Abstract
Introduction
Type 1 diabetes mellitus (T1DM) is characterized by an absolute deficiency of insulin and dependence on insulin therapy. Therefore, glycemic control and management are important for T1DM patients, particularly glycemic variability, which is associated with the development of diabetic complications. However, insufficient attention has been paid to the glycemic variability in T1DM patients so far. Our objective was to identify the effects of food intake on glycemic variability in T1DM patients.
Methods
This was a single-center study that took place in the outpatient clinics of Peking Union Medical College Hospital. A total of 68 Chinese T1DM patients between June 2018 and June 2019 were enrolled. After the baseline demographic and clinical characteristics were evaluated, each participant underwent 14-day flash glucose monitoring (FGM). They recorded caloric intake of breakfast, lunch, and dinner at least 3 days/week using a “Menthol Health” app. After 2 weeks, we obtained the FGM data and did further data analysis. Baseline characteristics and glycemic variability index generated by FGM were compared among groups. A general linear model was used to compare data among groups after adjusting for potential confounding factors. The quantitative relationship between two continuous variables was explored by constructing a linear regression equation.
Results
The results showed that the C-peptide level was independently correlated with the mean of daily differences (MODD) after adjusting for the possible confounders (β = − 0.239, p = 0.046). The dietary nutrition intake had no effect on glycemic variability. However, the nutritional composition of carbohydrate, fat, and protein was an independent risk factor for time spent in hypoglycemia (TBR) post adjustment (β = − 0.213, p = 0.054). However, there was no impact of daily total energy intake on glycemic variability index.
Conclusion
In our study, dietary nutrition intake had no effect on glycemic variability, but residual β-cell function was identified as an influencing factor for glycemic variability in T1DM adults. However, nutritional macronutrient composition played some roles in the occurrence of hypoglycemia. This might provide new evidence for the clinical glycemic control and management of T1DM in the Chinese population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Glycemic control and management have been an important problem for T1DM (Type 1 diabetes mellitus) patients, particularly glycemic variability, which is associated with the development of diabetic complications. However, potential influencing factors for glycemic variability in patients with T1DM were largely unclear. |
We hypothesized that food intake would be important for affecting glucose fluctuation in adults with T1DM. |
What was learned from the study? |
The results showed that C-peptide level rather than food intake was an independent risk factor for glycemic variability in T1DM patients after adjusting for the potential influencing factors. Dietary nutritional composition of carbohydrate, fat, and protein played some role in the occurrence of hypoglycemia. |
This is a pioneering study to investigate the relationship between food intake and glycemic variability in T1DM patients, which provides a new perspective and powerful evidence for better glycemic management in T1DM adults in the future. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13721413.
Introduction
The Ninth International Diabetes Federation (IDF) Atlas reported that there were 463 million diabetes mellitus (DM) adults globally in 2019 [1], among which type1 diabetes mellitus (T1DM) accounted for approximately 10–15% [2]. In China, a large epidemiological study showed that nearly 13,000 patients developed T1DM every year, and 65.3% of them were adults [3]. Another large-scale clinical study done in the Chinese population also validated that the median onset age of T1DM was 27.5 years, with 69.9% of them developing T1DM over 20 years old [4]. Therefore, effective management of T1DM adult patients is important for reducing the social and economic burden and improving health in China.
In the 2020 Standards of Medical Care in Diabetes published by America Diabetes Association (ADA), hemoglobin A1c (HbA1c) was still recommended as the gold standard for assessing blood glucose control in diabetes patients [5]. However, HbA1c only reflects the mean blood glucose level of the most recent 2–3 months but not the current glucose or glucose fluctuations. In T1DM patients, pancreatic β-cell function was impaired and insulin was absolutely scarce, unable to regulate blood glucose accurately. Therefore, glucose variability was generally large and difficult to control. Nowadays, traditional self-monitoring of blood glucose (SMBG) using a glucometer is still the major way to monitor blood glucose levels in diabetes patients [6]. But poor compliance because of pain and discomfort from fingerstick capillary blood sampling, insufficient identification of hyperglycemic or hypoglycemic episodes due to intermittent monitoring, and unreality in recording data limited the values and effects of SMBG in T1DM patients [5].
