Summary
Machado-Joseph disease, also called spinocerebellar ataxia type 3 (MJD/SCA3), is a hereditary and neurodegenerative movement disorder caused by ataxin-3 with a pathological polyglutamine stretch (mutant ataxin-3). Seven transgenic mouse models expressing full-length human mutant ataxin-3 throughout the brain have been generated and are compared in this review. They vary in the corresponding transgenic DNA constructs with differences that include the encoded human ataxin-3 isoform(s), number of polyglutamine(s), and the promoter driving transgene expression. The behaviors/signs evaluated in most models are body weight, balance/coordination, locomotor activity, gait, limb position, and age at death. The pathology analyzed includes presence of neuronal intranuclear inclusions, and qualitative evidence of neurodegeneration. On the basis of striking similarities in age-range of detection and number of behavior/sign abnormalities and pathology, all but 1 mouse model could be readily sorted into groups with high, intermediate, and low severity of phenotype. Stereological analysis of neurodegeneration was performed in the same brain regions in 2 mouse models; the corresponding results are consistent with the classification of the mouse models.
Similar content being viewed by others
Introduction
Machado-Joseph disease (MJD), also called spinocerebellar ataxia type 3 (SCA3), was described between 1972 and 1995, and it has been given 10 different names: 1) Machado disease [1]; 2) nigro-spino-dentatal degeneration with nuclear ophthalmoplegia [2]; 3) autosomal dominant striatonigral degeneration [3]; 4) Azorean disease of the nervous system [4]; 5) autosomal dominant system degeneration [5]; 6) Joseph disease [6]; 7) autosomal dominant motor system degeneration [7]; 8) MJD disease [8, 9]; 9) Machado-Joseph Azorean disease [10]; and 10) SCA3 [11]. Finally, SCA3 was found to be genetically identical to MJD [12]. MJD/SCA3 is the most prevalent spinocerebellar ataxia in many countries worldwide (for more detail see Bettencourt and Lima [13]).
MJD/SCA3 is an autosomal, dominantly inherited neurodegenerative disorder. It is caused by ataxin-3, with a stretch of 45 to 86 consecutive glutamines (mutant ataxin-3), whereas normal ataxin-3 has fewer than 44 [14–16]; the polyglutamine stretch is encoded by cytosine-adenine-guanine (CAG) repeats in the corresponding MJD1 (also named ATXN3) gene [14]. Several ataxin-3 isoforms are reported, including MJD1a (also named ataxin 3a) and ataxin 3c (also named MJD1-1), which differ in the last 17 to 30 amino acids, respectively. They result from alternative splicing and have been detected with extended polyglutamines in the brains of MJD/SCA3 patients [14, 17, 18]. Mutant ataxin-3 expression is widespread, even though neurodegeneration is selective [19]. Polyglutamine diseases also encompass other spinocerebellar ataxias, Huntington’s disease, spinal and bulbar muscular atrophy, and dentatorubral-pallidoluysian atrophy. All polyglutamine diseases present an inverse correlation between CAG repeat length encoding the polyglutamine stretch and age of onset. Intergenerational CAG repeats expansion results in a more severe phenotype in the offspring than the parent (anticipation). The pathological polyglutamine stretch confers a toxic gain of function to the disease protein, by altering its conformation, its interaction with other proteins, and forming ubiquitinated intranuclear inclusions in neurons (for more detail see Ross [20] and La Spada and Taylor [21]).
MJD/SCA3 is clinically heterogeneous, even between patients within any given family (for more detail see Bettencourt and Lima [13] and Riess et al. [22]. The major signs are progressive and include: a) cerebellar dysfunctions, which involve inaccurate voluntary movements, such as gait and limb ataxia, action and trunk tremor, and speech difficulty (dysarthria); and b) pyramidal signs, which involve increased reflexes (Babinski sign) and muscle tone (spasticity) in the legs more than the arms. Minor signs, but more specific, than to other spinocerebellar ataxia, are “bulging eyes” due to oculomotor dysfunction causing eyelid retraction, and motor neuron signs resulting in facial and lingual fasciculations. Five subtypes of MJD/SCA3 are proposed, based on the variability of clinical signs. Not all patients fit this classification and a patient may begin 1 type and evolve into another. Type I: early age of onset, major/minor signs, although pyramidal signs are more prominent than cerebellar signs, extrapyramidal signs (disturbed posture [dystonia], slow movement [bradikinesia]), and premature death. Type II: intermediate age of onset, and major/minor signs. Type III: later age of onset, major/minor signs, although cerebellar signs are more prominent than pyramidal signs, peripheral signs, and no premature death. Peripheral nerve signs include muscle atrophy (motor), distal sensation loss (sensory), and thermoregulatory and urinary system dysfunctions (autonomic). Pyramidal signs (upper motor neuron) in type III might be obscured by lower motor neuron degeneration. Type IV: variable onset, neuropathy and parkinsonism (paucity of movement or akinesia, and muscular rigidity). Type V: spastic paraplegia alone. Sleep disorders and/or depression can occur, and weight loss without loss of appetite. At the end stage, patients undergo cachexia and pulmonary complications. Genetic factors contribute to such clinical variability. The CAG repeat length is longest in type I, intermediate in type II, and shortest in type III patients. Type IV and V are caused by unidentified familial factors, not CAG repeat dependent. To the author’s knowledge, clinical variability has not been associated with different ataxin-3 isoforms.
