/kg/day, which can be increased in steps of 0.5 mg/kg/day to a maximum of 3 mg/kg/day [6, 7]. Additionally, infants are unable to swallow oral tablets or capsules. In clinical practice, omeprazole is often administered as extemporaneous formulations by crushing the omeprazole microgranules, which may destroy the enteric coating, or by suspending the microgranules in water or sodium bicarbonate [8]. The amount of sodium bicarbonate needed to safely alkalize the gastric acid is not known for infants. When omeprazole tablets or capsules are dissolved in water or juice, infants may chew on the microgranules causing damage to the enteric coating. Consequently, the oral bioavailability of these extemporaneous omeprazole administrations may be unpredictable and may result in variable degrees of drug exposure although this has not been studied in the pediatric population [9]. This may also explain the reported low effectiveness of omeprazole in infants with GERD [7]. In particular, for infants who need nasogastric tube feeding, omeprazole administration via a gastric tube often results in omeprazole deposits and tube occlusion. The replacement of the nasogastric tube is a very stressful experience for the infants and their parents. It is clear that the current oral administration of omeprazole in infants results in unpredictable exposure levels and added burden for patients and parents. This reduces the drug compliance and does not contribute to a good clinical effect.
To increase the effectiveness of omeprazole therapy in infants, rectal administration may potentially overcome the limitations associated with oral omeprazole. Moreover, when young infants reject oral formulations, suppositories present a more secure way of drug administration. In 1969, Kerawalla et al. compared oral versus rectal indomethacin suppositories in young infants and found them to be well tolerated, convenient to administer, and showed no local side-effects [10]. A frequently prescribed drug for which suppositories are widely used as an alternative for oral formulations is acetaminophen [11, 12]. In addition, omeprazole as a suppository appears to be an effective dosage form in healthy adults, resulting in adequate systemic exposure and acid reduction [13, 14]. Hence, the aim of this study was to develop a pediatric omeprazole suppository suitable for infants with GERD, including adequate stability and suitability for pharmaceutical batch production.
2 Methods
The raw material, i.e., omeprazole and the pharmaceutical excipients, namely arginine (L) base and witepsol H15 were purchased from BUFA (BUFA, IJsselstein, The Netherlands) and were of European Pharmacopeia grade. BUFA is one of the suppliers designated by the NVZA (Dutch Association of Hospital Pharmacists). Omeprazole and the pharmaceutical excipients were processed by BUFA according to Pharmacopeia European Monograph and delivered with the corresponding certificate of analysis. Upon arrival of the materials in the hospital pharmacy (Rijnstate Hospital, Arnhem), an entry check was carried out in accordance with the analytical certificate. All other chemicals and solvents were of analytical reagent grade.
2.1 Composition
As a starting point for the design of the suppository, omeprazole, arginine (L) base, and witepsol H15 were included [13]. The dosage strengths of the omeprazole suppositories were chosen based on the oral omeprazole starting dose of 1 mg/kg and were aimed at the 6 weeks to 1 year age range. Omeprazole suppositories were produced in 8 different strengths (3 mg through 10 mg). The suppositories were produced with the suppository molding unit from Erweka (Gemini BV, Apeldoorn, The Netherlands). For omeprazole and arginine (L) base, a displacement factor of 0.65 was used. The used suppository molds were transparent and had a capacity of 1.15 ml. In order to achieve an evenly distributed omeprazole suspension suppository, the following factors were varied to obtain an optimal preparation process—temperature, stirring rate, and arginine (L) base amount per suppository (10 mg vs 100 mg), as described in more detail below.
2.2 Temperature and Stirring Speed
To optimize the suppository consistency and omeprazole distribution, the temperature of the suppository mass was varied in the range of 32–37 °C and the stirring speed was varied between 150 and 350 rpm. The consistency of the mass was determined by the uniformity of mass (European Pharmacopeia 9.0 Monograph, omeprazole). Physical analysis also included visual examination—shape, surface, color and texture. Distribution of omeprazole across the suppository was first determined in petroleum ether by visual examination. In addition, the suppository was sectioned laterally ensuring that each section (the point and tail of the suppository) quantitatively (Sect. 2.4) contained proportionally equal amounts of omeprazole.
2.3 Arginine (L) Base Amount per Suppository: 10 mg Versus 100 mg
Arginine (L) base was added to the omeprazole suppository to minimize degradation of the suppository during the storage period. Two different amounts of arginine (L) base (10 mg and 100 mg per suppository) were tested to investigate whether or not arginine (L) base affects the solidification time and omeprazole distribution over the suppository; arginine base (L) does not dissolve in the suppository base witepsol and as a result sedimentation and migration of the arginine (L) base to the bottom of the suppository can occur. The effects on the solidification time and the distribution of omeprazole and arginine (L) base over the suppository were determined.