The invention of continuous glucose monitoring (CGM) made real-time glucose monitoring possible. Flash glucose monitoring (FGM) was a new type of CGM and was brought to the market in 2014 [7]. The sensor can be worn for up to 14 days [8]. This device was more convenient than the traditional CGM system with no requirement of daily capillary blood calibrations [7]. Recent studies have provided evidence for the efficacy and safety of FGM in DM patients [9, 10]. Studies demonstrated that wearing FGM significantly improved the psychological health and life quality, as well as reduced HbA1c and hypoglycemia occurring in T1DM patients [9,10,11,12]. Although the relationship between glycemic variability and chronic complications in T1DM patients has been shown in the published studies, the exact influencing factors of glycemic variability in the T1DM population were largely unclear [13, 14]. This study aims to identify the effects of food intake on glycemic variability in Chinese T1DM adults using FGM, which would provide evidence and targets for better blood glucose control and a further decrease in the development of diabetic complications in T1DM patients.
Methods
Participants
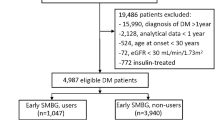
This single-center study took place in the outpatient clinics of Peking Union Medical College Hospital. A total number of 110 Chinese T1DM patients between June 2018 and June 2019 were recruited. All participants provided written informed consent. Eligibility criteria included age at least 18 years old; clinical diagnosis of T1DM, which was in line with the description of T1DM by the World Health Organization (WHO) in 1999; and therapeutic dose of insulin was stable for at least 3 months (dose change less than 10%). Patients with the following conditions were excluded: pregnant women or breastfeeding women; type 2 diabetes mellitus (T2DM) and special types of diabetes; severe liver dysfunction, which presented as alanine transaminase or aspartate transaminase exceeding three times the upper limit of normal range; severe kidney dysfunction, which was defined as creatinine exceeding two times the upper limit of normal range or estimated glomerular filtration rate (eGFR) less than 30 ml/min/1.73 m2; anemia: hemoglobin no greater than 120 g/L in men or no greater than 110 g/L in women; and during the T1DM honeymoon period.
After baseline demographic and clinical characteristics were evaluated, all participants were required to maintain their original insulin regimen and lifestyles, including food intake and exercise. They wore an FGM device (Abbott) to detect glucose levels continuously after collecting baseline vein blood for 14 days. During this period, subjects who recorded their caloric intake of breakfast, lunch, and dinner at least 3 days/week and got effective FGM data more than 10 days were finally included in this study. Seven subjects dropped out because of personal reasons. Thirty-five participants were excluded, nine of which did not finish the 2 weeks of FGM and 26 did not record food intake regularly or donate blood. Therefore, 68 subjects were eventually included in the data analysis (Fig. 1).
The Human Care and Use Committee of the Peking Union Medical College Hospital approved the study protocol (Beijing, China, 13275).
Baseline Characteristics Collection
Baseline demographic and clinical data, including sex, age, time of diagnosis, daily insulin doses, exercise, and oral glucose-lowering medication usages, were collected during first visiting for all patients. Regular exercise was defined as 30 min/day for at least 3 days per week. Participants received a physical examination, such as general conditions, height, weight, and blood pressure (BP), including systolic blood pressure (SBP) and diastolic blood pressure (DBP). Body mass index (BMI) was calculated as weight/height squared (kg/m2). In the meantime, peripheral vein blood was collected to detect glucose and lipid metabolic parameters. Fasting plasma glucose (FPG), total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were analyzed by routine automated laboratory methods (HospitalAU5800, Beckman Coulter, US) in Peking Union Medical College Hospital. HbA1c was assessed by high-performance liquid chromatography (Huizhong MQ-6000, Shanghai, China). Fasting C-peptide (FCP) level was measured by electrochemiluminescence assay (Roche Cobas E602, Shanghai, China). The participants were assigned to two groups based on C-peptide level: detectable C-peptide population (> 0.01 ng/mL) and no detectable C-peptide population (< 0.01 ng/mL).
