Abstract
Introduction
Hypoglycemia leading to hospitalization is associated with adverse economic outcomes, although the real burden is unknown. The HIPOS-WARD (Hypoglycemia In Portugal Observational Study-Ward) aimed to characterize ward admissions due to hypoglycemia episodes in treated patients with diabetes and assess their economic impact to the National Health System.
Methods
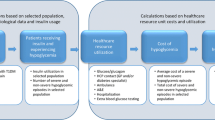
Observational, cross-sectional study, conducted in 16 Portuguese centers for 22 months. The applied microcosting approach was based on healthcare resource data, collected from patients’ charts upon ward admission until discharge, and unitary costs from official/public data sources. Absenteeism was also estimated for active workers on the basis of the human capital approach.
Results
Of the 176 patients with diabetes mellitus enrolled, 86% had type 2 diabetes. Half of the patients (50.0%) were on insulin-based therapy, followed by 30.1% on a secretagogue-based regimen, 9.7% on non-secretagogue therapy, and 10.2% on a combination of insulin and secretagogue. Overall mean costs per patient were medication, 45.45 €; laboratory analysis, 218.14 €; examinations, 64.91 €; physician and nurse time, 268.55 € and 673.39 €, respectively. Bed occupancy was the main cost driver (772.09 €) and indirect cost averaged 140.44 €. Overall, the cost per hypoglycemia episode leading to hospitalization averaged 2042.52 € (range 194.76–16,762.87 €). Patients treated with insulin-based regimens (2267.76 €) and type 2 diabetes (2051.29 €) had the highest mean costs. The mean cost increased with repeated hypoglycemic events (2191.67 €), correlated complications (2109.26 €), and death (5253.38 €).
Conclusion
HIPOS-WARD’s findings confirm and support both the substantial clinical and economic impact of hospitalization due to hypoglycemia in Portugal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hypoglycemia events related to antidiabetic treatment are one of the most frequent adverse events, and also expected to be costly once they usually require hospitalization. Therefore, there is general concern when managing patients with diabetes mellitus (DM) in terms of clinical, humanistic, and economic aspects. |
Knowledge on the real economic burden of hypoglycemic events during DM treatment is still scarce. Thus, this paper aims to present the economic impact of managing the hypoglycemic events leading to hospitalization in the scope of DM control. |
For informing healthcare-related decision-making: this paper may highlight the importance to guide the DM disease management on the prevention of the hypoglycemic event, aiming to successfully reduce the costs associated with hospital admissions. |
Introduction
Uncontrolled diabetes mellitus (DM) is characterized by deviations in insulin secretion/action, affecting glucose metabolism with important consequences for the patient’s overall health and quality of life. DM is a major cause of cardiovascular events, being often associated with premature death [1, 2]. Type 1 DM (DM1) is an autoimmune variation that mostly affects the young, while type 2 DM (DM2) is the most frequent subtype (90%), commonly associated with unhealthy lifestyles and genetic and socioeconomic factors [3].
There were an estimated 425 million cases of DM worldwide in 2017, with an expected increase up to 629 million by 2045 due to the continuous rise in prevalence. The economic healthcare burden incurred for patients with DM expected for 2045 (USD 625 billion) was already surpassed in 2017 (ca. USD 727 billion). Therefore, DM is considered one of the main public health issues, affecting both patients’ health and governments’ healthcare budgets [3, 4].
To avoid micro- and macrovascular complications, international and national guidelines usually recommend lowering hemoglobin A1c (HbA1c) to less than 7.0% for most patients with DM through lifestyle management and, when necessary, pharmacological therapies [5,6,7]. Hypoglycemia events are one of the most frequent antidiabetic drug-related adverse events [8, 9] and usually the most common endocrine emergency leading to hospitalization [10,11,12,13,14]. Consequentially, there is great concern regarding the risk of hypoglycemia events during the metabolic control of patients with DM1 and DM2.
In 2015, a prevalence of 13.3% and an incidence of 699.5/100,000 habitants were estimated for patients with DM aged from 20 to 79 years in Portugal. This disease was responsible for 4.0% of all-cause deaths in that year. DM is a main cause of hospitalization (16%), with a mean duration of 3.4 days (or 11.6 days, excluding day-care episodes), which is more than the average duration of general hospitalization causes in the Portuguese National Health System (NHS) [15].
Despite the considerable and increasing burden of DM for the NHS, national data on hospital admissions due to hypoglycemia are scarce, hindering successful disease management and prevention of adverse events.
HypoglycemIa in POrtugal Study (HIPOS) was a sequence of three observational studies to capture the overall panorama of hypoglycemia events in Portugal in different settings of healthcare assistance: ambulatory (HIPOS-PHARMA) [16], emergency room (HIPOS-ER) [17], and hospitalizations (HIPOS-WARD). Their main objective was to assess the clinical characteristics of patients with DM enrolled by type of admission, and the resource consumption and corresponding costs were estimated as secondary objectives. In HIPOS-PHARMA, the application of a self-administered questionnaire investigated patients’ awareness and knowledge about hypoglycemia and associated symptoms, in addition to previous information provided by healthcare professionals. In HIPOS-ER, patients’ characteristics and hypoglycemia episode data were collected in the scope of emergency department attendance, leading or not to hospitalization. The economic consequences of severe hypoglycemia episodes were demonstrated once 44.1% of enrolled patients were hospitalized, with a mean cost of 2880 € per case [18].