2.4 Analytical Method
For the quantitative analysis of omeprazole and related compound (European Pharmacopeia 9.0 Monograph omeprazole) D [5-methoxy-2-[[(4-methoxy-3,5-dimethylpyridin-2-yl)methyl]sulfonyl]-1H-benzimidazole(omeprazole sulphone), a high-performance liquid chromatography combined with ultraviolet (HPLC–UV) method was used, modified from the European Pharmacopeia 9.0 Monograph of omeprazole.
This method was modified because omeprazole, the degradation products (including omeprazole sulphone) and the internal standard lansoprazole had to be separately detectable. By modifying the method, good chromatograms with sharp, separated peaks were obtained in a single run. Measurements were also taken at 302 nm instead of 280 nm.
Omeprazole was removed from the suppository by extraction, since omeprazole is very slightly soluble in water. The suppository was placed in an Erlenmeyer flask and 25 ml of dichloromethane, 10 ml of internal standard lansoprazole solution (3 mg/l) and 15 ml of 0.1 mol/l sodium hydroxide were added. The Erlenmeyer flask was shaken vigorously for 1 min after which 250 µl of the top layer was pipetted into a 10 ml volumetric flask and supplemented with the eluent. Omeprazole, lansoprazole and omeprazole sulphone were separated using a Shimadzu LC20 system on a C18 analytical column (Inertsil ODS-5) with a mixture of acetonitrile R (standardized pharmacopoeia solution) and a solution of 1.4 g/L disodium hydrogen phosphate R, adjusted to the right pH with phosphoric acid R (standardized pharmacopoeia solution) as a mobile phase at a flow rate of 1 ml/min. UV detection for quantification was kept at a wavelength of 302 nm. The injection volume was 25 µl.
The composition of the eluent (proportion of phosphate buffer/acetonitrile), the pH, and the column temperature were varied to achieve an optimal analytical method; peaks had to be well separated and should not tail. Lansoprazole was chosen as the internal standard for the omeprazole HPLC method since lansoprazole is also a PPI and behaves chemically in the same way as omeprazole, with no overlap in the chromatogram with omeprazole or omeprazole-sulphone. The method was validated for the quantification of omeprazole in the sample matrix witepsol H15 and in the presence of omeprazole sulphone. The validation parameters are shown in Table 1.
2.5 Long-Term Stability Study
The influence of light and temperature on the long-term stability of the omeprazole suppositories was investigated. For this study, the definitive composition of the omeprazole suppositories was used, which consisted of witepsol H15, omeprazole, and 100 mg arginine (L) base. Omeprazole suppositories with the lowest strength of 3 mg (A) and with the highest strength of 10 mg (B) were studied over one year. The samples were stored under the following conditions, namely:
-
(1)
in a climate cabinet at 4 °C (range 2–8 °C)
-
(2)
in the dark at room temperature (< 25 °C)
-
(3)
in daylight at room temperature (< 25 °C).
The temperature of the climate cabinet was monitored and registered. The samples were analyzed at 0, 1, 2, 3, 4, 5, 6, 9 and 12 months using the modified stability-indicating HPLC–UV method for determination of omeprazole and omeprazole sulphone. End-of-shelf-life specifications are based on the European Pharmacopeia 9.0 Monograph for omeprazole—the suppositories must not be colored and the omeprazole content must be between 90 and 110%.
2.6 Manufacturing Procedure
The manufacturing procedure was developed for batch compounding. The arginine (L) base was first rubbed finely into a rough stone mortar followed by omeprazole mixed in equal parts with the arginine (L) base. Witepsol H15 was melted in a stainless steel mortar on a water bath of 50–60 °C, while stirring continuously, after removing from the water bath before the mass had completely melted, and the temperature was measured (40–45 °C). Next, the omeprazole–arginine (L) base mixture was mixed with equal parts of witepsol H15, followed by the remaining witepsol H15. At a temperature of 35–35.5 °C, the suppository mass was transferred to the suppository molding machine and poured in suitable rectal forms.
2.7 Statistical Analysis
We calculated the recovery and coefficient of variation (CV) as the mean of 6 different samples analyzed by one laboratory technician. For the inter-assay CV, the values of three technicians were used. All of these values were compared with standard specifications as listed in Table 1. For linearity, the lack-of-fit and goodness-of-fit were assessed using four concentrations in the range of 1–15 mg/L measured in triplicate and compared with the F value for the relevant degrees of freedom and a p value of 0.05. SPSS Statistics, version 26.0 (IBM Corp, New York, USA) was used for statistical analysis.