Diet Records
“Menthol Health” app was used to record participants’ diets for 2 weeks. The recorded content included the types and weight of food eaten that day. The app calculates the total daily caloric intake and the ratio of the three macronutrients. Referring to the Chinese Type 1 Diabetes Diagnosis and Treatment Guidelines (2017), a daily caloric intake between 25 kcal/kg and 30 kcal/kg is appropriate. Therefore, less than 25 kcal/kg was categorized as low calorie intake, whereas more than 30 kcal/kg was defined as high calorie intake. Additionally, the dietary pattern is defined as appropriate if the carbohydrate accounts for 50–60%, the protein 10–20%, and the fat 20–30%. If not, it is defined as inappropriate.
Glucose Monitoring
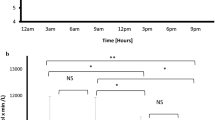
On the same day that HbA1c was detected, participants began to wear the FGM device (Abbott), which is a retrospective CGM system; thus patients cannot obtain the monitored glucose value during this study. The sensor records glucose values once every 15 min, ranging from 2.2 to 27.8 mmol/L. After 2 weeks, the glucose data stored in the sensor were collected. Excluding the data on the first and last day of wearing, the 1152 glucose values for the remaining 12 days were included in the data analysis. Excel and EasyGV Version 9.0 R2 developed by Oxford University were used to calculate parameters related to glycemic variability generated by FGM, including standard deviation (SD), coefficient of variation (CV), mean amplitude of glycemic excursions (MAGE), mean of daily differences (MODD), lability index (LI), continuous overall net glycemic action 1 h (CONGA1), glycemic risk assessment diabetes equation (GRADE), mean absolute glucose (MAG), M value, and J index. According to the Expert Consensus on the Management of Blood Glucose Fluctuations in Diabetic Patients [15], the following are used as normal thresholds: SD < 1.4 mmol/L, MAGE < 3.9 mmol/L, MODD < 0.83 mmol/L. Time above range (TAR) (%) is the percentage of time that blood glucose is greater than 10.0 mmol/L within 24 h. Time below range (TBR) (%) is the percentage of time that blood glucose is less than 3.9 mmol/L within 24 h. Time in range (TIR) (%) is the percentage of time that blood glucose is between 3.9 and 10.0 mmol/L within 24 h.
Statistic Analysis
SPSS 26.0 was used for statistical analysis. The normality of the data was analyzed by Shapiro–Wilk test, and the Leneve test was used to determine the homogeneity of variance. According to the data distribution characteristics, the mean ± standard deviation or the median (quartile 1, quartile 3) is used to describe the data. The data was compared between two groups by the Student t test or Mann–Whitney U test. One-way analysis of variance (ANOVA) or Kruskal–Wallis test was used for comparison among multiple groups. A general linear model was used to compare data among groups after adjusting for potential confounding factors. Categorical variables were reported as percentages (%), and the chi-square test was used for comparison. The quantitative relationship between two continuous variables was explored by constructing a linear regression equation. A two-tailed p < 0.05 is considered statistically significant.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. The Human Care and Use Committee of the Peking Union Medical College Hospital approved the study protocol (Beijing, China, 13275). All subjects provided informed consent to participate in the study.