MJD/SCA3 pathology includes severe neuronal loss in spinal cord and brain regions, such as dentate nuclei (cerebellum), pontine nuclei (brainstem), substantia nigra (basal ganglia), and to a lesser degree, cerebellar cortex [15] (for more detail see Rub et al. [23]). Recent studies suggest that degeneration is more widespread and might include striatum [24], Purkinje cells in the cerebellum [25], and cerebral cortex (for more detail see Rub et al. [23]). Based on pathoanatomical studies [23], it is proposed that the central nervous loops and systems affected include: 1) cerebellothalamocortical motor loop causing cerebellar signs, pyramidal signs, and some of the motor peripheral signs; 2) basal ganglia-thalamocortical motor loop causing ataxia and extrapyramidal signs; 3) somatosensory system causing autonomic and sensory peripheral nerve loss; 4) vestibular system causing impaired body balance (postural instability), and related eye movements (eye jumps or nystagmus, and vestibulo-ocular reaction); 5) oculomotor system causing “bulging eyes,” vision problems (double vision or diplopia), slow eye movements (ophthalmoplegia); and 6) midbrain dopaminergic system causing parkinsonian features. Intranuclear inclusions were detected initially in affected neurons of patients [17, 26], but subsequently they were observed in less affected brain regions [27]. Their reactivity with different antibodies revealed cellular proteins associated with toxicity [26]. Therefore, neuronal inclusions are considered markers of pathogenesis.
There is no treatment currently available to cure or delay the onset of MJD/SCA3. Generation and characterization of transgenic mice expressing mutant ataxin-3 are providing insight into the mechanisms causing the disease and facilitating the development of a therapy. Transgenic mice expressing portions of the mutant ataxin-3 age [28–30], and a lentiviral-based rat model expressing mutant ataxin-3 in a single brain region [24] have been reported, but these are not the focus of this review. Seven transgenic mice expressing full-length mutant ataxin-3 throughout the brain have been reported and are described as dramatically different in previous reviews [31]. In this review, the behavior/signs and pathology of a representative mouse line for each of the 7 transgenic mice are compared. On the basis of striking similarities, the mouse models are sorted into groups of high, intermediate, or low phenotype severity.
Mouse Models
Eight transgenic mice expressing full-length human mutant ataxin-3 have been reported. The first transgenic mouse that expressed full-length mutant ataxin-3 isoform MJD1a with 79 polyglutamines under control of the L7 promoter (Purkinje cell specific) failed to develop neurological deterioration at 23 weeks of age [28]. By contrast, transgenic mice expressing a portion of such human mutant ataxin-3 containing the expanded polyglutamines and under the control of the same promoter had severe atrophy of the cerebellum, including Purkinje cell loss at 8 weeks of age, and severe ataxic behavior starting at 4 weeks of age [28]. Based on these results and cell model studies, the toxic fragment hypothesis was proposed, in which all cells express full-length mutant ataxin-3 and affected neurons express a protease that releases the toxic fragment [28].
For each of the next 7 transgenic mice generated [32–38]: the transgenic mouse construct, behavior/signs, and pathology are summarized as follows.
Transgenic Construct Used for Each Mouse Model
The 7 transgenic mouse models are numbered to facilitate their description (Table 1, mouse models 1-7). The components of the transgenic constructs used to generate each mouse model are described as follow (Table 1, transgenic construct).
Mouse Model 1
For mouse model 1 [32], the transgenic construct contains the MJD1 gene with 84 or 15 CAG and is flanked at the 5′end by 35 kb and at the 3′end by 150 kb of the SCA3 locus and the arms of the yeast artificial chromosome. All ataxin-3 isoforms (including MJD1a and ataxin-3c) could be synthesized; the human ataxin-3 promoter drives widespread expression (see Introduction for details). The transgenic mice are maintained on a C57BL/6 J genetic background. A representative transgenic mouse line is “MJD84.2”; the control animal “MJD15.4” and wild-type mice were comparable.
Mouse Model 2
For mouse model 2 [33], the transgenic construct used encodes human ataxin-3 isoform MJD1a with 71 or 20 CAG under the control of the mouse prion protein promoter. In the MoPrP.Xho vector, the cDNA was inserted in the Xho I site. At the 5′end of Xho I is 6 kb followed downstream by noncoding exon 1, intron 1, and exon 2 of the prion protein gene. At the 3′ end of Xho I site is 2.2 kb of unstranslated prion protein gene sequence. Expression occurs throughout the brain but is lower in Purkinje cells. The transgenic mice are maintained on a B6C3F1/J genetic background; B6C3F1/J is F1 offspring of C57BL/6J × C3H/HeJ. A representative transgenic mouse is “homozygous Q71C”; the control animal “Q20A” and wild-type mice were comparable.
Mouse Model 3
For mouse model 3 [34], ataxin-3 isoform 3c with 70 or 15 CAG are expressed under the control of the mouse prion protein promoter. The vector MoPrP used has 1.14 kb upstream of exon 1, intron 1, and 52 bp of exon 2. At the 3′ end of insertion site is a SV40 mRNA polyadenylation signal. The transgenic mice were maintained on a C57BL/6N genetic background. A representative transgenic mouse is “70.61”; the control animal “15.1” and wild-type mice were comparable.
Mouse Model 4
For mouse model 4 [35], isoform MJD1a with 79 or 22 CAG with an N-terminal hemagglutinin tag are expressed using the same vector described for model 2. The transgenic mice were maintained on a FVB/N genetic background. A representative transgenic mouse is “ataxin-3-Q79HA”; the control animal “ataxin-3-Q22HA” and wild-type mice were comparable.