3 Results
3.1 Composition
Based on the data regarding the temperature, the stirring speed, and the amount of arginine (L) base (as described below in more detail), 100 mg of arginine (L) base was added per suppository, and the suppositories were poured at a temperature of 34.7 °C, and a stirring speed of 200 rpm was used. The composition of a 4-mg omeprazole suppository consists of 4 mg omeprazole, 100 mg arginine (L) base and 1,002 g witepsol H 15. The batch size was 600 suppositories at a time.
3.2 Temperature and Stirring Speed
A pouring temperature > 35 °C and a stirring speed < 180 rpm resulted in the sedimentation and migration of the omeprazole and the arginine (L) base to the bottom of the suppository. A pouring temperature < 34.5 °C and a stirring speed of > 250 rpm resulted in suppositories that were too light and too brittle. Optimal omeprazole suppositories were obtained when poured at a temperature of 34.7 °C and a stirring speed of 200 rpm. The suppositories were torpedo shaped, white colored and homogeneous with no cracks/air bubbles/bursts, and the inside and outside of the suppository had a smooth uniform surface. The suppositories met the requirements of the uniformity of mass. Each section of the suppository (point and tail) contained proportionally equal amounts of omeprazole.
3.3 The Arginine (L) Base Amount per Suppository: 10 mg Versus 100 mg
Adding 100 mg of arginine (L) base to the suppository resulted in a good omeprazole distribution across the suppository (point and tail analysis). The arginine (L) base amount (10 mg or 100 mg) did not affect the solidification time and the distribution. Arginine (L) base was added to the suppository to prevent degradation; this pharmaceutical excipient is not absorbed by the intestine and can therefore be used safely in children. If a suppository contains < 50 mg of pharmacon then 100 mg of filler should be added. Since a good suppository was obtained with both 10 mg and 100 mg arginine (L) base, the decision was made to add 100 mg arginine (L) base, because the arginine (L) base can also be used as a filler to supplement the amount of solids to > 100 mg, obviating the need of other fillers.
3.4 Analytical Method
A previously reported HPLC–UV method was modified and validated. Omeprazole, lansoprazole and omeprazole sulphone were separated on a C18 analytical column with a mixture of acetonitrile R and a solution of 1.4 g/L disodium hydrogen phosphate R, adjusted to pH 6.5 with phosphoric acid R (72.5: 27.5) as a mobile phase at a flow rate of 1 ml/min. With changes in the composition of the eluent (proportion of phosphate buffer 70–75/acetonitrile 25–30) and the pH 6.5–8.5, the retention time, the peak shape, and the separation changed. This mobile phase displayed well-separated sharp peaks and no tailing. The retention times were omeprazole 3.3 min, omeprazole sulphone 4.5 min, and lansoprazole 7.5 min. The column temperature was optimal at 25°C. Increasing the column temperature deteriorated the shape of the peaks. UV detection for quantification was kept at a wavelength of 302 nm. The injection volume was 25 µl. The validation parameters of the HPLC–UV method developed are shown in Table 1. The most effective mobile phase obtained consisted of a mixture of acetonitrile R and a solution of 1.4 g/L disodium hydrogen phosphate R adjusted to pH 6.5 with phosphoric acid R.
3.5 Specificity
The influence of the matrix (witepsol H15 and arginine (L) base) on the chromatogram was determined by preparing a test formulation without the active substance and handling this test formulation in the same way as a test formulation with omeprazole. No disturbing peaks of the matrix were present in the chromatogram. For further validation, arginine (L) base was not included, since it does not dissolve and remains on the bottom of the Erlenmeyer flask.
3.6 Recovery
The recovery of the components to be determined in the matrix was investigated using the test mixture method. The recovery was determined by making two 8-point calibration lines. One calibration curve included the matrix and extraction and the other calibration line was made without matrix and extraction. The comparison of the calibration lines showed that the extraction procedure had no influence on the recovery, since the two lines differed little from each other in terms of correlation and slope. Therefore, the decision was made to continue to use the calibration curve with matrix and extraction in the study as it mimics the composition and the work-up of the omeprazole suppository.