Results
Demographic Characteristics and Glycemic Variability
A total of 68 T1DM adults were finally enrolled in this study; 34% were male; median age was 35 years (29, 46); and the diabetes duration was 7 years (3, 13). Participants had a median HbA1c (%) of 7.4% (6.3, 8.3) and fasting plasma glucose of 8.1 mmol/L (5.9, 11.4). All patients received insulin treatment, with a median total daily insulin dose of 34 U and 0.58 U/kg. Twenty-five percent took oral glucose-lowering medication, such as metformin and acarbose. These Chinese participants presented an average BMI of 21.5 kg/m2, with normal range of fasting plasma lipid profiles and blood pressure; 79% of the participants did regular exercise more than 30 min/day for at least 3 days each week (Table 1).
In the whole study, FGM showed that the median glucose level of participants was still 8.1 mmol/L (7.0, 9.7), with an elevated SD of 3.3 mmol/L (> 1.4 mmol/L). The glycemic variability indices MAGE 7.6 mmol/L and MODD 3.2 mmol/L were both higher than normal range. General glucose trend results showed that glucose levels were higher than 10.0 mmol/L during a median of 28% of the daily time, while the glucose levels were less than 3.9 mmol/L during 7.6% of the time over 24 h. Although there were no widely accepted threshold values for other glycemic variability indices, including CV, LI, CONGA1, GRADE, MAG, M value, and J index, the results are reported in Table 2.
Glycemic Variability was Different Between Detectable C-peptide Population and No Detectable C-peptide Population in T1DM Patients
It is well known that the C-peptide level is one of the critical factors in reducing blood glucose. To explore whether the C-peptide level affects glycemic variability, we compared the clinical characteristics and glycemic variability between participants with residual β-cell function (C-peptide > 0.01 ng/mL) and no detectable C-peptide population. As shown in Table 1, the median C-peptide concentration was 0.29 ng/mL (0.12, 0.56) in T1DM adults with residual β-cell function. The baseline characteristics were almost comparable between the two groups, while the T1DM duration was shorter (3 years (1, 8)) in the detectable C-peptide group compared with those without residual β-cell function (10 years (6, 18)) (p < 0.001) and insulin doses also tended to be lower (0.55 U/kg vs. 0.59 U/kg) (p = 0.052).
Although no significant difference was observed in mean glucose level (p > 0.05), the FGM data showed smaller glycemic variability in T1DM patients with residual β-cell function (Table 2). Specifically, after adjustment for sex, age, BMI, duration, FPG, HbA1c, daily insulin dose, exercise, and oral medication, MODD and MAG were both significantly lower in detectable C-peptide patients than those in T1DM without residual β-cell function (p = 0.031 and p = 0.037, respectively) (Table 2).
Daily Caloric Intake had No Effect on Glycemic Variability in T1DM Patients
Caloric intake was another impacting factor for energy metabolism. The mean daily caloric intake was 23.9 ± 6.5 kcal/kg and the median total caloric intake was 1363.7 kcal (1185.7, 1595.5) in the whole population. On the basis of the Chinese Type 1 Diabetes Diagnosis and Treatment Guidelines recommendation, we divided T1DM patients into a low-calorie group (19.7 kcal/kg), modest-calorie group (27 kcal/kg), and high-calorie group (34.9 kcal/kg). There were no differences in the nutritional composition (carbohydrate, protein, and fat) among these three groups. The baseline characteristics showed that patients with high caloric intake had significantly higher TC level than those in the low-calorie group (p < 0.05), whereas the participants with low caloric intake presented with higher systolic and diastolic blood pressure than those of T1DM adults and modest caloric intake (p < 0.05). However, they did not differ in age, sex, duration of T1DM, HbA1c, FPG, FCP, daily insulin dose, lipid profiles, and exercise (p > 0.05) (Table 3). Surprisingly, when it comes to FGM data, after adjustment for the potential confounding factors, including sex, age, BMI, duration, SBP, DBP, FPG, HbA1c, TC, LDL-C, FCP, daily insulin dose, exercise, and oral medication, the three groups presented with comparable mean glucose levels (MG) and glycemic variability (SD, CV, MAGE, MODD, TIR, TBR, TAR, GRADE, J index, CONGA1, LI, M value, and MAG) (p > 0.05) (Table 4).
