Abstract
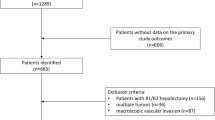
Occult metastasis from the initial tumor and a de novo second primary hepatocellular carcinoma (HCC) were recognized as the main causes for the onset of early and late HCC recurrence, after liver resection (LR). This study aims to compare the time to recurrence after LR for HCC in which a margin ≤ 1 mm or > 1 mm was achieved. A single-center retrospective study involving 256 patients was conducted from June 2005 to June 2019. HCC patients resected with a radical surgical approach were investigated and stratified into groups A (resection margins ≤ 1 mm) and B (> 1 mm), as measured on final pathologic assessment. Kaplan–Meier estimators were used to estimate the probability of recurrence, and the log-rank test was used to compare groups. Uni- and multivariable (stepwise) Cox regression models were used to assess the effect of several HCC pathological characteristics. Twenty patients were excluded for the presence of microscopic tumor invasion at pathologic analysis (R1); 236 patients underwent radical (R0) LR, and were included in the study and divided into group A (n = 61, 26%), and group B (n = 175, 74%). No differences between the two groups were detected regarding: epidemiology, tumor characteristics, type of LR, and follow-up. The estimated probability of recurrence for group A and group B at 12 and 24 months was 27% and 38%, and, 33% and 46%, respectively. Univariate and multivariable Cox regression model estimates showed that tumor grading (HR 2.1, 95% CI 1.2–3.4, p = 0.006), number of nodules (HR 1.2, 95% CI 1.0–1.4, p = 0.015), and extension of the resection (HR 1.8, 95% CI 1.0–1.1, p = 0.047) were independent risk factors for HCC recurrence, with no significant effect of margin status on time to recurrence. A R0 approach that considers a margin of resection > 1 mm does not improve the likelihood of HCC recurrence. Otherwise, our experience confirms that biologic tumor characteristics are the principal factors predictive of local and systemic recurrence.



Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- BCLC:
-
Barcelona clinic liver cancer
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- HCC:
-
Hepatocellular carcinoma
- HR:
-
Hazard ratio
- INR:
-
International normalized ratio
- IQR:
-
Inter-quartile range
- PHT:
-
Portal hypertension
- LR:
-
Liver resection
- LT:
-
Liver transplantation
- RECIST:
-
Response evaluation criteria in solid tumors
- TACE:
-
Transarterial chemoembolization
- TTR:
-
Time to recurrence
References
Mazzaferro V, Llovet JM, Miceli R et al (2009) Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol 10:35
Farinati F, Giacomin A, Vanin V, Sergio A, Burra P, Cillo U, Di Nolfo A, Del Poggio P, Benvegnu L, Zoli M, Borzio F, Giannini EG, Caturelli E, Cazzagon N, Rapaccini GL, Trevisani F, Italian Liver Cancer (ITA.LI.CA) group (2012) Liver transplantation for hepatocellular carcinoma in clinical practice: the lesson from a 20-year multicentre experience in Italy. Eur J Gastroenterol Hepatol. 24(2):195–202
Gruttadauria S, di Francesco F, Spada M (2012) Fifty-six-month survival after liver transplantation in a patient with more than one-hundred hepatocellular carcinoma nodules. Transpl Int. 25(9):e101–e103. https://doi.org/10.1111/j.1432-2277.2012.01507.x(Epub 2012 May 26. No abstract available. PMID: 22632155)
Torzilli G, Donadon M, Marconi M, Palmisano A, Del Fabbro D, Spinelli A, Botea F, Montorsi M (2008) Hepatectomy for stage B and stage C hepatocellular carcinoma in the Barcelona clinic liver cancer classification: results of a prospective analysis. Arch Surg 143(11):1082–1090
Onali S, Marshall A, Sharma D, O’Donoghue P, Dannhorn E, Johnson P et al (2015) ALBI score predicts survival independently of hepatic venous pressure gradient (HVPG) and indocyanine green (ICG) clearance in HCC patients undergoing resection. Gut 64(Suppl):A460–A461
Jianyong L, Lunan Y, Wentao W, Yong Z, Bo L, Tianfu W, Minqing X, Jiaying Y (2014) Barcelona clinic liver cancer stage B hepatocellular carcinoma: trans-arterial chemoembolization or hepatic resection? Medicine (Baltimore) 93(26):e180
