Abstract
Introduction
iGlarLixi, a fixed-ratio combination of insulin glargine 100 U/mL and the glucagon-like peptide 1 receptor agonist (GLP-1 RA) lixisenatide, is one option for treatment intensification in individuals with type 2 diabetes (T2D) who are unable to achieve targeted glycaemic control with their current glucose-lowering agent. Real-world data on the impact of prior treatment on the effectiveness and safety of iGlarLixi may be useful to guide individualised treatment decisions.
Methods
This analysis of the 6-month, retrospective, observational SPARTA Japan study compared glycated haemoglobin (HbA1c), body weight and safety for pre-specified subgroups defined by prior treatment: post oral antidiabetic agent (OAD), GLP-1 RA, basal insulin (BI) + OADs (BOT), GLP-1 RA + BI or multiple daily injections (MDI). The post BOT and MDI subgroups were further divided on the basis of prior dipeptidyl peptidase 4 inhibitor (DPP-4i) use, and the post MDI group was divided on the basis of whether participants continued bolus insulin.
Results
Of the 432 participants in the full analysis set (FAS), 337 were included in this subgroup analysis. Across subgroups, mean baseline HbA1c ranged from 8.49% to 9.18%. iGlarLixi significantly (p < 0.05) reduced mean HbA1c from baseline in all but the post GLP-1 RA + BI group. At 6 months, these significant reductions ranged from 0.47% to 1.27%. Prior DPP-4i exposure had no impact on the HbA1c-lowering effect of iGlarLixi. Mean body weight decreased significantly in the FAS (0.5 kg) and the post BOT (1.2 kg) and MDI (1.5 and 1.9 kg) subgroups but increased in the post GLP-1 RA subgroup (1.3 kg). iGlarLixi treatment was generally well tolerated, with very few participants discontinuing because of hypoglycaemia or gastrointestinal events.
Conclusion
In participants with suboptimal glycaemic control on various regimens, 6 months of iGlarLixi treatment improved HbA1c in all but one prior treatment subgroup (GLP-1 RA + BI), and was generally well tolerated.
Trial Registration
UMIN-CTR Trials Registry, UMIN000044126; registered 10 May 2021.
Plain Language Summary
Despite initially receiving oral treatment for their diabetes, many individuals with type 2 diabetes are unable to achieve their blood glucose targets and require treatment intensification as their disease progresses. In these individuals, options for treatment intensification include adding an injectable therapy, such as a glucagon-like peptide 1 receptor agonist or basal insulin, or the combination of both. However, the impact of previously received treatments on the ability of treatment intensification to improve outcomes in these individuals has yet to be evaluated. Here, we report the findings of an analysis that aimed to determine the influence of different treatment backgrounds on the effectiveness and safety of iGlarLixi, a fixed-ratio combination (i.e. combined as a single subcutaneous injection) of the glucagon-like peptide 1 receptor agonist lixisenatide and basal insulin glargine 100 U/mL, in Japanese individuals with type 2 diabetes. We found that iGlarLixi improved glycaemic control and was well tolerated in most individuals, regardless of previously received treatments. These results suggest that iGlarLixi may offer an effective option for improving outcomes in Japanese individuals with type 2 diabetes who require treatment intensification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
In individuals with type 2 diabetes (T2D) requiring treatment intensification, identifying subgroups of individuals who are more likely to respond to treatment can improve individualised treatment decision-making. |
The aim of this subgroup analysis of SPARTA Japan, a retrospective, observational study investigating the real-world effectiveness and safety of iGlarLixi (a fixed-ratio combination of insulin glargine 100 U/mL and the glucagon-like peptide 1 receptor agonist [GLP-1 RA] lixisenatide) in Japanese individuals, was to determine the influence of different treatment backgrounds on the effectiveness and safety of iGlarLixi. |
What was learned from the study? |
The use of iGlarLixi in a real-world setting was associated with improved glycaemic control (a reduction in glycated haemoglobin, HbA1c) in all but one prior treatment regimen subgroup (participants who had previously received a GLP-1 RA + basal insulin). |
In participants who had previously received a GLP-1 RA + basal insulin, iGlarLixi treatment maintained HbA1c, while reducing the burden of multiple daily injections. |
iGlarLixi was well tolerated in all prior treatment regimen subgroups. |
Introduction
Both globally and in Japan, the incidence of type 2 diabetes (T2D) is expected to continue to increase, with the increase in Japan largely due to an ageing population and a Westernised lifestyle [1]. Maintaining glycaemic control is critical in reducing the risk of long-term T2D complications [2], but as this may not be adequate with oral glucose-lowering agents (OADs) alone, many individuals require treatment intensification with one or more injectable agents [3, 4], including glucagon-like peptide 1 receptor agonists (GLP-1 RAs) and insulin [5]. Clinical trials have shown that treatment intensification with a GLP-1 RA plus basal insulin (BI) is more effective and has a more durable effect than intensification with BI alone, and is associated with less hypoglycaemia and weight gain than intensified insulin regimens [6,7,8,9].
Although guidelines recommend regularly reviewing treatment and intensifying without delay when goals are not being met [4], clinical inertia is common, and can result in suboptimal glycaemic control and an increased risk of complications [2, 10]. There are many barriers to treatment intensification, including concern about insulin-related adverse events (AEs) and difficulties with regimens requiring multiple injections [10]. With a view to reducing injection burden and the incidence of AEs, fixed-ratio combinations of BI and a GLP-1 RA have been developed [11]. One such fixed-ratio combination is insulin glargine plus lixisenatide (iGlarLixi). Randomised clinical trials have demonstrated the efficacy and safety of iGlarLixi (1:1) in Japanese individuals with T2D that was suboptimally controlled with OADs [9, 12] or OADs plus BI [8]. Furthermore, the retrospective, observational ‘SPARTA Japan’ study confirmed the effectiveness and safety of iGlarLixi in routine clinical practice in Japan [13]. In SPARTA Japan, 6 months of iGlarLixi treatment significantly reduced mean glycated haemoglobin (HbA1c) and body weight compared with baseline, with a low incidence of hypoglycaemia and gastrointestinal events.
