Abstract
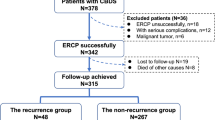
Recurrence of common bile duct stones (CBDS) is common after surgical stone extraction, but the causes of recurrence are not fully understood. This study aimed to report the experience of treating recurrent CBDS. A total of 106 consecutive cases of recurrent CBDS treated from January 2006 to December 2015 were included. During surgery, the choledochoscopic pass-through test was performed to assess the structure and function of the duodenal papilla. The choledochoscopic pass-through test revealed 62 patients (58.49%) with incomplete closure of the lower end of the common bile duct, and 28 (26.42%) with stenosis at the lower common bile duct. Intra-operative bile bacterial culture was positive in 98 (92.45%) patients. The rate of complete stone clearance was 99.1%. The total recurrence rate of CBDS was 3.13%. The long-term success rate of surgical treatment (excellent and good) reached 92.7% .Duodenal papilla (Oddi sphincter) dysfunction is the main cause of recurrent CBDS. Common bile duct exploration with stone extraction, hilar ductoplasty, and Roux-en-Y hepaticojejunostomy can effectively eliminate the recurrence of CBDS and reduce the incidence of post-hepaticojejunostomy complications. Thus, it is an optimal surgical procedure for recurrent CBDS.
Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Dasari BV, Tan CJ, Gurusamy KS et al (2013) Surgical versus endoscopic treatment of bile duct stones. In: Dasari BV (ed) Cochrane database of systematic reviews. Wiley, Chichester, p CD003327
Williams E, Beckingham I, El Sayed G et al (2017) Updated guideline on the management of common bile duct stones (CBDS). Gut 66:765–782. https://doi.org/10.1136/gutjnl-2016-312317
Shah KN, Clary BM (2017) Chapter 36A—Stones in the bile duct: clinical features and open surgical approaches and techniques. Blumgart’s surgery of the liver, biliary tract and pancreas, vol 2. Elseiver, Amsterdam, pp 585–603.e3
Salama AF, Abd Ellatif ME, Abd Elaziz H et al (2017) Preliminary experience with laparoscopic common bile duct exploration. BMC Surg 17:32. https://doi.org/10.1186/s12893-017-0225-y
Imaizumi H, Kida M, Takezawa M et al (2007) Early complications of endoscopic sphincterotomy for common bile duct stones. Dig endoscop. https://doi.org/10.1111/j.1443-1661.2007.00710.x
Cohen SA, Siegel JH, Kasmin FE (1996) Complications of diagnostic and therapeutic ERCP. Abdom Imaging 21:385–394. https://doi.org/10.1007/s002619900089
Tian XH, Liu Y, Jiang H et al (2018) A novel laparoscopic transcystic approach using an ultrathin choledochoscope and holmium laser lithotripsy in the management of cholecystocholedocholithiasis: an appraisal of their safety and efficacy. Am J Surg 215:631–635. https://doi.org/10.1016/j.amjsurg.2017.05.020
Freeman ML, Nelson DB, Sherman S et al (2002) Complications of endoscopic biliary sphincterotomy. N Engl J Med 335:909–919. https://doi.org/10.1056/nejm199609263351301
Prat F, Malak NA, Pelletier G et al (1996) Biliary symptoms and complications more than 8 years after endoscopic sphincterotomy for choledocholithiasis. Gastroenterology 110:894–899. https://doi.org/10.1053/gast.1996.v110.pm8608900
Pereira-Lima JC, Jakobs R, Winter UH et al (1998) Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc 48:457–464. https://doi.org/10.1016/S0016-5107(98)70085-9
Kawaji Y, Isayama H, Nakai Y et al (2019) Multiple recurrences after endoscopic removal of common bile duct stones: a retrospective analysis of 976 cases. J Gastroenterol Hepatol. https://doi.org/10.1111/jgh.14630
Moraca RJ, Lee FT, Ryan JA et al (2002) Long-term biliary function after reconstruction of major bile duct injuries with hepaticoduodenostomy or hepaticojejunostomy. Arch Surg 137:889–894
Lillemoe KD, Melton GB, Cameron JL et al (1990s) Postoperative bile duct strictures: management and outcome in the 1990s. Ann Surg 232:430–441. https://doi.org/10.1097/00000658-200009000-00015
Xia H-T, Dong J-H, Yang T et al (2015) Selection of the surgical approach for reoperation of adult choledochal cysts. J Gastrointest Surg 19:290–297. https://doi.org/10.1007/s11605-014-2684-0
European Association for the Study of the Liver (EASL) (2016) EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 65:146–181. https://doi.org/10.1016/j.jhep.2016.03.005
Molvar C, Glaenzer B (2016) Choledocholithiasis: evaluation, treatment, and outcomes. Semin Intervent Radiol 33:268–276. https://doi.org/10.1055/s-0036-1592329
Ko CW, Lee SP (2002) Epidemiology and natural history of common bile duct stones and prediction of disease. Gastrointest Endosc 56:S165–S169
Li Z-Q, Sun J-X, Li B et al (2019) Meta-analysis of single-stage versus two-staged management for concomitant gallstones and common bile duct stones. J Minim Access Surg. https://doi.org/10.4103/jmas.JMAS_146_18