Torzilli G, Belghiti J, Kokudo N, Takayama T, Capussotti L, Nuzzo G, Vauthey JN, Choti MA, De Santibanes E, Donadon M, Morenghi E, Makuuchi M (2013) A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: is it adherent to the EASL/AASLD recommendations? An observational study of the HCC East-West study group. Ann Surg 257(5):929–937
Iguchi K, Hatano E, Yamanaka K, Tanaka S, Taura K, Uemoto S (2015) Validation of the conventional resection criteria in patients with hepatocellular carcinoma in terms of the incidence of post-hepatectomy liver failure and long-term prognosis. Dig Surg 32(5):344
Ciria R, López-Cillero P, Gallardo AB, Cabrera J, Pleguezuelo M, Ayllón MD, Luque A, Zurera L, Espejo JJ, Rodríguez-Perálvarez M, Montero JL, de la Mata M, Briceño J (2015) Optimizing the management of patients with BCLC stage-B hepatocellular carcinoma: modern surgical resection as a feasible alternative to transarterial chemoemolization. Eur J Surg Oncol 41(9):1153
Gruttadauria S, Pagano D, Tropea A, Cintorino D, Castellana L, Bonsignore P, Ricotta C, Piccolo G, Vizzini G, Luca A (2016) Laparoscopic approach for thermoablation microwave in the treatment of hepatocellular carcinoma: a single center experience. J Laparoendosc Adv Surg Tech A 26(10):808–811
Gruttadauria S, Tropea A, Pagano D, Guarini A, Liotta R, Ling T, Tuzzolino F, Luca A, Vizzini G, Gridelli B (2016) Mini-invasive approach contributes to expand the indication for liver resection for hepatocellular carcinoma without increasing the incidence of posthepatectomy liver failure and other perioperative complications: a single-center analysis. J Laparoendosc Adv Surg Tech A 26(6):439–446
Patel T, Harnois D (2014) Assessment of response to therapy in hepatocellular carcinoma. Ann Med 46(3):130–137
Ishizawa T, Hasegawa K, Aoki T, Takahashi M, Inoue Y, Sano K, Imamura H, Sugawara Y, Kokudo N, Makuuchi M (2008) Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology 134(7):1908–1916
Capussotti L, Ferrero A, Viganò L, Muratore A, Polastri R, Bouzari H (2006) Portal hypertension: contraindication to liver surgery? World J Surg 30(6):992–999
Kingham TP, Correa-Gallego C, D’Angelica MI, Gönen M, DeMatteo RP, Fong Y, Allen PJ, Blumgart LH, Jarnagin WR (2015) Hepatic parenchymal preservation surgery: decreasing morbidity and mortality rates in 4152 resections for malignancy. J Am Coll Surg 220(4):471–479
Lowe MC, D’Angelica MI (2016) Anatomy of hepatic resectional surgery. Surg Clin N Am 96(2):183–195
Mitsuyoshi A, Inoguchi K, Yokoyama D (2016) The Cavitron ultrasonic surgical aspirator with a low amplitude is a useful dissection device for surgical procedures: application to vascular detachment and lymph node dissection. Updates Surg 68(2):205–209. https://doi.org/10.1007/s13304-016-0360-5
Zhong FP, Zhang YJ, Liu Y, Zou SB (2017) Prognostic impact of surgical margin in patients with hepatocellular carcinoma: a meta-analysis. Medicine (Baltimore) 96:e8043
Poon RT-P, Fan S-T, Ng IO, Wong J (2000) Significance of resection margin in hepatectomy for hepatocellular carcinoma. Ann Surg 231:544–551
Matsui Y, Terakawa N, Satoi S et al (2007) Postoperative outcomes in patients with hepatocellular carcinomas resected with exposure of the tumor surface: clinical role of the no-margin resection. Arch Surg 142:596–602
Torzilli G, Donadon M, Cimino M (2012) Are tumor exposure and anatomical resection antithetical during surgery for hepatocellular carcinoma? A critical review. Liver Cancer 1:177–182
Donadon M, Terrone A, Procopio F, Cimino M, Palmisano A, Viganò L, Del Fabbro D, Di Tommaso L, Torzilli G (2019) Is R1 vascular hepatectomy for hepatocellular carcinoma oncologically adequate? Analysis of 327 consecutive patients. Surgery 165(5):897–904
Koh PS, Chan AC, Cheung TT, Chok KS, Dai WC, Poon RT, Lo CM (2016) Efficacy of radiofrequency ablation compared with transarterial chemoembolization for the treatment of recurrent hepatocellular carcinoma: a comparative survival analysis. HPB (Oxford) 18(1):72–78