Dietary Nutrient Composition Affected Blood Glucose in T1DM Patients
Although the groups with different amounts of daily caloric intake showed no differences in glycemic variability, we evaluated the effects of nutritional composition on glucose variability. The participants were assigned into two groups according to the dietary pattern recommendation by the Chinese Type 1 Diabetes Diagnosis and Treatment Guidelines. Twenty-three patients were included in the appropriate nutrition group, while 45 had inappropriate nutrition intake. However, the daily caloric intake between the two groups was comparable (p > 0.05). The patients in the appropriate nutrition group ate significantly more carbohydrate (55.7%) and less fat (27.3%) than those in the inappropriate nutrition group (49.3% and 33%, respectively) (p < 0.001). But the protein intake was comparable between the two groups (p > 0.05). Other demographic and clinical data were all matched between the two nutritional groups (Table 5). As for the mean glucose level monitored by FGM, the two groups did not differ after adjustment for the potential influencing factors (p > 0.05). Interestingly, the group with appropriate nutrition intake spent less time in hypoglycemia (< 3.9 mmol/L) (4.4%) compared with those in the inappropriate nutrition group (9.7%) (p = 0.046) (Table 6).
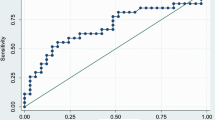
C-peptide and Nutritional Composition were Independent Risk Factors for Glycemic Variability and Blood Glucose Distribution but Not Mean Glucose Levels
Finally, we evaluated the relationship between FCP, daily caloric intake, nutritional composition as well as MG, and glycemic variability and glucose distribution (Table 7). All the three factors did not affect the mean glucose level of 2-week FGM after adjusting for age, sex, BMI, duration, HbA1c, daily insulin doses, oral medication use, and exercise. However, when it comes to the glycemic variability, FCP was considered an independent influencing factor for MODD (β = − 0.239, p = 0.046) after adjustment for the age, sex, BMI, duration, HbA1c, daily insulin doses, daily caloric intake, nutritional composition, oral medication use, and exercise. The daily caloric intake had no relationship with glycemic variability. But the nutritional composition tended to independently decrease the time spent in hypoglycemia (TBR) after adjusting for the possible confounding factors (β = − 0.213, p = 0.054).
Discussion
In this study, we found that daily nutrition intake had no effect on glucose variability in T1DM adults, but C-peptide level was an influencing factor for glycemic variability independent of mean blood glucose level. However, nutritional composition of carbohydrate, fat, and protein affected the occurence of hypoglycemia.
Insulin secreted by β-cells was absolutely insufficient in T1DM patients, resulting in impaired glycemic regulation and relatively large glycemic variability [13]. However, the glycemic variability was intimately correlated with the development of diabetic complications [14]. Therefore, reducing the glucose variability, not only the HbA1c level, would have great clinical significance for combating the complications and mortality of T1DM patients. In this study, the median duration of T1DM was 7 years among the participants and the median HbA1c was 7.4%, which was higher than the goal of 7% recommended by ADA. Another glycemic assessment target was TIR in patients wearing a CGM sensor. The 2020 Standards of Medical Care in Diabetes published by ADA recommended TIR as an acceptable endpoint for clinical trials to evaluate the glycemic control with a goal of 70% TIR aligning with an HbA1c of approximately 7% [5]. In accordance with HbA1c, the TIR (61.0%) was less than the glycemic goal. Therefore, the glycemic control was substandard in more than half of the T1DM patients in this cohort. Additionally, the glycemic variability indices, such as SD, MAGE, MODD, were all higher than values recommended by the Expert Consensus on the Management of Blood Glucose Fluctuations in Diabetic Patients [15]. Large glucose variability has been considered a common problem in the blood glucose management of T1DM patients supported by another two published retrospective studies [16, 17], which calls for more attention and positive control of glycemic variability.