Mattila A, Luhtala J, Mrena J et al (2014) An audit of short- and long-term outcomes after laparoscopic removal of common bile duct stones in Finland. Surg Endosc 28:3451–3457. https://doi.org/10.1007/s00464-014-3620-9
Quaresima S, Balla A, Guerrieri M et al (2016) Results of medium seventeen years’ follow-up after laparoscopic choledochotomy for ductal stones. Gastroenterol Res Pract 2016:9506406. https://doi.org/10.1155/2016/9506406
Ding G, Cai W, Qin M (2014) Single-stage vs. two-stage management for concomitant gallstones and common bile duct stones: a prospective randomized trial with long-term follow-up. J Gastrointest Surg 18:947–951. https://doi.org/10.1007/s11605-014-2467-7
Nzenza TC, Al-Habbal Y, Guerra GR et al (2018) Recurrent common bile duct stones as a late complication of endoscopic sphincterotomy. BMC Gastroenterol 18:39. https://doi.org/10.1186/s12876-018-0765-3
Uchiyama K, Onishi H, Tani M et al (2003) Long-term prognosis after treatment of patients with choledocholithiasis. Ann Surg 238:97–102. https://doi.org/10.1097/00000658-200307000-00013
Li S, Su B, Chen P, Hao J (2018) Risk factors for recurrence of common bile duct stones after endoscopic biliary sphincterotomy. J Int Med Res 46:2595–2605. https://doi.org/10.1177/0300060518765605
Il KD, Kim M-H, Lee SK et al (2001) Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc 54:42–48. https://doi.org/10.1067/mge.2001.115335
Xie A, Fang C, Huang Y et al (2013) Application of three-dimensional reconstruction and visible simulation technique in reoperation of hepatolithiasis. J Gastroenterol Hepatol 28:248–254. https://doi.org/10.1111/jgh.12066
Olsson G (2017) Aspects on the role of prophylactic procedures to influence post-ERCP complication rates. Thesis
Sharma A, Dahiya P, Khullar R et al (2012) Management of common bile duct stones in the laparoscopic era. Indian J Surg 74:264–269. https://doi.org/10.1007/s12262-012-0593-6
Chang JH, Kim TH, Kim CW et al (2014) Size of recurrent symptomatic common bile duct stones and factors related to recurrence. Turk J Gastroenterol 25:518–523. https://doi.org/10.5152/tjg.2014.6457
Oak JH, Paik CN, Chung WC et al (2012) Risk factors for recurrence of symptomatic common bile duct stones after cholecystectomy. Gastroenterol Res Pract 2012:1–6. https://doi.org/10.1155/2012/417821
Tsai T-J, Lin C-K, Lai K-H et al (2018) Does preserved sphincter of Oddi function prevent common bile duct stones recurrence in patients after endoscopic papillary balloon dilation? J Chin Med Assoc 81:311–315. https://doi.org/10.1016/j.jcma.2018.01.007
Ahmed M (2018) Acute cholangitis - an update. World J Gastrointest Pathophysiol 9:1–7. https://doi.org/10.4291/wjgp.v9.i1.1
Zhou B, Hu J, Zhong Y (2017) Surgical treatments for patients with recurrent bile duct stones and Oddis sphincter laxity. Intractable Rare Dis Res 6:172–176. https://doi.org/10.5582/irdr.2017.01053
Xia H-T, Liu Y, Yang T et al (2017) Better long-term outcomes with hilar ductoplasty and a side-to-side Roux-en-Y hepaticojejunostomy. J Surg Res 215:21–27. https://doi.org/10.1016/j.jss.2017.03.036
Geng Z-M, Yao Y-M, Liu Q-G et al (2005) Mechanism of benign biliary stricture: a morphological and immunohistochemical study. World J Gastroenterol 11:293. https://doi.org/10.3748/wjg.v11.i2.293
Xia HT, Yang T, Liu Y et al (2018) Proper bile duct flow, rather than radical excision, is the most critical factor determining treatment outcomes of bile duct cysts. BMC Gastroenterol. https://doi.org/10.1186/s12876-018-0862-3
Funding
None.
Author information
Authors and Affiliations
Contributions
HTX: study design, data collections, data analysis, writing,final approval of manuscript. XLX: study design, data collections, data analysis, writing,final approval of manuscript. TY: data collections, data analysis,final approval of manuscript. YL: data collections, data analysis,final approval of manuscript. BL: data collections, data analysis,final approval of manuscript. JW: data collections, data analysis, final approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Ethics approval
This study was approved by the Institutional Review Board (IRB) of our hospital, and the requirement of written informed consent was waived due to the retrospective nature of this study.
Consent for publication
The authors agree to transfer the ownership of copyright to Updates in Surgery.
Informed consent
For this type of study, no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xia, H., Xin, X., Yang, T. et al. Surgical strategy for recurrent common bile duct stones: a 10-year experience of a single center. Updates Surg 73, 1399–1406 (2021). https://doi.org/10.1007/s13304-020-00882-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00882-8