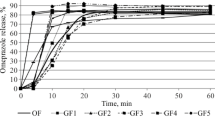
3.7 Long-Term Stability Study
After storage of the suppositories for 1 year under conditions 1 [in a climate cabinet at 4 °C (range 2–8 °C)] and 2 [in the dark at room temperature (< 25 °C)], the color, weight and content (within 90–110% range) remained stable (Fig. 1). After storage under condition 3 for 1 year [in daylight at room temperature (< 25 °C)], the suppositories were discolored to yellow and the content had fallen sharply (± 85% of the declared value of the omeprazole 10 mg suppositories and ± 70% of the declared value of the omeprazole 3 mg suppositories). On the basis of the shelf life test, the suppositories need to be kept at room temperature in the dark to guarantee a shelf life of 1 year for all strengths of the omeprazole suppositories tested.
4 Discussion
In this study, we developed omeprazole suppositories of 3–10 mg with good physical and chemical stability, which are suitable for use in infants. The manufacturing process was optimized and is suitable for preparing small or large batches. The long-term stability study showed a shelf life of 1 year provided the suppositories are stored in the dark at room temperature.
As the basis for this omeprazole suppository, the same pharmaceutical excipients as in the study by Choi et al. [13] were used. Witepsol H15 is used frequently as a suppository base in many infant suppositories and can be used safely. Arginine (L) base is added to the suppository to minimize degradation of the omeprazole suppository; this pharmaceutical excipient is not absorbed by the intestine and can therefore be used safely in children. Choi et al. used 1% arginine (L) base (w/w) per suppository and did not investigate different amounts of arginine (L) base. In our study, we examined whether the amount of arginine (L) base (10 mg or 100 mg) affected the quality of the suppositories. Arginine base (L) does not dissolve in the suppository base witepsol and, as a result, sedimentation and migration of the arginine (L) base to the bottom of the suppository can occur. However, in the study by Choi et al., the preparation process is described very briefly, with only the temperature during mixing being mentioned. The stirring speed and the pouring temperature were not investigated, but are of great importance for preparing a good suppository. We tested two different amounts of arginine (L) base (10 mg and 100 mg) per suppository.
With both quantities (10 mg and 100 mg), an evenly distributed suppository was obtained. By adding 100 mg arginine (L), we obviated the need to use an additional filler. This is especially relevant in infants, where toxicity of excipients may present as a higher risk than in adults. For a good clinical result, omeprazole suppositories have to be prepared with a good distribution of omeprazole across the suppository.
The biggest challenge in the development of the omeprazole suppository was to prevent the sedimentation and migration of the omeprazole and arginine (L) base to the tip of the suppository. In a suspension suppository, the pharmaceutical particles may settle down as long as the base has not yet solidified. The omeprazole suppository must be poured at the lowest possible temperature and, once poured, it must be solidified immediately to prevent the omeprazole from settling down in the tip of the suppository, which partly remains in the strip. The stirring speed was also of great importance. A too low stirring speed resulted in omeprazole suppositories which showed settlement in the tip and a too high stirring speed resulted in omeprazole suppositories which were too brittle and too light due to too much air being impacted. Optimal omeprazole suspension suppositories were obtained with 100 mg arginine (L) base, pouring at a temperature of 34.7 °C and a stirring speed of 200 rpm. For quantitative analysis of omeprazole, the internal standard and omeprazole sulphone, a previously developed HPLC–UV method was modified and validated. The composition of the eluent, the pH of the eluent and the column temperature were optimized to obtain the most suitable analytical method.
Another challenge was to quantify omeprazole in the omeprazole suppositories, since omeprazole is only very slightly soluble in water. An extraction method was developed to separate omeprazole from the witepsol H15. The suppository was placed in a mixture of dichloromethane, internal standard and 0.1 mol/l of sodium hydroxide and, after shaking for one minute, the omeprazole, omeprazole-sulphone (if present) and internal standard were separated from the witepsol and were located in the upper layer of the mixture. A small amount of this layer was further processed to be injected on the HPLC–UV. To obtain suppositories with a good shelf-life, storage in the dark at room temperature was important to prevent the suppositories from discoloring and to ascertain stable omeprazole concentrations.
4.1 Limitations
The omeprazole suppositories were successfully formulated at laboratory scale; however, to scale-up to commercial production, more research is necessary. Scaling up requires other pieces of equipment, the suppository mass is larger and the suppositories are often cooled after pouring into molds. As a result, the pouring temperature and the stirring speed can be different when scaling up, and research is necessary into the relationship between melting and solidification time. All of these factors are extremely critical for the physical and chemical properties of the final suppositories.