Mouse Model 5
For mouse model 5 [36], isoform ataxin-3c with 77 CAG expression is conditional by a tetracycline-off system. Two transgenic constructs were used. The promoter construct contains the hamster prion protein promoter (25 kb followed downstream by exon 1); a promoter mouse line was generated and initially maintained on FVB/N genetic background until interbred to homozygosity [39]. The responder construct contains a tretracycline responsive element followed downstream by a “minimal” CMV promoter, and the cDNA encoding isoform ataxin-3c with 77 CAG. The reporter transgenic mice were maintained on a C57BL/6 genetic background. In double transgenics, the promoter construct synthesizes a tetracycline transactivator that binds the tetracycline-responsive element in the responder construct that activates transcription of ataxin-3 cDNA. To block expression, the mice are treated with doxycycline (a tetracycline derivative) binds the transactivator abolishing its binding to the responder construct. Unexpectedly, expression was more prominent in glial cells than in neurons. A representative transgenic mouse is “PrP/MJD77-het/hom”; wild-type mice were used as control animals.
Mouse Model 6
For mouse model 6 [37], the transgenic construct contains the cDNA encoding isoform ataxin-3c with 148 CAG, a partial rat huntingtin promoter (764 bp: -777 to -14), and a SV40 mRNA polyadenylation signal. Expression is widespread expression. The transgenic mice were maintained on a C57BL/6N genetic background. A representative transgenic mouse is “HDProm-MJD148”; the control animals were wild-type mice.
Mouse Model 7
For mouse model 7 [38], the transgenic construct contains the cDNA encoding isoform ataxin-3c with 94 CAG, a CMV promoter (details were not reported), and a SV40 mRNA polyadenylation signal. Expression is widespread. A representative transgenic mouse is “hemi-CMVMJD94”. The control animals were wild-type mice. The transgenic mice were maintained on a C57BL/6 or FVB/N genetic background; in the latter the intergenerational instability of expanded CAG repeat was lower.
Summary
In summary, (Table 1), the transgenic constructs vary in ataxin-3 isoform encoded, number of CAG repeats, and promoter. All promoters drive expression throughout the brain, but at lower levels in Purkinje cells of models 2 and 4. Mouse model 5 has conditional expression, which is more prominent in glial cells than neurons. The genetic background is different between a few mouse models.
Behavior and Signs Evaluated in Most Mouse Models
The comparison is limited to behavior/signs reported for most models (presented in Table 2; see details as follows): lower body weight, reduced balance and coordination, abnormal gait, locomotor hypoactivity, abnormal limb positions, and premature death. The corresponding signs develop in MJD/SCA3 patients: weight loss, postural instability, gait ataxia, possibly bradykinesia, limb ataxia, and premature death, respectively (see Introduction for details).
Mouse Model 1
Mouse model 1 [32], line 84.2 had: 1) lower body weight: 12 to 22 % at 1 to 5 months of age; 2) reduced balance/coordination: inability to turn on a grid [32], and reduced beam-walking ability at 7.5 to 13 months in another report [40]; 3) abnormal gait: wide-based limbs at 1 month [32], and shorter stride-alternated footprint pattern at 13.5 months, as described in another report [40]; 4) locomotor hypoactivity: described as inactivity; 5) abnormal limb position when held by tail: forelimb clasping at 6 months, and all limb clasping at 14 months (instead of normal escape reflexes, which is limb spreading); and 6) premature death: not reported, but could not have occurred before 13.5 months because tests were done on animals at this age.
Mouse Model 2
Mouse model 2 [33], homozygous Q71C had: 1) low body weight: 41 % at 2.5 months and 50 % at 3.5 months; 2) reduced balance and coordination: short latency on rotarod test at 1.75 months and zero latency at 2.75 months; 3) abnormal gait: wide-based footprint pattern at 2 to 3 months and dragged to scribbled footprint pattern at 3 to 5 months; 4) locomotor hypoactivity: progressive from mild to severe between ages 1.75 to 5 months, as determined by an open field test; 5) abnormal limb position: progressive feet clutching and limb extension in resting position from 2 to 5 months; and 6) premature death: occurred at 3 to 5 months of age.
Mouse Model 3
Mouse model 3 [34], line 70.61 had: 1) low body weight: the animals were described as small; 2) reduced balance and coordination: inability to grab a pen and walk on it at 6 to 8 months; 3) abnormal gait: wide-based footprint pattern at 3 months, and dragged footprint pattern at 6 months; 4) locomotor hypoactivity: progressive by open field test from 6 to 8 months; 5) abnormal limb position when held by tail: limb clasping from 6 to 8 months; and 6) premature death: was reported within 4 to 6 months, however, behavioral tests were performed on animals 8 months of age. The age at death, thus, is presumably 4 to 8 months.
Mouse Model 4
Mouse model 4 [35], line ataxin-3-Q79HA had: 1) low body weight: 20 to 34 % at 2 to 12 months; 2) reduced balance and coordination: short latency on rotarod test at 7 to 8 months; 3) abnormal gait: wide based footprint pattern at 7 to 8 months, and dragged footprint pattern at 11 to 12 months; 4) locomotor hypoactivity: by open field test at 8 months; 5) abnormal limb position when held by tail: forelimb clasping at 6 months; and 6) premature death: not reported, but could not have occurred before 12 months because tests were performed on animals at this age.
Mouse Model 5
Mouse model 5 [36], line PrP/MJD77-het/hom had: 1) low body weight: 7 %, 17 %, 13 % at 2.25, 6, and 13 months, respectively; 2) reduced balance and coordination: short latency on rotarod test at 2.25 to 13 months, and inability to grab a pen and walk on it at 6 months; 3) abnormal gait: dragged footprint pattern at 20 months; 4) locomotor hypoactivity: not reported; instead, hyperactivity was observed by open field test at 6 months; 5) abnormal limb position when held by tail: limb clasping at 2.25 and 6 months of age; 6) premature death: not reported but could not have occurred before 20 months because tests were done on animals at this age. When switching off expression at an early age, the abnormal signs were reversed.
