Abstract
Irisin was discovered as a PGC-1a-activated messenger of myocytes that links sedentary lifestyle, obesity, and diabetes. In this study, we investigated the short-term prognostic value of early measurement of irisin concentration in 1530 Han Chinese patients with acute ischemic stroke (AIS) from three stroke centers. The subjects were the first-ever AIS patients who were hospitalized at three stroke centers during the period from January 2015 to December 2016. Clinical information and stroke severity were collected at admission. Neurological evaluations were conducted at the 6-month follow-up. Serum levels of irisin, National Institutes of Health Stroke Scale (NIHSS), and conventional risk factors were evaluated to determine their value to predict functional outcome and mortality within 6 months. Multivariate analyses were performed using logistic regression models. During follow-up, a poor functional outcome was found in 588 patients (38.4%; 95% confidence interval (CI), 36.0–40.9%), and 325 patients died (21.2%; 95% CI, 19.2–23.3%). The stroke patients included in the study were divided into four groups according to irisin quartiles (first is the lowest level). Poor outcome across the irisin quartiles ranged from 54.5% (first quartile) to 21.7% (fourth quartile), and mortality rate ranged from 39.3% (first quartile) to 6.3% (fourth quartile). In a multivariate model using the first quartile (Q1) of irisin vs. Q2–Q4 together with the clinical variables, the marker displayed prognostic information and increased odds ratios of poor outcome by 58% (OR for Q1, 1.58 [95% CI, 1.12–2.43]) and mortality by 185% (OR for Q1, 2.85 [95% CI, 1.79–4.02]). In addition, a model containing known risk factors plus irisin compared with a model containing known risk factors without irisin showed a greater discriminatory ability to predict poor outcome (the area under the curve (AUC) with an increase from 0.73 to 0.75 [95% CI, 0.70–0.81]) and mortality (the AUC increased from 0.80 to 0.83 [95% CI, 0.78–0.87]). Irisin is a novel, independent prognostic marker improving currently used risk stratification of stroke patients. Further studies are needed to confirm this association, which may pave the way to new therapeutic options. Trial registration: ChiCTR-OPC-17013501
Similar content being viewed by others
Introduction
Irisin is a small polypeptide hormone that is released by cleavage of the extracellular component of fibronectin type III domain-containing protein 5 (FNDC5) [1]. The level of secreted irisin is commonly increased by exercise [2]. It is almost ubiquitously expressed in various tissues including cardiac tissue [3] with low basal levels in the liver, lung, skeletal muscle, and testis [4].
Previous studies have shown that circulating levels of irisin and/or irisin mRNA expression are negatively linked to anthropometric and biochemical parameters [5, 6], obesity [6], insulin resistance [7] or type 2 diabetes [8], metabolic syndrome [9], and central nervous system energy metabolism [10]. Due to the crosstalk between metabolic dysfunction and cardio-cerebrovascular diseases, a role for irisin in the cardio-cerebrovascular system is also expected. A previous study reported that the gradual decrease of serum irisin might be a diagnostic marker for myocardial infarction (MI) [11].
Interestingly, Endres et al. [12] found that physical activity decreases the risk of stroke and suggested a prevention strategy during cerebral ischemia by increasing blood flow and reducing brain injury. However, another study reported that increased irisin levels were associated with the development of major adverse cardiovascular events (MACEs) in patients with established coronary artery disease after percutaneous coronary interventions (PCIs) [13]. It should be noted that the small sample size (n = 103) reduced the reliability of results. According to the studies mentioned above, we hypothesized that serum irisin concentration is associated with functional outcome in stroke patients. In this study, we therefore investigated the short-term prognostic value of early measurement of irisin concentration in 1530 Han Chinese patients with acute ischemic stroke (AIS) from three stroke centers.
Methods
Study Population
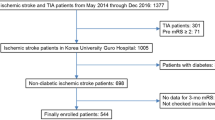
The subjects were first-ever AIS patients who were hospitalized at three stroke centers (Beijing, Weifang, and Wuhan) during the period from January 2015 to December 2016. Some information has been reported previously [14]. AIS was defined according to the World Health Organization Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (WHO-MONICA) criteria and was verified by magnetic resonance imaging (MRI) reports performed within 24 h after admission. Patients with basic diseases that affect irisin concentration or metabolism were excluded. The exclusion criteria were as follows: (1) pre-stroke diagnosis of dementia or cognitive impairment, a history of any psychiatric illness, and decreased level of consciousness; (2) malignant tumor, sarcopenia, liver insufficiency and renal insufficiency (creatinine > 1.5 mg/dl), metabolic abnormalities (not included diabetes), severe edema, and autoimmune diseases; and (3) use of psychotropic drugs prior to stroke onset. Written informed consents were obtained from all patients. This study conformed with the principles of the Declaration of Helsinki and was approved by the investigational review board of the Weifang Medical University (Trial registration: ChiCTR-OPC-17013501; retrospectively registered on 23 September 2017).