Uncovering the etiology and pathogenesis of glycemic variability in T1DM would help a lot in the improvement of glucose control. MODD and MAG were both significantly lower in the detectable C-peptide group compared with those of the no detectable C-peptide population after adjustment for sex, age, BMI, duration, FPG, HbA1c, daily insulin dose, exercise, and oral medication, although MG level was comparable between the two groups. This indicated that the residual β-cell function may not act on reducing blood glucose by secreting insulin but on maintaining glucose stability. It has been shown that the lost effects of endogenous insulin secretion on pancreatic α-cells may lead to loss of the regulatory response of glucagon to hypoglycemia [18]. Therefore, lower glycemic variability in patients with detectable C-peptide may be associated with glucagon’s regulatory response. In light of the importance of residual β-cell function in controlling glycemic variability, T1DM management should be strengthened as soon as possible, as this was indicated as the mere strategy to delay the decline in C-peptide levels caused by the extension of the disease duration [19], thereby improving glycemic variability.
Surprisingly, our study showed that total energy intake was not correlated with glycemic variability in T1DM patients after adjusting for the potential confounders. A large number of studies have provided evidence for the relationship between energy intake and glycemic control in the diabetic population [20,21,22,23], in which caloric restriction had beneficial effects on blood glucose control [24, 25]. A previous study also explored the relationship between meal timing, meal frequency, breakfast consumption habits, and glycemic control (HbA1c) in T1DM patients, who were enrolled in the Finnish Diabetic Nephropathy Study [26]. They uncovered the association between consumption of breakfast as well as multiple smaller meals and good glycemic control in T1DM adults, whereas the increased number of meals might elevate glycemic variability. Another study assessed the effects of skipping breakfast on the average, SD, and CV of HbA1c levels in T2DM patients and showed that skipping breakfast was independently associated with not only poor glycemic control but also with large glycemic variability [27]. However, the published studies did not accurately evaluate the effects of energy intake on glycemic variability. To the best of our knowledge, this is the first study to explore the relationship between total caloric intake and glycemic variability in T1DM adults using FGM. Our results suggest that daily energy intake had no effect on glycemic variability in T1DM, but this needs further validation in large cohorts.
Eating is one of the most challenging parts for doctors to determine the treatment plan for diabetic patients. In addition to total caloric intake, nutritional composition, particularly macronutrients, also has a great impact on metabolism [28, 29]. In recent years, healthy eating patterns recommended in research, including the Mediterranean-style [30, 31], low-carbohydrate [32, 33], and vegetarian or plant-based eating patterns [34, 35], were all shown to be beneficial to health. Nevertheless, the Standards of Medical Care in Diabetes published by ADA in 2020 suggested that there is no “one-size-fits-all” percentage of calories from carbohydrate, protein, and fat for diabetes patients on the basis of previously published evidence [36]. Therefore, they recommended individualized assessment of current eating patterns, preferences, and metabolic goals to determine the macronutrient distribution for diabetes patients. The Chinese Type 1 Diabetes Mellitus Diagnosis and Treatment Guidelines recommended 50–60% of carbohydrate, 10–20% of protein, and 20–30% of fat in Chinese T1DM patients. In this study, we found that patients with eating patterns in accordance with this guideline recommendation spent less time in hypoglycemia (< 3.9 mmol/L) but did not increase hyperglycemia time nor mean blood glucose level. The average carbohydrate caloric proportion was 55.7%, protein 27.3%, and fat 17.1% compared with 49.3%, 33.0%, and 18.0%, respectively, in those with inappropriate nutrition intake. Therefore, this macronutrient distribution is appropriate for Chinese T1DM adults to reduce the incidence of hypoglycemia. But this discovery also requires more validation in large cohorts and animal models.