Mouse Model 6
Mouse model 6 [37], line HDProm-MJD148 had: 1) low body weight was not reported; 2) reduced balance and coordination: short latency on rotarod test at 14.2 to 17 months; 3) abnormal gait was not reported; 4) locomotor hypoactivity: followed the hyperactivity observed by home cage activity and the open field test at 4 to 14 months; 5) abnormal limb position: not reported; 6) premature death: not reported, but could not have occurred before 17 months because tests were done on animals at this age.
Mouse Model 7
Mouse model 7 [38], Hemi-CMVMJD94 had: 1) low body weight was not reported; 2) reduced balance and coordination: short latency on rotarod test at 4 to 21 months; 3) abnormal gait: not reported; instead, a normal footprint pattern was reported at 18 and 21 months; 4) locomotor hypoactivity: reported as not statistically significant; 5) abnormal limb position: not reported; 6) premature death; not reported, but could not have occurred before 21 months because tests were done on animals at this age.
Summary
In summary, 6 specific behaviors/signs were analyzed in most mouse models. Their presence, absence, and age of occurrence were used to evaluate the severity of behaviors/signs (Table 2, last column). Mouse model 5 was not included in any group (see Discussion for details).
Pathology Evaluated in Most Mouse Models
The pathology evaluated in each mouse model were varied, thus, the comparison is limited to those reported in most models. They are presented in Table 3 and detailed as follows.
Mouse Model 1
Mouse model 1 [32], line 84.2: 1) Intranuclear inclusions in neurons: detected in pontine and dentate nuclei. It is unclear if substantia nigra was analyzed. They were not detected in cerebellar cortex, hippocampus, striatum, or glial cells, and rarely in Purkinje cells. 2) Neurodegeneration: a) Decrease in number of neurons stained with a dye or antibody at 12 months, by use of an unspecified quantification method and hematoxylin and eosin- and Holmes silver-stained brain sections, 30 % fewer pontine and 40 % fewer dentate neurons were seen. Ten percent fewer calbindin immunostained Purkinje cells; Purkinje cell loss was marked by the observation of empty baskets. At 13.5 months, another report [40] had indicated the use of stereology analysis to show 14 % fewer neurons immunostained for neuronal-specific nuclear protein (NeuN) in pontine nuclei, and 14 % fewer tyrosine-hydroxylase-positive neurons in substantia nigra. b) increased number of glial cells immunostained for the glial fibrillary acidic protein (GFAP): at 12 months, dentate nuclei had increased GFAP staining with a few reactive astrocytes attributed to neuronal loss and indicative of gliosis. Reactive astrocytes were also reported in cerebellar white matter. c) Abnormal morphology of neurons: at 12 months, hematoxylin and eosin- and Holmes silver-stained pons had degenerating neurons described as “hyperchromatic and shrunken scattered dark cells with pyknotic or small nuclei and eosinophilic cytoplasm. Calbindin immunostained Purkinje cells had shrinkage, cell body displacement, and dendritic atrophy.”
Mouse Model 2
Mouse model 2 [33], homozygous Q71C: 1) Intranuclear inclusions in neurons: larger in size (i.e., the size of nucleolus or larger) and number in pons, cerebellar nuclei, substantia nigra, olfactory bulb, and spinal cord (motor and sensory neurons). They were smaller and scarce in other brain regions on the midsagittal plane, including the frontal cortex, hippocampus, thalamus, and cerebellar cortex. At a later stage, few large inclusions were detected in the thalamus and cerebellar cortex. None were detected in glial cells. 2) Neurodegeneration: a) decrease in number of neurons stained with a dye or antibody: at 2 to 2.75 months, by use of unbiased stereology, the total number of tyrosine hydroxylase (TH)-positive neurons in substantia nigra of homozygous Q71-C was 38 % lower than in control Q20-A transgenic mice. By analysis of variance, this reduction was statistically significant. No significant differences were found in the total number of Nissl-stained neurons in the dentate nucleus of homozygous Q71-C compared to controls, in brain sections stained with cresyl violet. Nevertheless, a tendency to a decrease in number was observed in homozygous Q71C, suggesting that a larger number of animals should be analyzed. b) Increase in number of glial cells immunostained for GFAP: not obvious, although stained cells were not quantified using stereology. c) Abnormal morphology of neurons: not determined.
Mouse Model 3
Mouse model 3 [34], line 70.61: 1) Intranuclear inclusions in neurons: detected in cerebellar nuclei, pons, granular layer of cerebellum, hippocampus, and cerebral cortex, but not in Purkinje cells. Indeed, it was reported that such inclusions were found in almost all brain regions analyzed. Size differences, however, were not evaluated; the inclusions shown in the report appear to have size differences. 2) Neurodegeneration: a) Decrease in number of neurons stained with a dye or antibody: at 4 months, in cerebellar sections immunostained with an antibody to phosphorylated neurofilaments revealed condensed or empty baskets around Purkinje cells indicative of Purkinje cell loss. b) Increase in number of glial cells immunostained for GFAP: not reported. c) Abnormal morphology of neurons: at 3 months, electron microscopy analysis showed 50 to 80 % Purkinje cell shrinkage, as described by authors, with “increased electron density of the cytoplasm and the karyoplasm and irregular shape of the cytoplasm and nucleus. Such shrinkage was distinguished from necrosis or apoptosis, and the nucleus was pyknotic.”