Clinical Variables and Follow-Up
At baseline, demographic data (age, sex, and body mass index (BMI)) and the following vascular risk factors: hypertension, diabetes mellitus, hypercholesterolemia, smoking, and a family history of ischemic stroke were collected. Pre-stroke therapy (oral anticoagulants or antiplatelet agents) and acute treatment (IV thrombolysis and/or mechanical thrombectomy) were also recorded. Patients were evaluated with the National Institutes of Health Stroke Scale (NIHSS) [14] score upon their admission, performed by a certified stroke neurologist. Stroke subtype was classified according to the TOAST (Trial of Org 10172 in Acute Stroke Treatment) criteria. Brain imaging (MRI) was done routinely within 24 h after admission. MRI with diffusion-weighted imaging (DWI) was available for some patients. The infarct volume was calculated by using the formula 0.5 × a × b × c (where a is the maximal longitudinal diameter, b is the maximal transverse diameter perpendicular to a, and c is the number of 10-mm slices containing infarct) [15].
The primary end point was functional outcome at 6 months post stroke. Structured follow-up telephone interview was used if the patients are already discharged. The follow-up using a standardized interview protocol was conducted by well-trained interviewers. If the patients had been discharged at the time of follow-up, a structured telephone interview was conducted. Functional outcome was assessed by the modified Rankin Scale (mRS) [16] blinded to serum biomarkers. A good functional outcome was defined as an mRS of 0–2 points, whereas a poor outcome was defined as an mRS of > 2 points [17]. Secondary end points were all-cause mortality within 6 months.
Blood Collection and Laboratory Test
All blood samples were collected on the first day of admission in the fasting state. Blood samples were centrifuged at 1000×g for 12 min, and serum was separated and stored at − 80 °C until the time of assay. Biochemical measurements were done using standard laboratory methods. The levels of serum total cholesterol (TC), triglycerides (TGs), high-sensitivity C-reactive protein (Hs-CRP), glucose, homocysteine (HCY), and high-density lipoprotein cholesterol (HDL-C) were measured by enzymatic assays, and fasting glucose levels were measured using the hexokinase method (auto-analyzer model 7600 II; Hitachi, Tokyo, Japan). Insulin resistance (IR) was estimated from fasting serum measurements using the homeostasis model assessment of insulin resistance (HOMA-IR): insulin (μIU/ml) × glucose (mmol/l) / 22.5. Serum irisin concentrations were measured in duplicate using an enzyme-linked immunosorbent assay (ELISA) kit (Aviscera Bioscience, Santa Clara, CA, USA) in accordance with the manufacturer’s instructions. The lower limit of detection (LOD) was 1.0 ng/ml, and the linear range of the standard was 1–500 ng/ml. The intra- and inter-assay coefficients of variation (CVs) were 3.3–5.0 and 4.3–6.8%, respectively. Serum interleukin-6 (IL-6) was determined by ELISA (Human IL-6 Quantikine ELISA Kit; R&D Systems, Inc., Minneapolis, MN, USA). For all measurements, levels that were less than LOD were considered to have a value equal to the LOD of the assay. Assays were performed in an independent laboratory blinded to clinical and neuroimaging data.
Statistical Analysis
Results are expressed as percentages for the categorical variables and as means (standard deviation, SD) or medians (quartiles) for the continuous variables, depending on the normal or non-normal distribution of data. Proportions were compared using the chi-square test, and Student’s t test and analysis of variance (ANOVA) were employed for the normally distributed variables, while the Mann–Whitney U test was employed for the asymmetrically distributed variables. Spearman’s rank correlation was used for bivariate correlations.