Conclusion
Overall, we demonstrated that residual β-cell function independently affected glycemic variability in Chinese T1DM adults rather than daily nutrition intake. Dietary macronutrient composition plays some roles in the occurrence of hypoglycemia. However, we acknowledge several limitations in this study. First, the sample size was relatively small and we require large cohorts to verify these preliminary findings. Additionally, this was an observational study and only the relationship was analyzed. More prospective and randomized clinical trials are called for to clarify these associations. Finally, the food intake was self-recorded in this study; thus there might be reporting bias. Nevertheless, this is a pioneering study to investigate the relationship between dietary total energy as well as macronutrient composition and glycemic variability in T1DM patients, which provides a new perspective and powerful evidence for better glycemic management in T1DM adults in the future.
References
International Diabetes Federation. IDF Atlas 9th edn. Brussels: IDF; 2019.
Katsarou A, Gudbjörnsdottir S, Rawshani A, et al. Type 1 diabetes mellitus. Nat Rev Dis Primers. 2017;3:17016.
Weng J, Zhou Z, Guo L, et al. Incidence of type 1 diabetes in China, 2010–13: population based study. BMJ. 2018;360:j5295.
Yang D, Deng H, Luo G, et al. Demographic and clinical characteristics of patients with type 1 diabetes mellitus: a multicenter registry study in Guangdong, China. J Diabetes. 2016;8:847–53.
Targets G. Standards of Medical Care in Diabetes–2020. Diabetes Care. 2020;43:S66-s76.
Danne T, Nimri R, Battelino T, et al. International consensus on use of continuous glucose monitoring. Diabetes Care. 2017;40:1631–40.
Heinemann L, Freckmann G. CGM versus FGM; or, continuous glucose monitoring is not flash glucose monitoring. J Diabetes Sci Technol. 2015;9:947–50.
Wright LA, Hirsch IB. Metrics beyond hemoglobin A1C in diabetes management: time in range, hypoglycemia, and other parameters. Diabetes Technol Ther. 2017;19:S16-s26.
Dover AR, Stimson RH, Zammitt NN, Gibb FW. Flash glucose monitoring improves outcomes in a type 1 diabetes clinic. J Diabetes Sci Technol. 2017;11:442–3.
Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet. 2016;388:2254–63.
Ólafsdóttir AF, Attvall S, Sandgren U, et al. A clinical trial of the accuracy and treatment experience of the flash glucose monitor freestyle libre in adults with type 1 diabetes. Diabetes Technol Ther. 2017;19:164–72.
Ish-Shalom M, Wainstein J, Raz I, Mosenzon O. Improvement in glucose control in difficult-to-control patients with diabetes using a novel flash glucose monitoring device. J Diabetes Sci Technol. 2016;10:1412–3.
Gorst C, Kwok CS, Aslam S, et al. Long-term glycemic variability and risk of adverse outcomes: a systematic review and meta-analysis. Diabetes Care. 2015;38:2354–69.
Lachin JM, Bebu I, Bergenstal RM, et al. Association of glycemic variability in type 1 diabetes with progression of microvascular outcomes in the diabetes control and complications trial. Diabetes Care. 2017;40:777–83.
Beck RW, Bergenstal RM, Cheng P, et al. The relationships between time in range, hyperglycemia metrics, and HbA1c. J Diabetes Sci Technol. 2019;13:614–26.
El-Laboudi AH, Godsland IF, Johnston DG, Oliver NS. Measures of glycemic variability in type 1 diabetes and the effect of real-time continuous glucose monitoring. Diabetes Technol Ther. 2016;18:806–12.
Dadlani V, Tamhane SU, Sun A, et al. High glucose variability in hospitalized patients with type 1 diabetes mellitus. Diabetes Technol Ther. 2017;19:572–9.
McCrimmon RJ, Sherwin RS. Hypoglycemia in type 1 diabetes. Diabetes. 2010;59:2333–9.