Mouse Model 4
Mouse model 4 [35], line ataxin-3-Q79HA: 1) Intranuclear inclusions in neurons: at 10 to 12 months, neuronal inclusions were detected in pons, dentate nuclei, and substantia nigra. It is not clear whether other brain regions were analyzed. 2) Neurodegeneration: a) a decrease in numbers of neurons stained with a dye or antibody: at 10 to 11 months, a nonsignificant decrease in the number of neurons in cerebellar dentate nucleus, molecular, granular, and Purkinje cell layers were observed in hematoxylin and eosin staining and immunostaining of neuronal-specific nuclear protein (NeuN) or calbindin. b) Increase in number of glial cells immunostained for GFAP: not reported. c) Abnormal morphology of neurons: at 11 months, calbindin staining revealed Purkinje cells with shrunken cell body and less dendritic arborization that is considered typical of degeneration.
Mouse Model 5
Mouse model 5 [36], line PrP/MJD77-het/hom: 1) Intranuclear inclusions in neurons: at 1, 12, and 20 months, neuronal intranuclear inclusions were shown in cerebral cortex; they are atypical because they did not increase in size with age. Neuronal inclusions were not reported in any other brain region, including pons, cerebellar nuclei, and substantia nigra. 2) neurodegeneration: a) decrease in numbers of neurons stained with a dye or antibody: not reported. b) Increase in number of glial cells immunostained for GFAP: not reported. c) Abnormal morphology of neurons: at 20 months, by electron microscopy, Purkinje cells were darkly stained as a result of higher electron density that is considered “dark cell degeneration.” Turning off transgene expression at an early disease stage, reversed the previously mentioned pathology. Whether the atypical inclusions were no longer stained was not shown.
Mouse Model 6
Mouse model 6 [37], line HDProm-MJD148: 1) intranuclear inclusions in neurons: at 25 months (18 months in homozygous), intranuclear inclusions were detected in neurons in pons, cerebellar nuclei, and other selective brain regions, including red nucleus, Purkinje cells. It is not clear whether substantia nigra was analyzed. 2) Neurodegeneration: a) decrease in number of neurons stained with a dye or antibody: not reported. b) Increase in number of glial cells immunostained for GFAP: not reported. c) Abnormal morphology of neurons: at 25 months by electron microscopy, Purkinje cells appeared darkly stained (dark cell degeneration).
Mouse Model 7
Mouse model 7 [38], hemi-CMVMJD94: 1) Intranuclear inclusions in neurons: at 12 months, no neuronal intranuclear inclusions were detected. 2) Neurodegeneration: a) decrease in number of neurons stained with a dye or antibody: not reported. b) Increase in number of glial cells immunostained for GFAP: at 12.25 months, stereological analysis of GFAP-positive cells revealed an increase of reactive astrocytes in selective brain regions, including substantia nigra and vestibular nuclei. Increased astocyte number is associated with neuronal death. c) Abnormal morphology of neurons: at 4 and 12.25 months, hematoxylin and eosin-stained brain sections, as described by authors, “revealed scattered dark, shrunken cells with basophilic cytoplasm” in several regions, including the thalamus, dentate, and pontine nuclei.
Summary
In summary, 2 aspects of pathology were examined in all mouse models (Table 3). Their presence, absence, and age of occurrence were used to evaluate the severity of pathology (Table 3, last column). Mouse model 5 was not included in any group (see Discussion for details).
Discussion
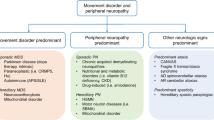
As described, 7 transgenic mice expressing full-length ataxin-3 have been previously reported (mouse models 1-7, Table 1). A representative line from each model is compared in this review (Table 1, last column). The transgenic construct used varied among mouse models (Table 1). Six behaviors/signs, presence of neuronal inclusions and qualitative evidence of neurodegeneration were considered for the comparison (Tables 2 and 3). On the basis of similarities among mouse models, all but model 5 could be readily sorted into groups of high, intermediate, or low severity of phenotype (Tables 2 and 3). Neurodegeneration quantified by stereology has been done in limited brain regions in only a few mouse models, but it is needed to evaluate severity of pathology (Table 4).
Mouse models 2 and 3 (high severity phenotype) express different ataxin-3 isoforms with similar polyglutamine lengths, under the control of the prion protein promoter (Table 1). Both models develop all 6 behavioral abnormalities, including premature death within 1 to 8 months (Table 2). Both models have neuronal inclusions and neurodegeneration within 2 to 4 months (Table 3). Thus, these mouse models have early onset, rapid progression, and premature death that are reminiscent of the most severe type of MJD/SCA3 (type I, see Introduction for details).
Additional information on mouse models 2 and 3:
-
1)
The structural difference between ataxin-3 isoform mjd1a and ataxin-3c are not essential to disease pathogenesis. Mouse models 2 and 3 have a remarkably similar phenotype, even though each express a different isoform of ataxin-3.
-
2)
Mouse models 2 and 3 have prominent neuronal inclusions compared to the intermediate and low models (Table 4), suggesting that pathogenic components are abundant (i.e., more readily detectable than in the intermediate and low severity mouse models). Indeed, a toxic fragment of mutant ataxin-3 was detected in the brain of model 2 [33, 41], and model 3 (V.F. Colomer Gould, unpublished results). This fragment was not detected in non-neuronal tissue in model 2 [42]. Such a fragment was not detected in the brain of mouse models with intermediate (model 1, [32]) or low severity phenotype (model 7, [38]). The fragment is probably present in the brain of intermediate and low severity mouse models, but at levels that are not readily detectable, as observed in the brain of Q71-B heterozygous transgenic mice [33]. The fragment was only detected in an enhanced image of the Western blot.
-
3)
In model 3, a reduced turnover rate of dopamine and serotonin is reported [34], which predictably occurs in model 2.