The relationship between serum concentrations of irisin and two end points (functional outcome and mortality) was evaluated using univariate and multivariate logistic regression analyses. As a continuous variable, we calculated odds ratios (ORs) for outcome per unit increase in irisin levels. We used crude models and multivariate models adjusted for all significant predictors. For multivariate analysis, categorical variables included age, sex, BMI, stroke etiology, the NIHSS score, infarct volume, pre-stroke and acute treatment, vascular risk factors, lesion location, HOMA-IR, blood levels of glucose, Hs-CRP, HCY, IL-6, TG, TC, HDL, LDL, and irisin quartiles. For a more detailed exploration of the irisin and two end points, we also used multivariate analysis models to estimate the adjusted OR and 95% CIs of outcome for irisin quartiles (with the highest irisin quartile as reference). Furthermore, included stroke patients were divided into two groups [low concentration group (first quartile, Q1) and normal concentration groups (second to fourth quartiles, Q2–Q4)] according to irisin quartiles. We also calculated ORs for the outcome between those two groups.
Second, receiver operating characteristic (ROC) curves were used to test the overall predicted accuracy of irisin and other markers to diagnose poor functional outcome and mortality, and results were reported as the area under the curve (AUC). The cutoff points of irisin from ROC analyses could be calculated, but this approach was clinically meaningless. It was unlikely anyone would ever use these cutoff points to predict future outcome in new patients with stroke. Furthermore, irisin was tested by ELISA kits that had great variability among the kits. Therefore, it was difficult to form a unified cutoff in different research populations. Thus, a cutoff level for serum irisin concentration to predict the stroke outcome was not used.
To test whether irisin level improves score performance, we considered the two nested logistic regression models with irisin and the established risk factors as compared with the established risk factors only. Under the lower-dimensional submodel, the difference in the deviation between the two models has an X2 distribution with 1 degree of freedom. Furthermore, care was taken to adjust for the optimistic bias of in-sample prediction error estimates using a fivefold cross-validation scheme. Letting Y be the indicator of the event of interest and X the covariate vector of a given risk score, high utility corresponds to accurately modeling the regression: E (Y|X = x). Brier’s score as the quadratic scoring rule to measure predictive performance was used. The fitted values of the predictive probabilities, Pr (Y = 1|X = x), are contrasted with the actually observed values.
Lastly, integrated discrimination improvement (IDI) and net reclassification improvement (NRI) indices were also calculated to determine the clinical utility of the addition of irisin to established risk factors and the ability of irisin to improve functional outcome and mortality prediction [18]. All statistical analyses were performed with SPSS for Windows, version 21.0 (SPSS Inc., Chicago, IL, USA), the ROCR package (version 1.0-2), and GraphPad Prism 5.0. Statistical significance was defined as P < 0.05.
Results
Patient Characteristics
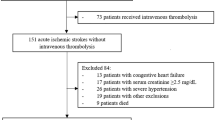
From 2193 screened patients, ischemic stroke was diagnosed in 1710 patients, and 1530 completed a 6-month follow-up and were included in the analysis (Fig. 1). These 1530 patients were similar in terms of baseline characteristics [age (P = 0.283), gender (P = 0.802), BMI (P = 0.376), and NIHSS score (P = 0.181)] compared to the overall screened patients with AIS (n = 2193). The baseline characteristics of the patients are described in Table 1. In this population, 796 (52.0%) were male, and the median age was 66 years (IQR, 57–77). At admission, the median NIHSS score was 8 (IQR, 4–13), and 233 patients (15.2%) received endovascular/surgical revascularization.
Association of Irisin with Established Risk Factors
As shown in Table 1, patients with higher irisin levels were younger, with lower BMI, less likely to have diabetes mellitus and coronary heart disease; had lower NIHSS score, small DWI, more likely to have received acute treatment; had lower blood levels of fasting blood glucose (FBG), CRP, HCY, TC, TG, LDL, and IL-6 (Table 1). Furthermore, Spearman’s analysis showed that irisin was further negatively correlated with NIHSS score, age, BMI, FBG, Hs-CRP, LDL, TG, TC, IL-6, HCY, and infarct volume and positively correlated with HDL (P < 0.01, all), as shown in Table 2.
