Abstract
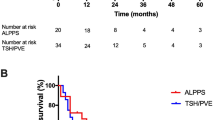
The ALPPS is a technique that allows achieving hepatic resection by a rapid future liver remnant hypertrophy. The aim of this study was to report the experience of an Italian center with ALPPS in patients with liver tumors. A retrospective analysis of patients undergoing ALPPS between 2012 and 2017 was performed. Patients’ characteristics and disease presentation, increase in future liver remnant (FLR) as well as intraoperative and postoperative short- and long-term outcomes were evaluated. A total of 24 patients underwent the ALPPS procedure: 17 procedures for hepatocarcinoma (HCC), 5 for colorectal liver metastases (CRLM), 1 for cholangiocarcinoma (CC) and 1 for Merkel Cell Carcinoma liver metastasis (MCCLM). Macrovascular invasion (MVI) was recorded in 10 (41.6%) patients: 8 (33.3%) patients with HCC had invasion of portal vein (5), middle hepatic vein (2) and inferior vena cava (1). One patient with CRLM had involvement of middle hepatic vein and one patient with CC had involvement of right portal vein and middle hepatic vein. A p-ALPPS in 14 cases (58.3%), 10 t-ALPPS (41.6%) and hanging maneuver in 19 patients (80%) were performed. Median postoperative stay was 26 days (range 16–68 days). 90-day mortality was 8.3% (two patients, one with CC and one with HCC), 90-day mortality for HCC was 5.8%. After stage 1, we counted 15 complications all of grade I; after stage 2 the number of complications was increased to 37:33 were of grade I and 4 were of grade IV. R0 resection was achieved in all patients with 100% oncology feasibility. After a median follow-up of 10 months (range 2–54), disease recurrence has been recorded in 6 patients with HCC and in 2 with CRLM. Eleven patients died, nine affected by HCC, one by CRLM, and one by CC. 2-years OS and disease-free survival (DFS) for the entire group were 47.3% and 47.5%, respectively. Concerning patients operated on for HCC, the 2-years OS and DFS were 38.5% and 60%, respectively. The ALPPS procedure is an interesting approach for large primary or secondary liver tumor with small FLR above all for large HCC associated with MVI, with acceptable OS and DFS.


Similar content being viewed by others
References
Hemming AW, Reed AI, Howard RJ et al (2003) Preoperative portal vein embolization for extended hepatectomy. Ann Surg 237:686
Liu H, Zhu S (2009) Present status and future perspectives of preoperative portal vein embolization. Am J Surg 197:686–690
Farges O, Belghiti J, Kianmanesh R et al (2003) Portal vein embolization before right hepatectomy. Ann Surg 237:208–217
Abulkhir A, Limongelli P, Healey AJ et al (2008) Preoperative portal vein embolizaion for major liver resection: a meta-analysis. Ann Surg 247:49–57
Wicherts DA, de Haas RJ, Andreani P et al (2010) Impact of portal vein embolization on long-term survival of patients with primarily unresectable colorectal liver metastases. Br J Surg 97:240–250
Schnitzbauer AA, Lang SA, Goessmann H et al (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling two-staged extended right hepatic resection in small for size settings. Ann Surg 255:405–414
Alvarez FA, Ardiles V, Sanchez Claria R et al (2013) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): tips and tricks. J Gastrointest Surg 17:814–821
Cavaness KM, Doyle MB, Lin Y et al (2013) Using ALPPS to induce rapid liver hypertrophy in a patient with hepatic fibrosis and portal vein thrombosis. J Gastrointest Surg 17:207–212
Vennarecci G, Laurenzi A, Santoro R et al (2013) The ALPPS procedure: a surgical option for hepatocellular carcinoma with major vascular invasion. World J Surg. https://doi.org/10.1007/s00268-013-2296-y
de Santibañes M, Boccalatte L, de Santibañes E (2017) A literature review of associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): so far, so good. Updates Surg 69(1):9–19. https://doi.org/10.1007/s13304-016-0401-0 (Epub 2016 Oct 20)
Truant S, Baillet C, Deshorgue AC et al (2017) Contribution of hepatobiliary scintigraphy in assessing ALPPS most suited timing. Updates Surg 69(3):411–419
Serenari M, Zanello M, Schadde E et al (2016) ALPPS Italian registry group. Importance of primry indication and liver function between stages: results of a multicenter Italian audit of ALPPS 2012–2014. HPB (Oxf) 18(5):419–427. https://doi.org/10.1016/j.hpb.2016.02.003 (Epub 2016 Mar 13)
Schadde E, Schnitzbauer AA, Tschuor C et al (2015) Systematic review and meta-analysis of feasibility, safety, and efficacy of a novel procedure: associating liver partition and portal vein ligation for staged hepatectomy. Ann Surg Oncol 22:3109–3120