-
4)
Model 2 is sterile [42], whereas model 3 is reported to be fertile. However, model 3 appears to undergo severe intergenerational CAG repeat instability. The shorter promoter in model 3 and slightly different genetic backgrounds need to be evaluated.
Taken together, the results suggest that models 2 and 3 will facilitate the development of a therapy based on targeting toxic fragment formation, aggregate, or neuronal inclusion formation, dopamine and serotonin turnover rate, and/or delaying premature death. In support of the toxic fragment formation as a target for therapy, a Drosophila model expressing disease ataxin-3 with putative cleavage sites mutated mitigated neurodegeneration [43]. In support of the disease protein aggregation and turnover as targets for therapy, results on mouse model 2 suggest that mutant ataxin-3 forms toxic microaggregates [44]. Normal ataxin-3 is a de-ubiquitinating enzyme [45] that suppresses polyglutamine toxicity by increasing their degradation [46]. It regulates aggresome formation, and degradation of proteins from endoplasmic reticulum [47]. Evidence obtained using material from mouse model 2 suggests that degradation by autophagy is deficient in MJD/SCA3 [48].
Mouse models 1 and 4 (intermediate severity phenotype) were generated using transgenic constructs that differ in the encoded ataxin-3 isoform, polyglutamine length, and promoter controlling expression (Table 1). Neither died prematurely; they developed 5 abnormal behaviors/signs within 1 to 14 months (Table 2). Both models have neuronal inclusions and neurodegeneration within 10 to 12 months (Table 3). The slower progression of disease and absence of premature death compared to the high severity group are reminiscent of a less severe type of MJD/SCA3. These mouse models will facilitate the identifications of events that modulate disease progression, which might lead to therapies that reduce progression rate.
Additional information on mouse models 1 and 4:
-
1)
Model 1 (and predictably model 4) has peripheral neuropathy [32], metabolic abnormalities in cerebellum [49], deranged calcium signaling [40, 50], reduced parkin levels possibly causing parkinsonism [51].
-
2)
Model 4 (and predictable model 1) has transcriptional dysregulation in the cerebellum [35], which is reversible with sodium butyrate [52].
Mouse models 6 and 7 (low severity group) express the same ataxin-3 isoform with different lengths of polyglutamines (148 or 94), and under the control of different promoters (huntingtin or CMV) (Table 1). Both models develop a maximum of 2 of the abnormal behaviors/signs within the age of 4 to 21 months (Table 2). Both models have some evidence of neurodegeneration within 4 to 25 months, but no neuronal inclusions under the age of 12 months. At 25 months, neuronal inclusions were detected in model 6, but were not searched for in model 7. Compared to the mouse models with high and intermediate severity phenotypes, mouse models 6 and 7 have fewer signs, later age of onset, slower progression of disease, and no premature death. They might be reminiscent of a mild type of MJD/SCA3 in patients. As proposed by the authors, these models might be useful to study the early stages of MJD/SCA3.
Additional information on mouse models 6 and 7:
-
1)
Model 6 expresses mutant ataxin-3c with 148 polyglutamines and model 7 expresses mutant ataxin-3c with 94 polyglutamines. One could speculate that the level of expression in model 7 is lower than in model 6, such that the dosage of polyglutamines is comparable causing a similar severity of disease.
-
2)
Hyperactivity precedes hypoactivity. Mouse model 6 (and predictably model 7) develops hyperactivity before hypoactivity (biphasic course of disease) [33]. It remains to be determined whether hyperactivity occurs at an early stage in the other mouse models and MJD/SCA3 patients.
-
3)
Intergenerational CAG repeat instability occurs in both models, and somatic mosaicism in neuronal and non-neuronal cells occurs in model 7 (and predictably model 6).
Mouse model 5 stands out from the rest of the mouse models. It is the only mouse model with conditional transgene expression; it expresses ataxin-3c with 77 polyglutamines under the control of the prion protein promoter (Table 1). It develops 4 abnormal behavior/signs within an age range of 2.25 to 20 months; which is a wider age range than the other mouse models (Table 2). Evidence of neurodegeneration was detected at 20 months, as with the low severity group (Table 3). Neuronal inclusions were only reported in cerebral cortex and did not increase in size with age [32], which is atypical for mutant ataxin-3 neuronal inclusions. In addition, the neuronal inclusions were detected at 1 month, a younger age than any mouse model (Table 3). Such differences between mouse model 5 and the other mouse models probably result from transgene expression being predominant in glial rather than neuronal cells [36]. Mouse model 5 might facilitate understanding the role of glial cells in MJD/SCA3 pathogenesis. As discussed by the authors, their model provides evidence that expression in glial cells causes alterations in Purkinje cells. They also refer to a SCA3 Drosophila model that reveals mutant ataxin-3 toxicity to glial cells [53].
The results on the comparison of each group of mouse models were pooled to highlight the main conclusions (Table 4). The severity of behavior/signs correlates with prominence of neuronal intranuclear inclusions. In the high and intermediate severity group, the percent decrease in number of neurons in substantia nigra correlates with severity of behaviors/signs and prominence of inclusions (Table 4); in the low severity group, indirect evidence of neurodegeneration in substantia nigra was established. By contrast, stereological analysis revealed no significant decrease in the number of neurons in dentate nuclei of a high severity mouse model. The dentate nuclei neurons were stained for nucleic acids (using cresyl violet) whereas substantia nigra neurons were immunostained for a single protein (tyrosine hydroxylase) [33]. The former might reveal neuronal loss and the latter neuronal dysfunction. To avoid such technical issues, the same method should be used to evaluate neurodegeneration. Ideally, the method should have the following characteristics: a) be applicable on all brain regions without changing reagents e.g. antibodies; b) detect neurodegeneration in mouse models with low to high phenotype severity; and c) render results quantifiable by stereological analysis.