Irisin and Functional Outcome
A poor functional outcome, defined by the mRS, was found in 588 patients (38.4%; 95% CI, 36.0–40.9%). Irisin level in patients with poor outcome was significantly lower than that in patients with good outcome (79.8 [IQR, 61.9–118.3] ng/ml vs. 94.9 [IQR, 71.2–146.5] ng/ml; Z = 8.359; P < 0.001; Fig. 2a). The poor outcome rate across irisin quartiles ranged from 54.5% (first quartile) to 21.7% (fourth quartile). The P value for the trend was less than 0.001 (Fig. 3a). In univariate logistic regression analysis, with an unadjusted OR of 0.985 (95% CI, 0.977–0.991; P < 0.001), low levels of irisin had a strong association with poor functional outcome. After adjusting for all other predictors, irisin was still a predictor of poor outcome with an adjusted OR of 0.990 (95% CI, 0.985–0.994; P < 0.001). In multivariate models comparing Q1, Q2, and Q3 against Q4 of irisin (Table 3), levels of irisin in Q1 and Q2 were associated with poor outcome, and the odds ratios were increased by approximately 205% (OR = 3.05; 95% CI, 2.11–4.32) and 64% (1.64; 1.14–2.48). The independent association of irisin with poor outcome was confirmed using the likelihood ratio test (P = 0.015). In a multivariate model using Q1 of irisin vs. Q2–Q4 together with the clinical variables, the marker displayed prognostic information and increased the odds ratio by 58% (OR for Q1, 1.58 [95% CI, 1.12–2.43]).
Baseline irisin in different stroke categories. a Irisin in stroke patients with good and poor functional outcomes. b Irisin in survivors and non-survivors of stroke. Mann–Whitney U test. All data are medians and interquartile ranges (IQRs). Poor functional outcome was defined as a modified Rankin Scale (mRS) of 3–6
The area under the ROC curve to predict poor outcome for irisin with an AUC of 0.70 (95% CI, 0.65–0.76; Fig. 4a) was in the range of the NIHSS with an AUC of 0.69 (0.64–0.75; P = 0.623). Irisin had a higher prognostic accuracy as compared to FBG [AUC, 0.60 (95% CI, 0.54–0.66); P < 0.001], Hs-CRP [AUC, 0.64 (0.58–0.69); P = 0.001], HCY [AUC, 0.61 (0.56–0.66); P < 0.001], and IL-6 [AUC, 0.63 (95% CI, 0.59–0.68); P < 0.001]. The combined model (irisin/NIHSS) could improve the NIHSS score [AUC of the combined model, 0.72 (95% CI, 0.69–0.77); P = 0.022]. A significant difference in the AUC between the established risk factors alone and the addition of irisin concentrations was observed (difference, 0.02 [95% CI, 0.01–0.03]; P = 0.031) (Table 4). This improvement was stable in an internal fivefold cross-validation that resulted in an average AUC (standard error) of 0.73 (0.034) for the established risk factors and 0.75 (0.030) for the combined model, corresponding to a difference of 0.02 (0.011). The fivefold cross-validated mean squared prediction error decreased from 0.166 (0.010) in the model with established risk factors to 0.157 (0.010) in the model with established risk factors and irisin, corresponding to an average decrease of 0.009 (0.001). The NRI statistic showed that the addition of irisin to established risk factors significantly increased the correct reclassification of poor outcome (P = 0.003). In addition, the IDI statistic did not find that irisin level significantly increased the discrimination between patients with poor outcome and good outcome (P = 0.088) (Table 4).
Irisin and Mortality Within 6 Months
After 6 months, 325 patients had died; thus, the mortality rate was 21.2% (95% CI, 19.2%–23.3%). Irisin in patients who survived was significantly higher as compared with patients who died (95.9 [IQR, 71.2–143.5] ng/ml vs. 67.4 [IQR, 58.5–87.9] ng/ml; Z = 12.550; P < 0.001; Fig. 2b). The mortality rate across the irisin quartiles ranged from 39.3% (first quartile) to 6.3% (fourth quartile). The P value for the trend was less than 0.001 (Fig. 3b). In multivariate models comparing Q1, Q2, and Q3 against Q4 of irisin (Table 3), levels of irisin in Q1, Q2, and Q3 were associated with mortality, and the odds ratios were increased by 402% (OR = 5.02; 95% CI, 2.99–8.24), 216% (OR = 3.16; 95% CI, 2.04–4.48), and 59% (1.59; 1.06–2.48), respectively. The independent association of irisin with poor outcome was confirmed using the likelihood ratio test (P = 0.002). In a multivariate model using Q1 of irisin vs. Q2–Q4 together with the clinical variables, the marker displayed prognostic information and increased the odds ratio by 185% (OR for Q1, 2.85 [95% CI, 1.79–4.02]).