Identifying subgroups of individuals who are more likely to respond to treatment can improve individualised treatment decision-making. In SPARTA Japan, greater improvements were seen in individuals with a shorter duration of T2D and those with higher baseline HbA1c. In order to better understand the effectiveness of iGlarLixi in individuals with different treatment backgrounds, we conducted a subgroup analysis of SPARTA Japan based on prior T2D treatment. Here, we report the results of this subgroup analysis.
Methods
Study Design and Population
The study design and methods have been previously described [13]. Briefly, SPARTA Japan was a retrospective, observational study that collected data from the medical records of eligible participants from 27 medical institutions across Japan. Data were included for adults with T2D (as diagnosed by their treating physician) who had initiated treatment with iGlarLixi at least 6 months before data collection and had data available for the following: HbA1c within 3 months prior to iGlarLixi initiation; HbA1c within 6 months after treatment initiation; and body weight within 6 months prior to iGlarLixi initiation. Exclusion criteria included a diagnosis of type 1 diabetes, treatment with insulin degludec/liraglutide (IDegLira) within 3 months prior to initiation of iGlarLixi, or off-label use of iGlarLixi.
Compliance with Ethics Guidelines
Written informed consent for the use of participant data was obtained, and SPARTA Japan was approved by a central ethics committee (Sone Clinic in Tokyo, Japan; on 24 February 2021) for some institutions and by their own institutional ethics committee in other institutions. Individual institutions and their respective ethics committees are listed in Supplementary Table S1. SPARTA Japan was a retrospective observational study and, as such, compliance with the Declaration of Helsinki 1964 was not required.
Study Objectives and Endpoints
The primary endpoint of SPARTA Japan was the change in HbA1c from baseline to 6 months after the initiation of iGlarLixi treatment. Secondary endpoints included the change in HbA1c after 3 months of treatment, and the proportion of participants achieving age-defined HbA1c targets at 3 and 6 months after treatment (< 65 years, < 7.0%; 65 to < 75 years, < 7.5%; ≥ 75 years, < 8.0% [14]). Exploratory endpoints, assessed at 3 and 6 months after treatment initiation, included changes in body weight and iGlarLixi dose, and the incidence of hypoglycaemia and gastrointestinal events.
For this analysis, data were compared for five subgroups defined by prior treatment. (1) Suboptimally controlled on OADs (henceforth referred to as ‘post OAD’), defined as participants who had not received any insulin or GLP-1 RAs within 3 months prior to the initiation of iGlarLixi. This subgroup was further stratified by use of dipeptidyl peptidase 4 inhibitor (DPP-4i) within 3 months prior to the initiation of iGlarLixi (‘post OAD, DPP-4i (+)’ and ‘post OAD, DPP-4i (−)’, respectively). (2) Switched from combination therapy with OADs plus insulin (BI-supported oral therapy [BOT], henceforth referred to as ‘post BOT’), defined as participants who received BI with OADs (regardless of treatment interruption) within 3 months prior to the initiation of iGlarLixi, but had not received GLP-1 RAs or bolus insulin. This subgroup was further stratified by baseline daily BI dose (< 10 units [U]/day, ≥ 10 U/day), and use of DPP-4i within 3 months prior to the initiation of iGlarLixi, henceforth referred to as ‘post BOT, DPP-4i (+)’ and ‘post BOT, DPP-4i (−)’, respectively. (3) Switched from combination therapy with OADs plus GLP-1 RA (henceforth referred to as ‘post GLP-1 RA’), defined as participants who had received a GLP-1 RA with OADs (regardless of treatment interruption) within 3 months prior to the initiation of iGlarLixi, but had not received any insulin. (4) Switched from combination therapy with GLP-1 RA plus BI (henceforth referred to as ‘post GLP-1 RA + BI’), defined as participants who had received a GLP-1 RA with BI (regardless of treatment interruption) within 3 months prior to the initiation of iGlarLixi, but had not received any other insulin preparations concomitantly. (5) Switched from multiple daily injections (MDI) (henceforth referred to as ‘post MDI’), defined as participants who had received BI and bolus insulin within 3 months prior to the initiation of iGlarLixi, and had not received concomitant GLP-1 RA. This group was further divided into two subgroups: those who continued bolus insulin after the initiation of iGlarLixi, henceforth referred to as ‘post MDI, bolus insulin (+)’; and those who did not continue bolus insulin after the initiation of iGlarLixi, henceforth referred to as ‘post MDI, bolus insulin (−)’. Between-subgroup comparisons for change from baseline in HbA1c at 6 months were adjusted for baseline HbA1c, diabetes duration and age.
For this subgroup analysis, data were excluded for the following participants: those who received prior treatment with diet and exercise therapy alone; those who switched from GLP-1 RA or BI monotherapy (without an OAD); those who switched from BOT or GLP-1 RA + BI and had received BI other than long-acting insulin; or those who were post-OAD, or switched from GLP-1 RA or GLP-1 RA + BI in combination with bolus insulin.
Definitions of Timeframes
Because this was a retrospective analysis of data collected during routine clinical practice, assessments were not necessarily performed at set time points. Baseline data were those collected closest to the start of iGlarLixi treatment, within 6 months prior to initiation, or within 3 months prior to initiation for HbA1c data. During the iGlarLixi treatment period, 3- and 6-month HbA1c and body weight data were collected with a window of ± 45 days for each time point.
Statistical Analysis
The rationale for sample size calculations for the primary analysis has been defined previously [13]. In the current report, all analyses are descriptive. Baseline characteristics are presented as summary statistics, including mean (standard deviation, SD), median (range) and n (%). For the full analysis set (FAS) and the prior treatment subgroups, changes from baseline in HbA1c, body weight and treatment dose were compared using a paired t test. The McNemar’s test was used to compare the proportion of study participants who achieved treatment targets (HbA1c < 7.0% and age-specific HbA1c targets) at 3 and 6 months after initiation of iGlarLixi versus baseline. For changes in HbA1c and body weight, the mean and 95% confidence interval (CI) were also calculated. The incidence of hypoglycaemia and gastrointestinal events were also assessed. Statistical analyses were performed using SAS® Version 9.4 (SAS Institute; Cary, NC, USA).