Levi Sandri GB, Ettorre GM, Aldrighetti L, Cillo U, Dalla Valle R, Guglielmi A, Mazzaferro V, Ferrero A, Di Benedetto F, Gruttadauria S, De Carlis L, Vennarecci G, I Go MILS Group on HCC (2019) Laparoscopic liver resection of hepatocellular carcinoma located in unfavorable segments: a propensity score-matched analysis from the I Go MILS (Italian Group of Minimally Invasive Liver Surgery) Registry. Surg Endosc 33(5):1451–1458
Levi Sandri GB, Spoletini G, Vennarecci G, Francone E, Abu Hilal M, Ettorre GM (2018) Laparoscopic liver resection for large HCC: short- and long-term outcomes in relation to tumor size. Surg Endosc 32(12):4772–4779
Wakabayashi G, Cherqui D, Geller DA et al (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261:619–629
Field WBS, Rostas JW, Philps P, Scoggins CR, McMasters KM, Martin RCG 2nd (2017) Wide versus narrow margins after partial hepatectomy for hepatocellular carcinoma: balancing recurrence risk and liver function. Am J Surg 214(2):273–277
van der Pol CB, Lim CS, Sirlin CB, McGrath TA, Salameh JP, Bashir MR, Tang A, Singal AG, Costa AF, Fowler K, McInnes MDF (2019) Accuracy of the liver imaging reporting and data system in computed tomography and magnetic resonance image analysis of hepatocellular carcinoma or overall malignancy—a systematic review. Gastroenterology 156(4):976–986
Kim Y, Furlan A, Borhani AA, Bae KT (2018) Computer-aided diagnosis program for classifying the risk of hepatocellular carcinoma on MR images following liver imaging reporting and data system (LI-RADS). J Magn Reson Imaging 47(3):710–722
Pagano D, Barbera F, Conaldi PG, Seidita A, Di Francesco F, Di Carlo D, Bàrbara M, Tuzzolino F, Luca A, Gruttadauria S (2019) Role of Allelic imbalance in predicting hepatocellular carcinoma (HCC) recurrence risk after liver transplant. Ann Transplant 24:223–233
Lim C, Salloum C, Lahat E, Sotirov D, Eshkenazy R, Shwaartz C, Azoulay D. Impact of narrow margin and R1 resection for hepatocellular carcinoma on the salvage liver transplantation strategy. An intention-to-treat analysis. HPB (Oxford). 2019. https://doi.org/10.1016/j.hpb.2019.02.001
Tsilimigras DI, Sahara K, Moris D, Hyer JM, Paredes AZ, Bagante F, Merath K, Farooq AS, Ratti F, Marques HP, Soubrane O, Azoulay D, Lam V, Poultsides GA, Popescu I, Alexandrescu S, Martel G, Guglielmi A, Hugh T, Aldrighetti L, Endo I, Pawlik TM (2019) Effect of surgical margin width on patterns of recurrence among patients undergoing R0 hepatectomy for T1 hepatocellular carcinoma: an international multi-institutional analysis. J Gastrointest Surg 1:7. https://doi.org/10.1007/s11605-019-04275-0(Epub ahead of print)
Author information
Authors and Affiliations
Contributions
SG: critical revision of article, approval of article. DP, LRC, DC, SLP, SC, AS, and FdiF: concept/design, data analysis/interpretation, and drafting article.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest, as described by this journal, to disclose. This manuscript has not been published, and is not under consideration elsewhere. We declare that all authors are in agreement on the content of the manuscript and have no potential conflicts of interest. We have nothing to disclose regarding sources of support in the form of grants, equipment, and/or pharmaceuticals.
Research involving human participants and/or animals
Institutional review research board approval was granted by ISMETT-IRCCS, and appropriate good clinical and research practices were followed.
Informed consent
We have obtained consent to publish from the participants to report individual patient data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gruttadauria, S., Pagano, D., Corsini, L.R. et al. Impact of margin status on long-term results of liver resection for hepatocellular carcinoma: single-center time-to-recurrence analysis. Updates Surg 72, 109–117 (2020). https://doi.org/10.1007/s13304-019-00686-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-019-00686-5