With an AUC of 0.76 (95% CI, 0.70–0.82; Fig. 4b), irisin had a higher prognostic accuracy as compared to FBG [AUC, 0.62 (95% CI, 0.57–0.69); P < 0.001], Hs-CRP [AUC, 0.67 (0.61–0.73); P = 0.001], HCY [AUC, 0.60 (0.55–0.65); P < 0.001], IL-6 [AUC, 0.65 (95% CI, 0.59–0.70); P < 0.001], and NIHSS [AUC, 0.73 (95% CI, 0.68–0.79); P = 0.039]. The combined model (irisin/NIHSS) could improve the NIHSS score [AUC of the combined model, 0.79 (95% CI, 0.73–0.84), P = 0.008]. A significant difference in the AUC between the established risk factors alone and the addition of irisin concentrations was observed (difference, 0.03 [95% CI, 0.02–0.04]; P = 0.019) (Table 4). This improvement was stable in an internal fivefold cross-validation that resulted in an average AUC of 0.80 (0.027) for the established risk factors and 0.83 (0.024) for the combined model, corresponding to a difference of 0.03 (0.012). Improvement in the fitted values of the predictive probabilities for fivefold cross-validated Brier’s score was 0.066 (0.007) for the established risk factors with irisin as compared with 0.070 (0.010) for the established risk factors only. This corresponds to an average decrease of 0.004 (0.004). The NRI statistic showed that the addition of irisin to established risk factors significantly increased the correct reclassification of mortality (P < 0.001). In addition, the IDI statistic found that irisin level significantly increased the discrimination between survivors and non-survivors (P = 0.011) (Table 4).
Discussion
To the best of our knowledge, this multicenter study is the first report to investigate the prognostic potential of irisin in a substantial cohort of stroke patients. Data confirms evidence linking lower circulating irisin concentrations with signs of poor functional outcome in stroke and adds significant additional predictive information to the clinical score of the NIHSS.
A previous observation suggested that high circulating irisin levels were associated with an increased 10-year risk of cardiovascular diseases [19]. However, another study reported that low serum irisin level was an independent predictor of coronary artery severity in patients with stable coronary artery disease [20]. Conversely, Shen et al. [21] identified high serum irisin as a predictive biomarker for 1-year all-cause mortality in acute heart failure patients. In our study, the results showed that the reduced serum concentration of irisin was a useful prognostic marker of functional outcome and mortality in Chinese patients with stroke independent of established conventional risk factors. Differences in study design, methodologies used to assess irisin, and included patients make comparison between the present study and previous studies difficult. It should be noted that previous studies [13, 19,20,21] were often with small samples (less than 200) and at single sites, while the present study was a multicenter study with a large sample size (N = 1530).
In addition, since the discovery of irisin, its levels have been associated with hip fractures [22], sarcopenia [23], insulin resistance [24], chronic obstructive pulmonary disease [25], chronic kidney disease (CKD) [26], and CKD stage [27]. Furthermore, irisin-encoding gene (FNDC5) variant can change blood pressure in men with type 2 diabetes [28], while irisin improves endothelial function in type 2 diabetes [29] and in a mouse model of obesity [30]. In addition, irisin protects against endothelial injury and ameliorates atherosclerosis in Apo-E knockout mice [31].
The underlying mechanisms linking irisin with stroke outcome are not clearly illustrated in previous studies. First, a possible explanation is the interplay with other myokines, adipocytokines, or classical cytokines [32]. In this study, we also found that irisin was inversely correlated with HCY, Hs-CRP, and IL-6. However, irisin remained significantly associated with poor outcome even after adjustment for HCY, Hs-CRP, or IL-6, suggesting that the effect of irisin on outcome was independent of inflammation or HCY. Second, previous studies suggest that irisin has an essential role in glucose utilization and lipid metabolism [33, 34]. A study indicates that FNDC5/irisin ameliorates glucose/lipid metabolic abnormalities and insulin resistance in obese mice and enhances lipolysis via cAMP–PKA–HSL/perilipin pathway [35]. In fact, previous studies showed that admission glucose level (AGL) [36] is associated with poor clinical outcome in stroke, and elevated triglyceride/HDL-C ratio is related to risk of recurrent stroke [37]. Third, decreased circulating plasma levels of irisin seem to be associated with flow-mediated dilation (FMD) levels in patients with type 2 diabetes [38]. Impaired FMD in patients with acute ischemic stroke is associated with poor outcome [39]. Fourth, lower levels of irisin are independently associated with endothelial dysfunction [40]. Irisin alleviates endothelial dysfunction in type 2 diabetes partially via reducing oxidative/nitrative stresses through inhibiting signaling pathways implicating PKC-β/NADPH oxidase and NF-κB/iNOS [29]. Targonski et al. [41] reported that the presence of endothelial dysfunction was independently associated with an increased risk of cerebrovascular events. Lastly, irisin reduces ischemia-induced neuronal injury via activation of the Akt and ERK1/2 signaling pathways and contributes to the neuroprotective effect of physical exercise against cerebral ischemia [42]. Additional observations suggest that irisin produces protective effects against hypoxia/reoxygenation injury, which is dependent upon HDAC4 [43]. Hence, further studies should explore the molecular mechanism to elucidate direct irisin effects. Furthermore, future studies regarding the interaction between irisin and other myokines/adipocytokines might be helpful to allow a better understanding of irisin.