Results
Study Cohort and Demographics
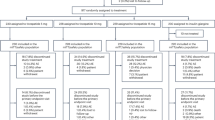
Of the 469 participants enrolled, 432 were included in the FAS [13]. Of these, 338 met the pre-specified criteria for inclusion in this subgroup analysis; however, one individual in the post BOT subgroup was incorrectly classified as receiving BI, so the total number of participants in this subgroup analysis was 337 (Fig. 1). At baseline, the mean age ranged from 58.5 to 63.2 years across subgroups, and the proportion of participants aged under 65 years ranged from 45.5% to 71.8% (Table 1). Mean body weight and body mass index (BMI) ranged from 70.1 to 73.1 kg and 26.2 to 27.2 kg/m2, respectively. The majority of participants had a duration of diabetes of at least 10 years; the mean duration was lowest in the post GLP-1 RA + BI subgroup (10.5 years), followed by the post MDI, bolus insulin (−) subgroup (11.8 years), and highest in the post MDI, bolus insulin (+) subgroup (15.8 years). Mean (median) baseline HbA1c ranged from 8.49% to 9.18% (7.90% to 9.10%). In all prior treatment subgroups, more than 75% of participants continued to take concomitant OADs.
Number of participants in each prior treatment subgroup. *Data are missing for eight participants in these subgroups. BI basal insulin, BOT basal insulin-supported oral therapy, DPP-4i dipeptidyl peptidase 4 inhibitor, FAS full analysis set, GLP-1 RA glucagon-like peptide 1 receptor agonist, MDI multiple daily injections, OAD oral antidiabetic agent
HbA1c Changes
iGlarLixi treatment significantly (p < 0.05) reduced mean HbA1c from baseline to 3 and 6 months in all subgroups, except for the post GLP-1 RA + BI subgroup (Fig. 2a). At 6 months, these significant reductions ranged from 0.47% to 1.27%, with the greatest decreases (> 1.0%) in the post OAD group and the post MDI, bolus insulin (−) group.
Change from baseline in mean glycated haemoglobin (HbA1c) at 3 and 6 months after initiation of insulin glargine/lixisenatide (iGlarLixi) a in the full analysis set and by prior treatment subgroup, b in participants who were previously suboptimally controlled on oral antidiabetic drugs, stratified by whether or not they received dipeptidyl peptidase 4 inhibitors before initiation of iGlarLixi, c in participants who switched from combination therapy of oral antidiabetic drugs and insulin (basal insulin-supported oral therapy), stratified by whether or not they received dipeptidyl peptidase 4 inhibitors before initiation of iGlarLixi; and d in participants who switched from basal insulin-supported oral therapy, stratified by baseline daily basal insulin dose (< 10 U/day vs ≥ 10 U/day). *p < 0.0001, **p < 0.001, †p < 0.05 vs baseline. Error bars show 95% confidence intervals. BI basal insulin, BOT basal insulin-supported oral therapy, DPP-4i dipeptidyl peptidase 4 inhibitor, FAS full analysis set, GLP-1 RA glucagon-like peptide 1 receptor agonist, HbA1c glycated haemoglobin, MDI multiple daily injections, ns not significant when adjusted for baseline HbA1c; diabetes duration and age in a multivariate regression analysis, OAD oral antidiabetic agent
When the post OAD group was stratified by prior DPP-4i use, iGlarLixi treatment significantly decreased mean HbA1c in both groups, at both 3 and 6 months (each p < 0.0001 vs baseline; Fig. 2b, Supplementary Fig. S1a). The changes in HbA1c after 6 months were − 1.28% (95% CI − 1.71, − 0.85) in the post OAD, DPP-4i (+) subgroup and − 1.26% (95% CI − 1.76, − 0.75) in the post OAD, DPP-4i (−) subgroup. After treatment for 3 months, the changes in HbA1c were − 0.94% (95% CI − 1.33, − 0.55) in the post OAD, DPP-4i (+) subgroup and − 1.25% (95% CI − 1.77, − 0.73) in the post OAD, DPP-4i (−) subgroup. In participants post BOT, iGlarLixi treatment significantly decreased HbA1c in both the DPP-4i (+) and DPP-4i (−) subgroups (each p < 0.05 vs baseline; Fig. 2c, Supplementary Fig. S1b). At 6 months, the mean HbA1c reductions were − 0.61% (95% CI − 1.07, − 0.16) in the post BOT, DPP-4i (+) subgroup and − 0.38% (95% CI − 0.72, − 0.04) in the post BOT, DPP-4i (−) subgroup. After adjustment for baseline HbA1c, diabetes duration and age, there were no significant differences between DPP-4i subgroups in HbA1c reduction at 6 months in the post BOT and post OAD groups. HbA1c reductions after 3 months were − 0.52% (95% CI − 0.99, − 0.05) and − 0.31% (95% CI − 0.62, − 0.01) in the respective subgroups. When these participants were stratified by baseline BI dose, 6 months of iGlarLixi treatment significantly reduced mean HbA1c in those who were receiving ≥ 10 U/day (− 0.58%, 95% CI − 0.96, − 0.19, p < 0.05), but not in those who were receiving < 10 U/day (− 0.35%, 95% CI − 0.82, 0.11; Fig. 2d, Supplementary Fig. S1c). HbA1c reductions from baseline to 3 months were not significant in either of these BI dose subgroups.