In this study we do not have clinical data to provide information about the effectiveness and the pharmacokinetic parameters. This information is provided in an accompanying article [15]. We have not conducted research on parental acceptance and preference for suppositories versus oral medications, so we cannot make any assumptions about their use in the clinic.
5 Conclusion
We developed and validated a pediatric omeprazole suppository suitable for infants with GERD. To study the efficacy and pharmacokinetics of this newly developed omeprazole suppository in infants with GERD due to EA or CDH we conducted a randomized controlled trial [15]. In this trial, we compared rectally administered with orally administered omeprazole and found a consistent increase in intraesophageal and gastric pH in infants with EA- or CDH-related GERD, similar to an oral dose. Since the manufacturing process is suitable for batch compounding we conclude that rectal omeprazole presents as an innovative, promising alternative for infants with pathological GERD.
References
Howden CW. Clinical pharmacology of omeprazole. Clin Pharmacokinet. 1991;20:38–49.
Rosen R, Vandenplas Y, Singendonk M, Cabana M, Dilorenzo C, Gottrand F, et al. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatric Gastroenterol Nutr. 2018;66:516–54. https://doi.org/10.1097/MPG.0000000000001889.
Peetsold MG, Kneepkens CF, Heij HA, IJsselstijn H, Tibboel D, Gemke RJ. Congenital diaphragmatic hernia: long-term risk of gastroesophageal reflux disease. J Pediatric Gastroenterol Nutr. 2010;51:448–53. https://doi.org/10.1097/MPG.0b013e3181d1b149.
Tovar J, Fragoso A. Gastroesophageal reflux after repair of esophageal atresia. Eur J Pediatr Surg. 2013;23:175–81. https://doi.org/10.1055/s-0033-1347911.
Marseglia L, Manti S, D’Angelo G, Gitto E, Salpietro C, Centorrino A, et al. Gastroesophageal reflux and congenital gastrointestinal malformations. World J Gastroenterol. 2015;21:8508. https://doi.org/10.3748/wjg.v21.i28.8508.
Gibbons TE, Gold BD. The use of proton pump inhibitors in children: a comprehensive review. Paediatr Drugs. 2003;5:25–40.
Bishop J, Furman M, Thomson M. Omeprazole for gastroesophageal reflux disease in the first 2 years of life: a dose-finding study with dual-channel pH monitoring. J Pediatric Gastroenterol Nutr. 2007;45:50–5. https://doi.org/10.1097/MPG.0b013e318049cbcc.
Zimmermann AE, Walters JK, Katona BG, Souney PE, Levine D. A review of omeprazole use in the treatment of acid-related disorders in children. Clin Ther. 2001;23:660–79.
Litalien C, Théorêt Y, Faure C. Pharmacokinetics of proton pump inhibitors in children. Clin Pharmacokinet. 2005;44:441–66.
Kerawalla FC, Rele V, Mehta A. Antipyretic effects of indomethacin suppositories: a double-blind study. Indian Pediatr. 1969;6:422–5.
Cuzzolin L, Antonucci R, Fanos V. Paracetamol (acetaminophen) efficacy and safety in the newborn. Curr Drug Metab. 2013;14:178–85.
Goldstein LH, Berlin M, Berkovitch M, Kozer E. Effectiveness of oral vs rectal acetaminophen: a meta-analysis. Arch Pediatr Adolesc Med. 2008;162:1042–6. https://doi.org/10.1001/archpedi.162.11.1042.
Choi MS, Chung SJ, Shim CK. Rectal absorption of omeprazole from suppository in humans. J Pharm Sci. 1996;85:893–4. https://doi.org/10.1021/js950375w.
Zylicz Z, van Sorge AA, Yska JP. Rectal omeprazole in the treatment of reflux pain in esophageal cancer. J Pain Symptom Manage. 1998;15:144–5.
Bestebreurtje P, Roeleveld N, de Koning BAE, Knibbe CAJ, Tibboel D, van Groen B, van de Ven CP, Plötz FB, de Wildt SN. Rectal omeprazole in infants with gastroesophageal reflux disease: a randomized pilot trial. Eur J Drug Metab Pharmacokinet. 2020. https://doi.org/10.1007/s13318-020-00630-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There was no funding for this study.
Conflicts of Interest
The authors declare no conflict of interest.
Statement of Human and Animal Rights
This article does not contain any studies with human and animal subjects performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bestebreurtje, P., Roeleveld, N., Knibbe, C.A.J. et al. Development and Stability Study of an Omeprazole Suppository for Infants. Eur J Drug Metab Pharmacokinet 45, 627–633 (2020). https://doi.org/10.1007/s13318-020-00629-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-020-00629-1