Strengths and Limitations
Our study is the first analysis of serial serum measurements of irisin in Han Chinese patients with stroke in a multicenter setting. Second, we collected data on a wide range of potentially confounding risk factors, allowing us to estimate the independent effect of irisin. Third, serum levels of irisin were tested by ELISA. This method is cost-efficient (less than 10 dollars per test) and is non-invasive. Lastly, we chose a different strategy using the fourth quartile, because we have found this strategy to be more sensitive to other factors that might influence the relatively low concentrations.
The following limitations of our study must be taken into account. First, data on potential confounding factors, including dietary intake, and outdoor physical activity, were not obtained. Second, there is an evidence that irisin may favorably influence stroke outcome through multiple pathways, including insulin resistance, diabetes, hypertension, and chronic inflammation. The inclusion of those factors in the models could possibly lead to over-adjustment, which tends to attenuate the associations. Third, irisin is usually measured by ELISA, but the quantification varies greatly among kits. These differences likely stem from the various irisin epitopes being targeted for measurement by the manufacturing companies. Fourth, the observational nature of the study precludes us to draw any conclusion on the role of irisin in the development of poor outcome and, therefore, no conclusion regarding cause–effect relationships can be made. In addition, this study is an association study between irisin and stroke outcome. It is currently unknown whether irisin tested at admission can influence risk-optimized therapeutic strategies. Additional randomized controlled trials are, therefore, urgently needed to evaluate whether the addition of irisin concentration to prediction modeling increases the accuracy enough to make its addition useful in a clinical setting. Finally, all participants of the present study were Han Chinese, and whether these observations can also be extended to other ethnic groups remains to be determined. In addition, the estimated amount of improvement gained by adding irisin to the multivariate model was small. The impact on practice needs further confirmation by large-scale multicenter studies.
In conclusion, irisin is a novel, independent prognostic marker improving currently used risk stratification of stroke patients. Further studies are needed to confirm this association, which may pave the way to new therapeutic options.
References
Boström P, Wu J, Jedrychowski MP, Korde A, Ye L, Lo JC, et al. A PGC1-a-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 2012; 481:463–468.
Huh J Y, Mougios V, Kabasakalis A, et al. Exercise-induced irisin secretion is independent of age or fitness level and increased irisin may directly modulate muscle metabolism through AMPK activation. The Journal of Clinical Endocrinology & Metabolism, 2014, 99(11): E2154–E2161.
Aydin S, Aydin S. Irisin Concentrations as a Myocardial Biomarker. Biomarkers in Cardiovascular Disease, 2016: 489–504.
Ferrer-Martínez A, Ruiz-Lozano P, Chien KR. Mouse PeP: a novel peroxisomal protein linked to myoblast differentiation and development. Dev Dyn. 2002; 224:154–167.
Panagiotou G, Mu L, Na B, et al. Circulating irisin, omentin-1, and lipoprotein subparticles in adults at higher cardiovascular risk. Metabolism, 2014, 63(10): 1265–1271.
Moreno-Navarrete JM, Ortega F, Serrano M, Guerra E, Pardo G, Tinahones F, et al. Irisin is expressed and produced by human muscle and adipose tissue in association with obesity and insulin resistance. J Clin Endocrinol Metab 2013;98: E769–778.
Crujeiras AB, Zulet MA, Lopez-Legarrea P, de la Iglesia R, Pardo M, Carreira MC, et al. Association between circulating irisin levels and the promotion of insulin resistance during the weight maintenance period after a dietary weight-lowering programin obese patients. Metabolism 2014; 63:520–31.
Choi YK, Kim MK, Bae KH, Seo HA, Jeong JY, Lee WK, et al. Serum irisin levels in new-onset type 2 diabetes. Diabetes Res Clin Pract 2013; 100:96–101.