In the FAS and all but one of the pre-treatment subgroups (post GLP-1 RA + BI), after 3 and 6 months of iGlarLixi treatment there were numerical increases from baseline in the proportion of participants with HbA1c < 7.0% (Table 2). These increases were significant at 3 and 6 months in the FAS (14.4% at 3 months and 18.5% at 6 months; both p < 0.001 vs baseline [5.6%]) and post OAD subgroup (18.6% and 27.9%, respectively; both p < 0.001 vs baseline [0%]), and after 6 months in the post BOT group (10.7%; p < 0.05 vs baseline [3.6%]) and both post MDI subgroups (30.8% and 45.5%, respectively; both p < 0.05 vs baseline [7.7% and 18.2%, respectively]). In the FAS and post OAD subgroup, the proportion of participants reaching their age-specific HbA1c targets increased significantly from baseline to 3 and 6 months after iGlarLixi treatment initiation (Table 2). In the other pre-treatment subgroups, the proportions generally remained similar or increased slightly; however, there were very small participant numbers in each age group.
Body Weight Changes
After iGlarLixi treatment for 6 months, mean body weight decreased significantly in the FAS (− 0.5 kg, 95% CI − 0.80, − 0.16; p < 0.05 vs baseline), the post BOT subgroup (− 1.2 kg, 95% CI − 1.83, − 0.63; p < 0.0001) and both post MDI subgroups (− 1.5 kg, 95% CI –2.79, − 0.29; p < 0.05 and − 1.9 kg, 95% CI − 3.59, − 0.26; p < 0.05), and increased significantly in the post GLP-1 RA subgroup (1.3 kg, 95% CI 0.29, 2.23; p < 0.05); there were no significant changes in the post OAD and post GLP-1 RA + BI subgroups (Fig. 3a). Changes in mean body weight from baseline to 6 months in the post OAD subgroup were non-significant regardless of prior DPP-4i use (− 0.5 kg, 95% CI − 1.46, 0.47 and 0.2 kg, 95% CI − 0.75, 1.15 in those who did and did not have prior use, respectively; Fig. 3b), whereas in the post BOT subgroup, a significant change was observed only in those who had not received DPP-4is (− 1.2 kg, 95% CI − 1.81, − 0.50; p < 0.001; Fig. 3c). When the participants in the post BOT subgroup were stratified by baseline daily BI dose, those who had received ≥ 10 U/day had significant mean reductions in body weight after 6 months (− 1.7 kg, 95% CI − 2.55, − 0.92; p < 0.001), whereas there was no significant change in body weight (− 0.3 kg, 95% CI − 1.07, 0.51) in those who had received < 10 U/day (Fig. 3d).
Change from baseline in mean body weight at 6 months after initiation of insulin glargine/lixisenatide (iGlarLixi) a in the full analysis set and by prior treatment subgroup, b in participants who were previously suboptimally controlled on oral antidiabetic drugs, stratified by whether or not they received dipeptidyl peptidase 4 inhibitors before initiation of iGlarLixi, c in participants who switched from combination therapy of oral antidiabetic drugs and insulin (basal insulin-supported oral therapy), stratified by whether or not they received dipeptidyl peptidase 4 inhibitors before initiation of iGlarLixi; and d in participants who switched from basal insulin-supported oral therapy, stratified by baseline daily basal insulin dose (< 10 vs ≥ 10 U/day). Baseline body weights shown are mean values for each group. Error bars represent 95% confidence intervals (CIs). *p < 0.05, **p < 0.001, ***p < 0.0001 vs baseline. BI basal insulin, BOT basal insulin-supported oral therapy, DPP-4i dipeptidyl peptidase 4 inhibitor, FAS full analysis set, GLP-1 RA glucagon-like peptide 1 receptor agonist, MDI multiple daily injections, OAD oral antidiabetic agent
Dose Changes
The mean (SD) initial daily iGlar dose as a component in iGlarLixi was 8.6 (4.3) U/day in the FAS, and ranged from 5.7 (2.8) to 12.2 (5.2) U/day in the pre-treatment subgroups (Supplementary Table S2). At the end of the study, the mean (SD) iGlar dose ranged from 9.8 (4.7) to 15.2 (4.6) U/day (p < 0.01 vs baseline). In the post OAD and post BOT subgroups, prior DPP-4i use did not alter the mean 6-month iGlar dose (Supplementary Fig. S2). When the post BOT subgroup was stratified by baseline BI dose, the iGlar dose increased significantly (p < 0.01) from initial dose to 6 months in both subgroups (by 2.0 and 3.9 U/day in those taking < 10 and ≥ 10 U/day at baseline, respectively; Supplementary Fig. S2), but the dose at the end of the treatment period was significantly higher in the group that had received ≥ 10 U/day at baseline versus the group that had received < 10 U/day (p < 0.0001).
Amongst participants who were receiving BI at baseline, the mean BI dose was 11.9 U/day in the FAS (as previously discussed in the primary SPARTA analysis [13]) and ranged from 8.9 to 12.2 U/day across applicable subgroups (Supplementary Fig. S3a). After 6 months of iGlarLixi treatment, the mean basal iGlar dose increased significantly in the FAS (by 1.2 U/day, 95% CI 0.5, 1.8; p < 0.001) and the post GLP-1 RA + BI subgroup (by 3.0 U/day, 95% CI 2.0, 4.0; p < 0.001), but did not change significantly in the other subgroups. In the post BOT subgroup, the mean change in BI dose was not affected by prior DPP-4i treatment use (Supplementary Fig. S3b), but the dose at the end of the treatment period was significantly higher in participants with a prior dose of BI of ≥ 10 U/day vs < 10 U/day (Supplementary Fig. S3c). In the subgroup who switched from MDI and continued to receive bolus insulin after initiating iGlarLixi, there was no significant change from baseline in the mean bolus insulin dose (Supplementary Fig. S4).
Safety
In the FAS, the cumulative incidence of hypoglycaemia increased from 7.4% of participants at baseline to 7.7% after 3 months and 14.4% after 6 months of iGlarLixi treatment; the incidence rate increased from 0.3 episodes/person year at baseline to 0.88 and 0.78 episodes/person year at 3 and 6 months, respectively (Table 3). During 6 months of iGlarLixi treatment, the incidence rate of hypoglycaemia was highest in the post MDI, bolus insulin (+) subgroup (increased from 0.62 episodes/person year at baseline to 1.47 and 0.95 episodes/person year at 3 and 6 months, respectively). Hypoglycaemia led to iGlarLixi treatment discontinuation in four participants: two in the post GLP-1 RA subgroup (5.1%) and one each in the post BOT subgroup (1.2%) and the post MDI, bolus insulin (+) subgroup (2.6%).