References
Nakano KK, Dawson DM, Spence A. Machado disease. A hereditary ataxia in Portuguese emigrants to Massachusetts. Neurology 1972;22:49-55.
Woods BT, Schaumburg HH. Nigro-spino-dentatal degeneration with nuclear ophthalmoplegia. A unique and partially treatable clinico-pathological entity. J Neurol Sci 1972;17:149-166.
Rosenberg RN, Nyhan WL, Bay C, Shore P. Autosomal dominant striatonigral degeneration. A clinical, pathologic, and biochemical study of a new genetic disorder. Neurology 1976;26:703-714.
Romanul FC, Fowler HL, Radvany J, Feldman RG, Feingold M. Azorean disease of the nervous system. N Engl J Med 1977;296:1505-1508.
Coutinho P, Andrade C. Autosomal dominant system degeneration in Portuguese families of the Azores Islands. A new genetic disorder involving cerebellar, pyramidal, extrapyramidal and spinal cord motor functions. Neurology 1978;28:703-709.
Rosenberg RN, Nyhan WL, Coutinho P, Bay C. Joseph’s disease: an autosomal dominant neurological disease in the Portuguese of the United States and the Azores Islands. Adv Neurol 1978;21:33-57.
Healton EB, Brust JC, Kerr DL, Resor S, Penn A. Presumably Azorean disease in a presumably non-Portuguese family. Neurology 1980;30:1084-1089.
Lima L, Coutinho P. Clinical criteria for diagnosis of Machado-Joseph disease: report of a non-Azorena Portuguese family. Neurology 1980;30:319-322.
Barbeau A, Roy M, Cunha L, et al. The natural history of Machado-Joseph disease. An analysis of 138 personally examined cases. Can J Neurol Sci 1984;11:510-525.
Fowler HL. Machado-Joseph-Azorean disease. A ten-year study. Arch Neurol 1984;41:921-925.
Stevanin G, Le Guern E, Ravise N, et al. A third locus for autosomal dominant cerebellar ataxia type I maps to chromosome 14q24.3-qter: evidence for the existence of a fourth locus. Am J Hum Genet 1994;54:11-20.
Matilla T, McCall A, Subramony SH, Zoghbi HY. Molecular and clinical correlations in spinocerebellar ataxia type 3 and Machado-Joseph disease. Ann Neurol 1995;38:68-72.
Bettencourt C, Lima M. Machado-Joseph Disease: from first descriptions to new perspectives. Orphanet J Rare Dis 2011;6:35.
Kawaguchi Y, Okamoto T, Taniwaki M, et al. CAG expansions in a novel gene for Machado-Joseph disease at chromosome 14q32.1. Nat Genet 1994;8:221-228.
Durr A, Stevanin G, Cancel G, et al. Spinocerebellar ataxia 3 and Machado-Joseph disease: clinical, molecular, and neuropathological features. Ann Neurol 1996;39:490-499.
Padiath QS, Srivastava AK, Roy S, Jain S, Brahmachari SK. Identification of a novel 45 repeat unstable allele associated with a disease phenotype at the MJD1/SCA3 locus. Am J Med Genet B Neuropsychiatr Genet 2005;133B:124-126.
Schmidt T, Landwehrmeyer GB, Schmitt I, et al. An isoform of ataxin-3 accumulates in the nucleus of neuronal cells in affected brain regions of SCA3 patients. Brain Pathol 1998;8:669-679.
Goto J, Watanabe M, Ichikawa Y, et al. Machado-Joseph disease gene products carrying different carboxyl termini. Neurosci Res 1997;28:373-377.
Nishiyama K, Murayama S, Goto J, et al. Regional and cellular expression of the Machado-Joseph disease gene in brains of normal and affected individuals. Ann Neurol 1996;40:776-781.
Ross CA. When more is less: pathogenesis of glutamine repeat neurodegenerative diseases. Neuron 1995;15:493-496.
La Spada AR, Taylor JP. Repeat expansion disease: progress and puzzles in disease pathogenesis. Nat Rev Genet 2010;11:247-258.
Riess O, Rub U, Pastore A, Bauer P, Schols L. SCA3: neurological features, pathogenesis and animal models. Cerebellum 2008;7:125-137.
Rub U, Brunt ER, Deller T. New insights into the pathoanatomy of spinocerebellar ataxia type 3 (Machado-Joseph disease). Curr Opin Neurol 2008;21:111-116.
Alves S, Regulier E, Nascimento-Ferreira I, et al. Striatal and nigral pathology in a lentiviral rat model of Machado-Joseph disease. Hum Mol Genet 2008;17:2071-2083.
Munoz E, Rey MJ, Mila M, et al. Intranuclear inclusions, neuronal loss and CAG mosaicism in two patients with Machado-Joseph disease. J Neurol Sci 2002;200:19-25.
Paulson HL, Perez MK, Trottier Y, et al. Intranuclear inclusions of expanded polyglutamine protein in spinocerebellar ataxia type 3. Neuron 1997;19:333-344.
Yamada M, Hayashi S, Tsuji S, Takahashi H. Involvement of the cerebral cortex and autonomic ganglia in Machado-Joseph disease. Acta Neuropathol (Berl) 2001;101:140-144.
Ikeda H, Yamaguchi M, Sugai S, et al. Expanded polyglutamine in the Machado-Joseph disease protein induces cell death in vitro and in vivo. Nat Genet 1996;13:196-202.
Torashima T, Koyama C, Iizuka A, et al. Lentivector-mediated rescue from cerebellar ataxia in a mouse model of spinocerebellar ataxia. EMBO Rep 2008;9:393-399.