Jang H B, Kim H J, Kang J H, et al. Association of circulating irisin levels with metabolic and metabolite profiles of Korean adolescents. Metabolism, 2017; 73:100–108
Wang S, Pan J. Irisin ameliorates depressive-like behaviors in rats by regulating energy metabolism. Biochemical and Biophysical Research Communications, 2016, 474(1): 22–28.
Kuloglu T, Aydin S, Eren MN, et al. Irisin: a potentially candidate marker for myocardial infarction. Peptides. 2014; 55:85–91.
Endres M, Gertz K, Lindauer U, et al. Mechanisms of stroke protection by physical activity [J]. Annals of Neurology, 2003, 54(5): 582–590.
Aronis K N, Moreno M, Polyzos S A, et al. Circulating irisin levels and coronary heart disease: association with future acute coronary syndrome and major adverse cardiovascular events [J]. International Journal of Obesity, 2015, 39(1): 156–162.
Tu W J, Qiu H C, Liu Q, et al. Decreased level of irisin, a skeletal muscle cell-derived myokine, is associated with post-stroke depression in the ischemic stroke population [J]. Journal of Neuroinflammation, 2018, 15(1): 133.
Sims, JR, Gharai, LR, Schaefer, PW, Vangel M, Rosenthal ES. ABC/2 for rapid clinical estimate of infarct, perfusion, and mismatch volumes. Neurology 2009; 72: 2104–2110.
Bonita R BR. Modification of Rankin Scale: recovery of motor function after stroke. Stroke 1988; 19: 1497–1500.
Tu W J, Zeng X W, Deng A, et al. Circulating FABP4 (Fatty Acid–Binding Protein 4) Is a Novel Prognostic Biomarker in Patients with Acute Ischemic Stroke. Stroke, 2017; 48:1531–1538.
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 2008; 27:157–172.
Park KH, Zaichenko L, Brinkoetter M, Thakkar B, Sahin-Efe A, Joung KE, et al. Circulating irisin in relation to insulin resistance and the metabolic syndrome. J Clin Endocrinol Metab 2013;98:4899–4907
Efe T H, Açar B, Ertem A G, et al. Serum irisin level can predict the severity of coronary artery disease in patients with stable angina [J]. Korean Circulation Journal, 2017, 47(1): 44–49.
Shen S, Gao R, Bei Y, et al. Serum Irisin Predicts Mortality Risk in Acute Heart Failure Patients [J]. Cellular Physiology and Biochemistry, 2017; 42(2): 615–622.
Yan J, Liu H J, Guo W C, et al. Low serum concentrations of Irisin are associated with increased risk of hip fracture in Chinese older women [J]. Joint Bone Spine 2018; 85(3): 353–358.
Chang JS, Kim TH, Nguyen TT, et al. Circulating irisin levels as a predictive biomarker for sarcopenia: A cross-sectional community-based study [J]. Geriatrics & Gerontology International, 2017; 17(11): 2266–2273.
Liu B W, Yin F Z, Qi X M, et al. The Levels of Serum Irisin as a Predictor of Insulin Resistance in Han Chinese Adults with Metabolically Healthy Obesity [J]. Clinical Laboratory, 2017, 63(5–6): 881–886.
Sugiyama Y, Asai K, Yamada K, et al. Decreased levels of irisin, a skeletal muscle cell-derived myokine, are related to emphysema associated with chronic obstructive pulmonary disease [J]. International Journal of Chronic Obstructive Pulmonary Disease, 2017, 12: 765–772.
Yang S, Xiao F, Pan L, et al. Association of serum irisin and body composition with chronic kidney disease in obese Chinese adults: a cross-sectional study. BMC Nephrology, 2015, 16(1): 16.
Ebert T, Focke D, Petroff D, et al. Serum levels of the myokine irisin in relation to metabolic and renal function [J]. European Journal of Endocrinology, 2014, 170(4): 501–506.
Brondani LA, Boelter G, Assmann TS, Leitao CB, Canani LH, Crispim D. Irisin-encoding gene (FNDC5) variant is associated with changes in blood pressure and lipid profile in type 2 diabetic women but not in men. Metabolism 2015; 64:952–957.
Zhu D, Wang H, Zhang J, Zhang X, Xin C, Zhang F, et al. Irisin improves endothelial function in type 2 diabetes through reducing oxidative/nitrative stresses. J Mol Cell Cardiol 2015; 87:138–147.