The 6-month incidence of gastrointestinal events was lowest in the post GLP-1 RA + BI subgroup (three participants, 4.6%), followed by the post GLP-1 RA subgroup (five participants, 12.8%; Table 3). In the other pre-treatment subgroups, the proportion of participants with gastrointestinal events during 6 months of iGlarLixi treatment ranged from 17.9% to 25.6%. Gastrointestinal events led to treatment discontinuation in three participants in the post MDI, bolus insulin (+) subgroup (7.7%), one participant each in the post OAD subgroup (1.2%), the post GLP-1 RA subgroup (2.6%), the post BOT subgroup (1.2%), and the post MDI, bolus insulin (−) subgroup (4.5%), and no participants in the post GLP-1 RA + BI subgroup.
Discussion
Real-world data on the potential effect of previous T2D treatment on the effectiveness and safety of iGlarLixi may be a useful tool in guiding future clinical decision-making. The results of this subgroup analysis showed that in clinical practice in Japan, treatment with iGlarLixi was effective in lowering HbA1c in most T2D pre-treatment subgroups, generally with favourable or minimal impact on body weight. iGlarLixi treatment for 6 months significantly reduced HbA1c from baseline in all but one prior treatment regimen subgroup. In participants in the post GLP-1 RA + BI subgroup, iGlarLixi treatment maintained HbA1c, while reducing the number of daily injections.
The post OAD and post BOT subgroups were further analysed on the basis of prior use of a DPP-4i. In Japan, DPP-4is are widely used [5]. As a result of a lack of clinically significant benefits, combining a DPP-4i and GLP-1 RA is not recommended [15], and typically DPP-4is are discontinued before initiating a GLP-1 RA or fixed-ratio combination containing a GLP-1 RA component. In this study, the analysis of the prior DPP-4i exposure on outcomes was conducted to confirm that switching from a DPP-4i to iGlarLixi does not lead to a deterioration in glycaemic control in clinical practice, and to confirm prior clinical trial data [16]. This analysis showed that prior DPP-4i use did not affect the HbA1c-lowering effect of iGlarLixi, did not negatively affect body weight during iGlarLixi treatment, and did not appear to impact changes in the iGlarLixi dose.
The proportion of participants with HbA1c < 7.0% increased from baseline to 6 months in all but the post GLP-1 RA + BI subgroup, and this increase was significant in all but the post GLP-1 RA subgroup. Furthermore, achievement of the HbA1c target by age group generally showed an increasing trend, with significant increases in the post OAD subgroup.
As insulin treatment carries the risk of increased body weight [17], it is reassuring that in the current analysis, treatment with iGlarLixi for 6 months resulted in significant mean body weight loss in three subgroups (post BOT and both post MDI subgroups, − 1.2 to − 1.9 kg) and minimal, non-significant, body weight changes in two subgroups (post OAD, − 0.2 kg and post GLP-1 RA + BI, + 0.6 kg). Mean body weight increased by 1.3 kg in the post GLP-1 RA subgroup (p < 0.05). The lack of weight variation in the post OAD and post GLP-1 RA + BI subgroups suggests that switching to iGlarLixi may be an optimal treatment choice for lean older individuals, in whom a weight-neutral approach may be preferred when switching treatment [14].
In addition to increasing body weight, insulin treatment is also associated with an increased risk of hypoglycaemia [18], thus the incidence of hypoglycaemia was an exploratory endpoint in SPARTA Japan. In all but one pre-treatment subgroup, the 6-month incidence rate of hypoglycaemia was lower than or similar to that in the FAS, ranging from 0.52 to 0.86 episodes/person year. As may be expected, the incidence rate was higher in the post MDI, bolus insulin (+) subgroup (increased from 0.62 episodes/person year at baseline to 0.95 episodes/person year over 6 months). Of interest, with the exception of participants in the post MDI, bolus insulin (+) subgroup, the incidences of hypoglycaemia with iGlarLixi in the other subgroups were lower or similar to that observed in the three 26-week, open-label clinical trials of iGlarLixi in Japanese individuals with T2D [8, 9, 12], which reported an incidence of symptomatic hypoglycaemia ranging from 13.0% to 18.8%.
Because GLP-1 RAs can be associated with gastrointestinal events, the incidence of these events was also an exploratory endpoint in SPARTA Japan. The proportion of individuals who experienced gastrointestinal events during 6 months of iGlarLixi treatment ranged from 4.6% to 25.6%, and was lowest in the post GLP-1 RA + BI subgroup (three participants, 4.6%), followed by the post GLP-1 RA subgroup (five participants, 12.8%). The most common gastrointestinal events were nausea in three subgroups and constipation in the other three. The number of participants discontinuing iGlarLixi treatment because of gastrointestinal events remained low across subgroups, ranging from none to three participants. As shown with the rates of hypoglycaemia, the incidence of gastrointestinal events observed in this analysis was either lower or similar to that observed in the three clinical trials of iGlarLixi in Japanese individuals with T2D [8, 9, 12], where gastrointestinal events were reported in 26.2% to 33.3% of participants in these trials. However, it should be noted that the incidence of gastrointestinal events may have been underestimated, as participants may have had only transient symptoms that were not reported.
In the post GLP-1 RA + BI subgroup, glycaemic control with iGlarLixi was not associated with a significant improvement; however, the glycaemic control in this subgroup did not deteriorate during iGlarLixi either. This switch was also reasonably well tolerated, with no participants in this subgroup discontinuing treatment because of hypoglycaemia or gastrointestinal events. Thus, switching from GLP-1 RA and BI to iGlarLixi may be a useful option to consider for improving quality of life by reducing the number of injections.