Considering the well-recognized economic impact of managing hypoglycemic events leading to hospitalization, this manuscript focuses on the economic data from HIPOS-WARD, aiming to describe the resource consumption and calculating the overall direct and indirect costs associated with hypoglycemic events in patients with DM treated with antihyperglycemic agents (AHA) in a ward setting.
Methods
Study Design and Patient Population
HIPOS-WARD was an observational, cross-sectional, nationwide study conducted between November 2016 and August 2018. The study was approved by the ethics committees of each participating center (Supplementary Material) and by the National Committee for Data Protection. All procedures were conducted in accordance with the Declaration of Helsinki and the Good Pharmacoepidemiology. All participants of the study or their legally acceptable representative signed an informed consent form, which adhered to IRB/ERC requirements, applicable laws and regulations, and sponsor requirements.
The hypoglycemia event was defined on the basis of the modified Whipple’s triad (signs and symptoms suggestive of hypoglycemia reverted with carbohydrates or glucagon, and a blood glucose level below 70 mg/dL measured by venous, arterial, or capillary samples) [19]. The hypoglycemic events were considered when they occurred while the patient was already at the hospital or admitted to the emergency room (ER) as the primary reason, and led to hospitalization (internal medicine or endocrinology wards). Hospitalization is defined as a ward admission period of at least 24 h from diagnosis [20].
Data Collection and Statistical Analysis
Socioeconomic and anthropometric data, diabetes characteristics (DM type, antidiabetic treatment, comorbidities, and medical history), and patients’ hypoglycemia literacy were collected by the study investigator through a specific questionnaire at ward admission. Data on hospitalized hypoglycemia episodes, such as characterization, evaluation, and resource consumption, were collected from patients’ clinical records from the ward admission to discharge or until death. These data included the length of stay, time spent by the physician and nurse (per day), administered drugs, laboratory tests, and examinations performed during hospitalization period. Since data collection was mainly based on hospital database, absenteeism was estimated in an exploratory manner and is presented separately from main analysis.
As defined per protocol AHA subgroups are (a) insulin based when treated with insulin as monotherapy; (b) secretagogue based when treated with sulfonylurea and/or meglitinides; (c) non-secretagogue based when treated with other drugs such as metformin, acarbose, glitazones, dipeptidyl peptidase 4 (DPP4) inhibitors, glucagon-like peptide 1 (GLP1) agonists, sodium/glucose cotransporter 2 (SGLT2) inhibitors); and (d) combined therapy group if both insulin and secretagogue therapy are used in association. Table S1 (Supplementary Material) describes the study procedures per visit and inclusion/exclusion criteria.
Data discrepancies were replaced with uniformized mean data from other enrolled patients (excluding outliers), or by considering label information (posology) and pharmacologic plausibility. Very poor registries, associated with huge uncertainty, were unconsidered. Regarding direct costs, only those supported by the NHS were assessed.
Qualitative variables are summarized as counts (n) and percentages (%), while quantitative variables are summarized as mean, median, standard deviation (SD), and range (minimum and maximum), considering a significance level of 5%. Statistical analysis was carried out with SAS® version 9.4 (SAS Institute Inc., Cary, NC, USA; 2014).
Cost Calculations
A microcosting approach was used to identify the complete cost structure of managing a hypoglycemic episode in the ward considering patient-level data on resources consumption and unitary costs (in euros, 2018), extracted from Portuguese official/public sources. Products of unitary costs and resource consumption were summed to estimate the total cost per category. Overall cost for hospitalization due to hypoglycemia episodes included direct medical cost (e.g., drugs, laboratory tests, examinations, healthcare professional fees) and non-medical costs (e.g., bed occupancy cost). The time spent by physician/nurse to manage hypoglycemic episodes was multiplied by the hourly rates from official yearly income tables of local syndicates: €20.87 and €13.35 for physicians and nurses, respectively [21, 22].
For medication cost, the acquisition prices from public hospitals’ contracts or, if not available, the corresponding reimbursement percentage of outpatient prices supported by the Portuguese NHS were used as a proxy [23, 24]. Whenever several brands were available for the same medication, the less costly for the most suitable presentation was considered.
The cost of laboratory analysis/other examinations was estimated by multiplying the number of examinations performed by the corresponding unitary cost from the Diagnosis-Related Groups (DRG) prices table published by the local authorities [25].