Truant S, Scatton O, Dokmak S et al (2015) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): impact of the inter-stages course on morbi-mortality and implica tions for management. Eur J Surg Oncol 41:674–682
Croome KP, Hernandez-Alejandro R, Parker M et al (2015) Is the liver kinetic growth rate in ALPPS unprecedented when compared with PVE and living donor liver transplant? A multicentre a nal ysis. HPB 17:477–484
Ratti F, Schadde E, Masetti M et al (2015) Strategies to increase the resectability of patients with colo rectal liver metastases: a multi-center case-match analysis of ALPPS and conventional two-stage hepatectomy. Ann Surg Oncol 22:1933–1942
Schadde E, Ardiles V, Slankamenac K et al (2014) ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg 38:1510
Shindoh J, Vauthey JN, Zimmitti G et al (2013) Analysis of the efficacy of portal vein embolization for patients with extensive liver malignancy and very low future liver remnant volume, in cluding a comparison with the associating liver partition with portal vein ligation for staged hepatectomy approach. J Am Coll Surg. 217:126–133 (discussion 133–124)
Petrowsky H, Györi G, de Oliveira M et al (2015) Is partial-ALPPS safer than ALPPS? A single-center experience. Ann Surg 261(4):e90–e92
Vennarecci G, Levi Sandri GB, Ettorre GM (2016) Performing the ALPPS procedure by anterior approach and liver hanging maneuver. Ann Surg 263(1):e11
Vennarecci G, Grazi GL, Sperduti I et al (2016) ALPPS for primary and secondary liver tumors. Int J Surg 30:38–44. https://doi.org/10.1016/j.ijsu.2016.04.031 (Epub 2016 Apr 22)
Oldhafer KJ, Donati M, Jenner RM et al (2014) ALPPS for patients with colorectal liver metastases: effective liver hypertrophy, but early tumor recurrence. World J Surg 38(6):1504–1509. https://doi.org/10.1007/s00268-013-2401-2
Shang J, Xu S, Zhang J, Ran X, Bai L, Tang H (2017) Efficacy of sorafenib in patients with hepatocellular carcinoma after resection: a meta-analysis. Oncotarget 8(65):109723–109731. https://doi.org/10.18632/oncotarget.21299 (eCollection 2017 Dec 12)
Vennarecci G, Grazi GL, Santoro R (2015) Ettorre GM.A room for the alpps procedure in patients with HCC. Int J Surg 13:90–91. https://doi.org/10.1016/j.ijsu.2014.11.054 (Epub 2014 Dec 9)
D’Haese JG, Neumann J, Weniger M et al (2016) Should ALPPS be used for liver resection in intermediate-stage HCC? Ann Surg Oncol 23(4):1335–1343
Chan AC, Poon RT, Chan C et al (2016) Safety of ALPPS Procedure by the Anterior Approach for Hepatocellular Carcinoma. Ann Surg 263:e14–e16
Cai X, Tong Y, Yu H, Liang X, Wang Y, Liang Y, Li Z, Peng S, Lau WY (2017) The ALPPS in the treatment of hepatitis B-related hepatocellular carcinoma with cirrhosis: a single-center study and literature review. Surg Innov 24(4):358–364. https://doi.org/10.1177/1553350617697187 (Epub 2017 Mar 12)
Torres OJ, Vasques RR, Silva TH, Castelo-Branco ME, Torres CC (2016) The ALPPS procedure for hepatocellular carcinoma larger than 10 centimeters. Int J Surg Case Rep 26:113–117. https://doi.org/10.1016/j.ijscr.2016.07.039 (Epub 2016 Jul 28)
Cheung TT, Wong TC, Chan SC (2016) Technical note on ALPPS for a patient with advanced hepa tocellular carcinoma associated with invasion of the inferior vena cava. Hepatobiliary Pancreat Dis Int 15(3):319–323
Heimbach J, Kulik LM, Finn R et al (2017) Aasld guidelines for the treatment of hepatocellular carcinoma. Hepatology. https://doi.org/10.1002/hep.29086
European Association for the Study of the Liver (2012) European organisation for research and treatment of cancer. EASL–EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Kokudo T, Hasegawa K, Matsuyama Y et al (2016) Survival benefit of liver resection for hepatocellu lar carcinoma associated with portal vein invasion. Liver cancer study group of Japan. J Hepatol 65:938–943
Costentin CE, Decaens T, Laurent A et al (2017) Sorafenib vs surgical resection for hepatocellular carcinoma with macrovascular invasion: a propensity score analysis. Liver Int 37(12):1869–1876
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors do not have conflict of interest. The manuscript has not been submitted to other journals for simultaneous consideration.
Research involving human participants and/or animals
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the study patients.
Rights and permissions
About this article
Cite this article
Vennarecci, G., Ferraro, D., Tudisco, A. et al. The ALPPS procedure: hepatocellular carcinoma as a main indication. An Italian single-center experience. Updates Surg 71, 67–75 (2019). https://doi.org/10.1007/s13304-018-0596-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0596-3