To the best of our knowledge, SPARTA Japan was the largest Japanese real-world study of iGlarLixi treatment, and this subanalysis is the first to explore the impact of prior treatment on the effectiveness and safety of iGlarLixi treatment in Japanese individuals with T2D. Taken together, the results of this subanalysis and the main SPARTA Japan analysis [13] support the findings of the three Japanese randomised clinical trials of iGlarLixi in individuals with T2D [8, 9, 12]. In these 26-week trials, iGlarLixi treatment reduced HbA1c by 1.27% to 1.58%, and the proportion of participants achieving HbA1c < 7.0% ranged from 51.8% to 71.5%. These reductions in HbA1c are similar in magnitude to that observed in the post OAD subgroup of the current analysis (− 1.27%); this subgroup is likely the most comparable with the populations in the clinical trials. However, in the current analysis, the proportion of participants achieving HbA1c < 7.0% (18.5% in the FAS, 5.1–45.5% across subgroups) was lower than that observed in the clinical trials. There are a number of reasons that may explain this difference, including that, unlike the clinical trials, the inclusion criteria in our study did not include an upper limit of baseline HbA1c. Furthermore, as this was an analysis of routine clinical practice, it is possible that there were many cases in whom the appropriate iGlarLixi dose was not achieved on the basis of titration or that the individuals were not specifically targeting an HbA1c < 7.0%. In the current study, the dose was adjusted mostly at the discretion of individual physicians and the final mean iGlarLixi dose ranged from 9.8 to 15.2 dose steps/day across subgroups. In contrast, in the three clinical trials, the dose was uptitrated on the basis of a designated titration algorithm, starting from 5–10 dose steps/day (to a maximum of 20 dose steps/day) until individuals reached a self-monitored blood glucose target, and rescue treatment was implemented if this target was not achieved [8, 9, 12]. Additionally, as SPARTA Japan was a retrospective observational study, the final measurements were not intended exactly at the 6-month time point. In this subanalysis, HbA1c tended to be lower at 6 months than 3 months across subgroups; thus, it is possible that a longer observation period may result in a higher proportion of individuals reaching target HbA1c. In summary, in clinical practice, the absence of a defined treat-to-target algorithm (as used in clinical trials) may result in a lower achievement of HbA1c targets, as observed in this analysis.
Several European real-world studies have assessed the use of iGlarLixi in individuals with T2D [19,20,21]. In an Italian, retrospective 6-month study of 675 participants, iGlarLixi reduced mean HbA1c by 0.77% in the overall population, and by 0.92% in participants treated as per the product label [19], which is consistent with the results of the current subanalysis. Furthermore, the Italian study observed significant reductions in mean body weight from baseline (by 1.2 kg) [19]. In a 24-week prospective Romanian study (N = 901), the proportion of participants achieving HbA1c < 7% with iGlarLixi was 22.6% [21], similar to that observed in the FAS in the current study, while mean body weight was reduced by 1.6 kg [21], which is more than the body weight reductions observed in the current study. In the Romanian study, iGlarLixi was associated with significant HbA1c reductions by 1.3% [21], which is similar to that observed in the Japanese clinical trials. Slightly greater reductions in mean HbA1c from baseline (1.6%) were observed with iGlarLixi over 26 weeks in a real-world prospective study in 353 Hungarian participants; however, a relatively low proportion (20.1%) were receiving insulin-based treatment at baseline [20], which may account for the greater HbA1c reduction. In the Hungarian study, the proportion of participants achieving HbA1c < 7% was 34.8%, and mean body weight decreased significantly by 2.3 kg from baseline [20].
The recent guidelines from the American Diabetes Association and the European Association for the Study of Diabetes [22] place increased focus on both glycaemic control and body weight reduction. They acknowledge that fixed-ratio combinations provide benefits in terms of treatment simplification and have a very high likelihood of achieving glycaemic goals. Such benefits were generally observed in SPARTA Japan across the subgroups assessed. The American Association of Clinical Endocrinologists guidelines [23] specifically recommend fixed-ratio combinations as alternatives to basal bolus insulin therapy; a clinically meaningful reduction of HbA1c accompanied by body weight loss was seen in participants previously on basal bolus insulin therapy in SPARTA Japan.
Although the results of our study may be useful in guiding treatment decisions for Japanese individuals with T2D, the analysis is not without limitations. Firstly, there are a number of limitations associated with the retrospective observational design of SPARTA Japan, including that the participants were not randomised to treatment with iGlarLixi, a number of potential confounders that may have influenced the results were not measured (e.g. comorbidities), and the possibility of physician selection and enrolment bias. Further, there was no comparator treatment, and the stability of previous diabetes treatment was not an inclusion criterion. Secondly, as there were a limited number of participants in each pre-treatment subgroup (ranging from 22 to 86), our results should be interpreted with caution, particularly in analyses in which the subgroups were further divided. Thirdly, participants with no HbA1c measurements at 3 and 6 months were not included in the analysis, meaning the incidence of AEs may have been underestimated. Finally, in SPARTA Japan, only the incidence/rates of gastrointestinal and hypoglycaemia events were assessed; therefore, the current analysis was unable to investigate other aspects of these adverse events, such as their duration.
Conclusions
In routine clinical practice in Japan, 6 months of treatment with iGlarLixi provided improved HbA1c across subgroups of participants who had suboptimal glycaemic control on various prior treatment regimens. Significant reductions in HbA1c were observed in all but one pre-treatment subgroup (i.e. the post GLP-1 RA + BI subgroup). Mean body weight decreased significantly in the FAS and the post BOT and MDI subgroups, but increased in the post GLP-1 RA subgroup. Treatment was generally well tolerated, with few participants discontinuing treatment because of hypoglycaemia or gastrointestinal events.
References
Kohsaka S, Morita N, Okami S, Kidani Y, Yajima T. Current trends in diabetes mellitus database research in Japan. Diabetes Obes Metab. 2021;23:3–18.
Maegawa H, Ishigaki Y, Langer J, Saotome-Nakamura A, Andersen M. Clinical inertia in patients with type 2 diabetes treated with oral antidiabetic drugs: results from a Japanese cohort study (JDDM53). J Diabetes Investig. 2021;12(3):374–81.