Han F, Zhang S, Hou N, Wang D, Sun X. Irisin improves endothelial function in obese mice through the AMPK-eNOS pathway. Am J Physiol Heart Circ Physiol 2015;309:H1501–H1508.
Lu J, Xiang G, Liu M, Mei W, Xiang L, Dong J. Irisin protects against endothelial injury and ameliorates atherosclerosis in apolipoprotein E-null diabetic mice. Atherosclerosis 2015; 243:438–448.
Polyzos S A, Kountouras J, Shields K, et al. Irisin: a renaissance in metabolism? [J]. Metabolism-Clinical and Experimental, 2013, 62(8): 1037–1044.
Iglesia R, Lopez-Legarrea P, Crujeiras A B, et al. Plasma irisin depletion under energy restriction is associated with improvements in lipid profile in metabolic syndrome patients [J]. Clinical Endocrinology, 2014, 81(2): 306–311.
Xin C, Liu J, Zhang J, et al. Irisin improves fatty acid oxidation and glucose utilization in type 2 diabetes by regulating the AMPK signaling pathway [J]. International Journal of Obesity, 2016, 40(3): 443–451.
Xiong X Q, Chen D, Sun H J, et al. FNDC5 overexpression and irisin ameliorate glucose/lipid metabolic derangements and enhance lipolysis in obesity [J]. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease, 2015, 1852(9): 1867–1875.
Desilles J P, Meseguer E, Labreuche J, et al. Diabetes Mellitus, Admission Glucose, and Outcomes After Stroke Thrombolysis [J]. Stroke, 2013, 44(7): 1915–1923.
Park J H, Lee J, Ovbiagele B. Nontraditional serum lipid variables and recurrent stroke risk [J]. Stroke, 2014, 45(11): 3269–3274.
Wang H, Zhang X, Chen W, et al. Relationship between serum irisin levels and urinary albumin excretion in patients with type 2 diabetes. Journal of Diabetes and Its Complications, 2015, 29(3): 384–389.
Santos-García D, Blanco M, Serena J, et al. Brachial arterial flow mediated dilation in acute ischemic stroke [J]. European Journal of Neurology, 2009, 16(6): 684–690.
Hou N, Han F, Sun X. The relationship between circulating irisin levels and endothelial function in lean and obese subjects. Clinical Endocrinology, 2015, 83(3): 339–343.
Targonski P V, Bonetti P O, Pumper G M, et al. Coronary endothelial dysfunction is associated with an increased risk of cerebrovascular events [J]. Circulation, 2003, 107(22): 2805–2809.
Li D J, Li Y H, Yuan H B, et al. The novel exercise-induced hormone irisin protects against neuronal injury via activation of the Akt and ERK1/2 signaling pathways and contributes to the neuroprotection of physical exercise in cerebral ischemia [J]. Metabolism, 2017, 68: 31–42.
Zhao Y T, Du J, Wang H, et al. Irisin Protects Against Hypoxia and Reoxygenation Injury Through Hdac4 [J]. Circulation. 2016; 134: A17980
Acknowledgements
All authors have contributed significantly and are in agreement with the content of the manuscript. We are grateful to the Department of Neurology and the Emergency Department; the nurses, physicians, and patients who participated in our study; and the staff of the central laboratory of the hospitals. We also thank Pro Shao-Gong Fang (Weifang Medical College) for the statistical advice and assistance with the qualitative measures used in this study.
Funding
This study was supported by grants from the Shandong Province Science and Technology Development Plan Project (No. 2015GGB14296), Shandong Province Key Research and Development Projects (No. 2016GSF201229), National Natural Science Foundation of China (Nos. 81671175 and 81602800), and CAMS Innovation Fund for Medical Science (No. 2017-I2M-1-021).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Role of the Sponsor
The funding organizations had no role in the design and concept of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
Ethics, Consent, and Permissions
Written informed consents were obtained from all patients. This study conformed with the principles of the Declaration of Helsinki and was approved by the investigational review board of the Weifang Medical University (Trial registration: ChiCTR-OPC-17013501; retrospectively registered on 23 September 2017).
Rights and permissions
About this article
Cite this article
Tu, WJ., Qiu, HC., Cao, JL. et al. Decreased Concentration of Irisin Is Associated with Poor Functional Outcome in Ischemic Stroke. Neurotherapeutics 15, 1158–1167 (2018). https://doi.org/10.1007/s13311-018-0651-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-018-0651-2