Hubener J, Vauti F, Funke C, et al. N-terminal ataxin-3 causes neurological symptoms with inclusions, endoplasmic reticulum stress and ribosomal dislocation. Brain 2011;134:1925-1942.
Yamada M, Sato T, Tsuji S, Takahashi H. CAG repeat disorder models and human neuropathology: similarities and differences. Acta Neuropathol 2008;115:71-86.
Cemal CK, Carroll CJ, Lawrence L, et al. YAC transgenic mice carrying pathological alleles of the MJD1 locus exhibit a mild and slowly progressive cerebellar deficit. Hum Mol Genet 2002;11:1075-1094.
Goti D, Katzen SM, Mez J, et al. A mutant ataxin-3 putative-cleavage fragment in brains of Machado-Joseph disease patients and transgenic mice is cytotoxic above a critical concentration. J Neurosci 2004;24:10266-10279.
Bichelmeier U, Schmidt T, Hubener J, et al. Nuclear localization of ataxin-3 is required for the manifestation of symptoms in SCA3: in vivo evidence. J Neurosci 2007;27:7418-7428.
Chou AH, Yeh TH, Ouyang P, et al. Polyglutamine-expanded ataxin-3 causes cerebellar dysfunction of SCA3 transgenic mice by inducing transcriptional dysregulation. Neurobiol Dis 2008;31:89-101.
Boy J, Schmidt T, Wolburg H, et al. Reversibility of symptoms in a conditional mouse model of spinocerebellar ataxia type 3. Hum Mol Genet 2009;18:4282-4295.
Boy J, Schmidt T, Schumann U, et al. A transgenic mouse model of spinocerebellar ataxia type 3 resembling late disease onset and gender-specific instability of CAG repeats. Neurobiol Dis 2010;37:284-293.
Silva-Fernandes A, Costa MdC, Duarte-Silva S, et al. Motor uncoordination and neuropathology in a transgenic mouse model of Machado-Joseph disease lacking intranuclear inclusions and ataxin-3 cleavage products. Neurobiol Dis 2010;40:163-176.
Scott MR, Kohler R, Foster D, Prusiner SB. Chimeric prion protein expression in cultured cells and transgenic mice. Protein Sci 1992;1:986-997.
Chen X, Tang TS, Tu H, et al. Deranged calcium signaling and neurodegeneration in spinocerebellar ataxia type 3. J Neurosci 2008;28:12713-12724.
Colomer Gould VF, Goti D, Pearce D, et al. A mutant ataxin-3 fragment results from processing at a site N-terminal to amino acid 190 in brain of Machado-Joseph disease-like transgenic mice. Neurobiol Dis 2007;27:362-369.
Colomer Gould VF, Goti D, Kiluk J. A neuroendocrine dysfunction, not testicular mutant ataxin-3 cleavage fragment or aggregate, causes cell death in testes of transgenic mice. Cell Death Differ 2006;13:524-526.
Jung J, Xu K, Lessing D, Bonini NM. Preventing Ataxin-3 protein cleavage mitigates degeneration in a Drosophila model of SCA3. Hum Mol Genet 2009;18:4843-4852.
Williams AJ, Knutson TM, Colomer Gould VF, et al. In vivo suppression of polyglutamine neurotoxicity by C-terminus of Hsp70-interacting protein (CHIP) supports an aggregation model of pathogenesis. Neurobiol Dis 2009;33:342-353.
Burnett B, Li F, Pittman RN. The polyglutamine neurodegenerative protein ataxin-3 binds polyubiquitylated proteins and has ubiquitin protease activity. Hum Mol Genet 2003;12:3195-3205.
Warrick JM, Morabito LM, Bilen J, et al. Ataxin-3 suppresses polyglutamine neurodegeneration in Drosophila by a ubiquitin-associated mechanism. Mol Cell 2005;18:37-48.
Burnett BG, Pittman RN. The polyglutamine neurodegenerative protein ataxin 3 regulates aggresome formation. Proc Natl Acad Sci U S A 2005;102:4330-4335.
Nascimento-Ferreira I, Santos-Ferreira T, Sousa-Ferreira L, et al. Overexpression of the autophagic beclin-1 protein clears mutant ataxin-3 and alleviates Machado-Joseph disease. Brain 2011;134:1400-1415.
Griffin JL, Cemal CK, Pook MA. Defining a metabolic phenotype in the brain of a transgenic mouse model of spinocerebellar ataxia 3. Physiol Genomics 2004;16:334-340.
Bezprozvanny I. Role of inositol 1,4,5-trisphosphate receptors in pathogenesis of Huntington's disease and spinocerebellar ataxias. Neurochem Res 2011;36:1186-1197.
Durcan TM, Kontogiannea M, Thorarinsdottir T, et al. The Machado-Joseph disease-associated mutant form of ataxin-3 regulates parkin ubiquitination and stability. Hum Mol Genet 2011;20:141-154.
Chou AH, Chen SY, Yeh TH, Weng YH, Wang HL. HDAC inhibitor sodium butyrate reverses transcriptional downregulation and ameliorates ataxic symptoms in a transgenic mouse model of SCA3. Neurobiol Dis 2011;41:481-488.
Kretzschmar D, Tschape J, Bettencourt Da Cruz A, et al. Glial and neuronal expression of polyglutamine proteins induce behavioral changes and aggregate formation in Drosophila. Glia 2005;49:59-72.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 510 kb)
Rights and permissions
About this article
Cite this article
Colomer Gould, V.F. Mouse Models of Spinocerebellar Ataxia Type 3 (Machado-Joseph Disease). Neurotherapeutics 9, 285–296 (2012). https://doi.org/10.1007/s13311-012-0117-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-012-0117-x