Baxter M, Morimoto Y, Tamiwa M, et al. A real-world observational study evaluating the probability of glycemic control with basal insulin or glucagon-like peptide-1 receptor agonist in Japanese patients with type 2 diabetes. Diabetes Ther. 2020;11(7):1481–96.
Draznin B, Aroda VR, American Diabetes Association Professional Practice Committee, et al. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes–2022. Diabetes Care. 2022;45(Suppl 1):S125–43.
Yokoyama H, Araki SI, Yamazaki K, et al. Trends in glycemic control in patients with insulin therapy compared with non-insulin or no drugs in type 2 diabetes in Japan: a long-term view of real-world treatment between 2002 and 2018 (JDDM 66). BMJ Open Diabetes Res Care. 2022;10(3): e002727.
Rosenstock J, Aronson R, Grunberger G, et al. Benefits of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide, versus insulin glargine and lixisenatide monocomponents in type 2 diabetes inadequately controlled on oral agents: the LixiLan-O randomized trial. Diabetes Care. 2016;39(11):2026–35.
Aroda VR, Rosenstock J, Wysham C, et al. Efficacy and safety of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide in type 2 diabetes inadequately controlled on basal insulin and metformin: the LixiLan-L randomized trial. Diabetes Care. 2016;39(11):1972–80.
Kaneto H, Takami A, Spranger R, Amano A, Watanabe D, Niemoeller E. Efficacy and safety of insulin glargine/lixisenatide fixed-ratio combination (iGlarLixi) in Japanese patients with type 2 diabetes mellitus inadequately controlled on basal insulin and oral antidiabetic drugs: the LixiLan JP-L randomized clinical trial. Diabetes Obes Metab. 2020;22(Suppl 4):3–13.
Terauchi Y, Nakama T, Spranger R, Amano A, Inoue T, Niemoeller E. Efficacy and safety of insulin glargine/lixisenatide fixed-ratio combination (iGlarLixi 1:1) in Japanese patients with type 2 diabetes mellitus inadequately controlled on oral antidiabetic drugs: a randomized, 26-week, open-label, multicentre study: the LixiLan JP-O2 randomized clinical trial. Diabetes Obes Metab. 2020;22(Suppl 4):14–23.
Andreozzi F, Candido R, Corrao S, et al. Clinical inertia is the enemy of therapeutic success in the management of diabetes and its complications: a narrative literature review. Diabetol Metabol Syndr. 2020;12(1):52.
Blonde L, Anderson JE, Chava P, Dendy JA. Rationale for a titratable fixed-ratio co-formulation of a basal insulin analog and a glucagon-like peptide 1 receptor agonist in patients with type 2 diabetes. Curr Med Res Opin. 2019;35(5):793–804.
Watada H, Takami A, Spranger R, Amano A, Hashimoto Y, Niemoeller E. Efficacy and safety of 1:1 fixed-ratio combination of insulin glargine and lixisenatide versus lixisenatide in Japanese patients with type 2 diabetes inadequately controlled on oral antidiabetic drugs: the LixiLan JP-O1 randomized clinical trial. Diabetes Care. 2020;43(6):1249–57.
Matsuhisa M, Miyoshi H, Yabe D, Takahashi Y, Morimoto Y, Terauchi Y. Use of iGlarLixi for management of type 2 diabetes in Japanese clinical practice: SPARTA Japan, a retrospective observational study. Diabetes Ther. 2022. https://doi.org/10.1007/s13300-022-01333-w.
Araki E, Goto A, Kondo T, et al. Japanese clinical practice guideline for diabetes 2019. J Diabetes Investig. 2020;11(4):1020–76.
Gallwitz B. Clinical use of DPP-4 inhibitors. Front Endocrinol (Lausanne). 2019;10:389.
Terauchi Y, Yabe D, Kaneto H, et al. Benefits of the fixed-ratio combination of insulin glargine 100 units/mL and lixisenatide (iGlarLixi) in Japanese people with type 2 diabetes: a subgroup and time-to-control analysis of the LixiLan JP phase 3 trials. Diabetes Obes Metab. 2020;22(Suppl 4):35–47.
Russell-Jones D, Khan R. Insulin-associated weight gain in diabetes—causes, effects and coping strategies. Diabetes Obes Metab. 2007;9(6):799–812.
Heller SR, Peyrot M, Oates SK, Taylor AD. Hypoglycemia in patient with type 2 diabetes treated with insulin: it can happen. BMJ Open Diabetes Res Care. 2020;8(1): e001194.
Candido R, Modugno M, Gabellieri E, et al. Efficacy, safety, and appropriateness of iGlarLixi, a fixed-ratio combination (FRC) in type 2 diabetes (T2D) in real-world settings: results from the ENSURE study [abstract 110-LB]. Diabetes. 2021;70(Suppl 1):110-LB.
Kis JT, Nagy G, Kovacs G. Effectiveness of iGlarLixi, a fixed-ratio combination of insulin glargine 100 U/mL and lixisenatide, in people with type 2 diabetes. Diabetes Ther. 2021;12(9):2517–29.
Bala C, Cerghizan A, Mihai BM, Moise M, Guja C. Real-world evidence on the use of a fixed-ratio combination of insulin glargine and lixisenatide (iGlarLixi) in people with suboptimally controlled type 2 diabetes in Romania: a prospective cohort study (STAR.Ro). BMJ Open. 2022;12(5):e060852.
Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753–86.
Blonde L, Umpierrez GE, Reddy SS, et al. American Association of Clinical Endocrinology Clinical Practice Guideline: developing a diabetes mellitus comprehensive care plan-2022 update. Endocr Pract. 2022;28(10):923–1049.
Acknowledgements
Funding
Sponsorship for this study, medical writing assistance, and the journal’s Rapid Service Fee is funded by Sanofi K.K.