The Diabetes Control and Complications Trial Research Group. Effect of intensive therapy on residual beta-cell function in patients with type 1 diabetes in the diabetes control and complications trial. A randomized, controlled trial. Ann Intern Med. 1998;128:517–23.
Dubé MC, Prud’homme D, Lemieux S, Lavoie C, Weisnagel SJ. Relation between energy intake and glycemic control in physically active young adults with type 1 diabetes. J Sci Med Sport. 2014;17:47–50.
Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 2014;383:1999–2007.
Ojo O. Dietary intake and type 2 diabetes. Nutrients. 2019;11:2177.
Kang HM, Kim DJ. Total energy intake may be more associated with glycemic control compared to each proportion of macronutrients in the Korean diabetic population. Diabetes Metab J. 2012;36:300–6.
Carter S, Clifton PM, Keogh JB. Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: a randomized noninferiority trial. JAMA Network Open. 2018;1:e180756.
Zubrzycki A, Cierpka-Kmiec K, Kmiec Z, Wronska A. The role of low-calorie diets and intermittent fasting in the treatment of obesity and type-2 diabetes. J Physiol Pharmacol. 2018;69(5):663–83.
Ahola AJ, Mutter S, Forsblom C, Harjutsalo V, Groop PH. Meal timing, meal frequency, and breakfast skipping in adult individuals with type 1 diabetes - associations with glycaemic control. Sci Rep. 2019;9:20063.
Hashimoto Y, Kaji A, Sakai R, et al. Skipping breakfast is associated with glycemic variability in patients with type 2 diabetes. Nutrition. 2020;71:110639.
Parry SA, Hodson L. Influence of dietary macronutrients on liver fat accumulation and metabolism. J Investig Med. 2017;65:1102–15.
Alferink LJ, Kiefte-de Jong JC, Erler NS, et al. Association of dietary macronutrient composition and non-alcoholic fatty liver disease in an ageing population: the Rotterdam Study. Gut. 2019;68:1088–98.
Jennings A, Berendsen AM, de Groot L, et al. Mediterranean-style diet improves systolic blood pressure and arterial stiffness in older adults. Hypertension. 2019;73:578–86.
Garcia M, Bihuniak JD, Shook J, et al. The effect of the traditional Mediterranean-style diet on metabolic risk factors: a meta-analysis. Nutrients. 2016;8:168.
Shai I, Schwarzfuchs D, Henkin Y, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. New Eng J Med. 2008;359:229–41.
Hall KD, Chung ST. Low-carbohydrate diets for the treatment of obesity and type 2 diabetes. Curr Opin Clin Nutr Metab Care. 2018;21:308–12.
Dinu M, Abbate R, Gensini GF, Casini A, Sofi F. Vegetarian, vegan diets and multiple health outcomes: a systematic review with meta-analysis of observational studies. Crit Rev Food Sci Nutr. 2017;57:3640–9.
Lynch H, Johnston C, Wharton C. Plant-based diets: considerations for environmental impact, protein quality, and exercise performance. Nutrients. 2018;10:1841.
American Diabetes Association. 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes–2020. Diabetes Care. 2020;43:S48–S65.
Acknowledgements
We thank the participants of the study.
Funding
This work was supported by the grants from National Natural Science Foundation of China (Nos. 81870579, 81870545, 81570715, 81170736), which supported the rapid service fee of this journal.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
All authors have no financial or other potential conflict of interest to disclose.
Compliance with Ethics Guidelines
This study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. The Human Care and Use Committee of the Peking Union Medical College Hospital approved the study protocol (Beijing, China, 13275). All subjects provided informed consent to participate in the study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhou, L., Deng, M., Zhai, X. et al. The Effects of Dietary Nutrition Intake on Glycemic Variability in Type 1 Diabetes Mellitus Adults. Diabetes Ther 12, 1055–1071 (2021). https://doi.org/10.1007/s13300-021-01028-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01028-8