Medical Writing, Editorial, and Other Assistance
We would like to thank the following institutions for their involvement in this study: Hamamatsu Medical Center, National Hospital Organization Hyogo-Chuo National Hospital, Medical Corporation Jinnouchi-kai Jinnouchi Hospital, Suzuki Internal Medicine and Diabetes Clinic, Nagoya City University Hospital, Medical Corporation Ayame Medical Clinic, Medical Corporation Kouseikai Iwamoto Internal Medicine Clinic, Primula Clinic, Medical Corporation Towa-kai Kikuchi Medical Clinic, Medical Corporation Hayaishi-kai Hayaishi Hospital, Japan Organization of Occupational Health and Safety, Kansai Rosai Hospital, National Hospital Organization Kure Medical Center and Chugoku Cancer Center, Medical Corporation Omotokai Ohama Dai-ichi Hospital, Medical Corporation Touyukai Kurihara Internal Medicine, Medical Corporation Muraki Internal Medicine and Gastroenterology Clinic, Internal Medicine Kokubo Clinic, General Incorporated Association of Hygiene and Culture Johsai Hospital, Osaka City General Hospital, Medical Corporation Morinoki-kai Morinoki Clinic, Seino Internal Medicine Clinic, Nishikawa Clinic, Social Welfare Organization Saiseikai Imperial Gift Foundation, Shizuoka Saiseikai General Hospital, Jichi Medical University Saitama Medical Center, Social Medical Corporation Shiseikai Inuyama Chuo General Hospital, Miyachi Clinic, Kasugai Municipal Hospital, and the Japan Organization of Occupational Health and Safety, Ehime Rosai Hospital. We also thank the participants who allowed their data to be used in the SPARTA Japan study. Editorial assistance in the preparation of this article was provided by Toni Dando who wrote the outline and first draft of this manuscript on behalf of inScience Communications, Springer Healthcare, and by Kate Palmer of inScience Communications, Springer Healthcare who assisted with post-submission revisions. Support for this assistance was funded by Sanofi K.K.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization: Hideaki Miyoshi, Munehide Matsuhisa, Daisuke Yabe, Yoko Takahashi, Yukiko Morimoto and Yasuo Terauchi; Data acquisition: Yoko Takahashi; Data analysis and interpretation: Hideaki Miyoshi, Munehide Matsuhisa, Daisuke Yabe, Yoko Takahashi, Yukiko Morimoto and Yasuo Terauchi; Writing - review and editing: Hideaki Miyoshi, Munehide Matsuhisa, Daisuke Yabe, Yoko Takahashi, Yukiko Morimoto and Yasuo Terauchi.
Disclosures
Hideaki Miyoshi has received research funding from Mitsubishi Tanabe Pharma Corporation and Taisho Pharmaceuticals; honoraria for lectures from Astellas Pharma, Inc., Eli Lilly Japan, MSD, Kowa Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Sanofi K.K., Sumitomo Dainippon Pharma Co., Ltd., Mitsubishi Tanabe Pharma Co., Novo Nordisk Pharma, Ltd., Nippon Boehringer Ingelheim Co. and Taisho Pharmaceutical Co.; and donations from Ono Pharmaceutical Co., Ltd., Kowa Pharmaceutical Co., Ltd., Abbott Japan Co., Taisho Pharmaceutical Co., Tanabe Pharma Co., Nippon Boehringer Ingelheim Co. and LifeScan Japan Inc. Munehide Matsuhisa has received honoraria from Sanofi K.K., Takeda Pharmaceutical, Eli Lilly Japan, Mitsubishi Tanabe Pharma Corporation, Astellas Pharma, Novo Nordisk Pharma, Ltd., Sumitomo Pharm and MSD; research funding from Sysmex and Nissui; and subsidies or donations from Novartis Pharma, Sanofi K.K. and Novo Nordisk Pharma. Daisuke Yabe has received consulting or speaker fees from Astellas Pharma, Eli Lilly Japan, MSD, Novo Nordisk Pharma, Nippon Boehringer Ingelheim, Ono Pharmaceuticals, Sumitomo Dainippon Pharma Co., Ltd. and Takeda Pharmaceutical; and clinically commissioned/joint research grants from Ono Pharmaceuticals, Novo Nordisk Pharma, Taisho Pharmaceutical, Arklay and Terumo. Yoko Takahashi and Yukiko Morimoto are employees of Sanofi K.K. and may hold shares and/or stock options in the company. Yasuo Terauchi has received honoraria for serving on advisory boards for MSD, Boehringer Ingelheim, Mitsubishi Tanabe Pharma Co., Daiichi Sankyo, Novo Nordisk, Eli Lilly, Sanofi K.K., Astellas Pharma and AstraZeneca; honoraria for lectures from MSD, Ono Pharmaceuticals, Boehringer Ingelheim, Takeda, Mitsubishi Tanabe Pharma Co., Daiichi Sankyo, Sanwa Kagaku Kenkyusho, Novo Nordisk, Eli Lilly, Sanofi K.K., Sumitomo Pharma Co., Ltd., Shionogi, Bayer Yakuhin, Astellas and AstraZeneca; and research funding from MSD, Ono Pharmaceuticals, Boehringer Ingelheim, Novartis, Takeda, Daiichi Sankyo, Novo Nordisk, Eli Lilly, Sanofi K.K., and Sumitomo Pharma Co., Ltd.
Compliance with Ethics Guidelines
Written informed consent for the use of participant data was obtained, and SPARTA Japan was approved by a central ethics committee (Sone Clinic in Tokyo, Japan; on 24 February, 2021) for some institutions and by their own institutional ethics committee in other institutions. Individual institutions and their respective ethics committees are listed in Supplementary Table S1. SPARTA Japan was a retrospective observational study and, as such, compliance with the Declaration of Helsinki 1964 was not required.
Data Availability
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Miyoshi, H., Matsuhisa, M., Yabe, D. et al. Use of iGlarLixi for the Management of Type 2 Diabetes in Japanese Clinical Practice: Prior Treatment Subgroup Analysis of the SPARTA Japan Study. Diabetes Ther 14, 671–689 (2023). https://doi.org/10.1007/s13300-023-01373-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01373-w