Standardized occupancy cost was calculated by subtracting the medical direct cost from the total cost of bed occupancy per hospital unit published on the 2009 Accountancy Portuguese Hospitals database [26]. This approach assumes that resulting costs correspond to the administrative services and maintenance of bed occupancy attributed to patient admission (i.e., laundry; meals, etc.). The resulting cost was then divided by the average number of days of occupancy registered in the database and multiplied by the length of stay of each episode per ward unit. Whenever a patient was hospitalized in more than one department/unit, costs were summed up considering the time spent on each department.
Absenteeism was considered from ER admission, hospital and home stay post-discharge for both patients and caregivers, as patients with DM are mostly retired and require the assistance of family members [17, 18].
Indirect cost was calculated on the basis of the human capital approach, which was applied considering productivity loss of active workers and the official Portuguese wage tables by gender and age group from the National Institute of Statistics [27]. To estimate the daily labor costs for employers, the monthly net wages from the private sector were grossed up by the social security contributions and income taxes. The Portuguese standard vacation and Christmas bonus monthly pay were also taken into consideration, while weekends and official holidays were excluded [28]. This was then multiplied by the number of absent days due to hypoglycemia episodes reported from ER attendance to the post hospitalization period. As a conservative approach, no productivity loss cost was attributed to life years lost for the only active worker that died.
Finally, to explore beyond the data collected, and despite the loss in statistically robustness due to a smaller sample size, subgroup analyses were performed, namely costs per gender and age groups; per DM type; and per AHA group. The hypothesis that patients previously exposed to a hypoglycemic event would have higher costs in the subsequent episode was also tested by comparing the cost of the current event of this subpopulation versus the cost of patients who had never experienced such an event. The previous episode cost was not included.
Results
A total of 176 patients were enrolled from 18 wards of 16 public hospitals integrated in the NHS in Portugal.
Sociodemographic and Disease Characteristics
Mean patient age was approximately 72 years (range 28–98 years) and 55.1% of the patients were female. Around half of the patients were married (56.6%) and most patients were retired (73.1%). Only 16 patients (9.2%) were active workers, 8.6% being in full-time work and 0.6% in part-time work.
Type 2 was the most frequent DM type (86.4%), followed by DM1 (10.2%). At study inclusion, half of the patients (50.0%) were on insulin-based therapy, 30.1% on a secretagogue-based regimen, 9.7% on non-secretagogue drug-based therapy, and 10.2% on a combination of insulin and secretagogue. At ward admission, or at the previous ER triage (when no data available), the HbA1c mean value was 7.3% (range 4.0–27.0%) and the lowest value of glycemia was 45.70 (range 9.00–298.00). Most of the patients had at least one complication due to DM at baseline: 50% of patients had eye complications, 26.1% had neuropathy, and 47.4% had nephropathy. Patients’ clinical characterization, also per subgroup, will be published elsewhere.
Hypoglycemic Event Characterization
Fifty-eight patients confirmed having experienced hypoglycemia events in the previous 12 months, of which 38 occurred in the last 30 days, 21 resulted in therapy changes, and 10 led to hospitalization. Hypoglycemia was the main cause of hospitalization (71.4% of patients) with internal medicine being the most common ward unit at which patients were admitted (87.4%). A median of 2.0 recurrent hypoglycemic episodes occurred for 36.0% of patients during hospitalization. Although none of these led to further complications, 23 patients (13.1%) were transferred to another ward unit. After discharge, most patients returned home (64.2%) and 8 patients (4.5%) died. Table 1 summarizes patient, disease, and hypoglycemic event characteristics.
Healthcare Resource Consumption
During hospitalization, almost all patients (92%) required at least one drug/IV solution, with the most frequent being NaCl 0.9% (45.7%) and insulin (31.5%). Examinations and laboratory analyses were performed on 80.1% and 99.4% of patients, respectively. The most commonly performed examinations were the electrocardiogram (EGC) and the simple X-ray, while the capillary glycemia was the most frequent assessment per patient (median of 27 times). On average, patients spent 13.3 h in the ER department and 9.2 days in the ward department, including the average of 4.3 days in the secondary ward unit, when necessary. Regarding medical time of assistance, physicians and nurses spent on average 12.3 h and 49.5 h monitoring patients’ evaluation, respectively.
Eighty-one percent (n = 13) of the 16 active workers patients reported work absence. These patients had a mean age of 49 years (range 28–74 years), 77% were male and belonged to the insulin-based therapy group. A mean of 3.08 absent days was observed from ER admission to ward admission (range 0–19 days) and 8.77 days from ward admission to discharge (range 1–31 days). Family members’ absenteeism was considered underreported (only 1 case was registered) and was thus excluded from the analysis as outlier. Healthcare resource consumption is summarized in Table 2.
Direct Costs per Hospitalization Episode
Most patients (n = 162; 92%) had medication costs and a mean of 5.70 drugs/patient was administered. Per episode, the average medications cost was 45.45 € (maximum 704.58 €), 218.14 € was spent on laboratory analyses (maximum 1720.43 €), and 64.91 € on examinations (maximum 355.17 €). The mean cost per episode associated with physician and nurse attendance was 268.55 € (maximum 8403.83 €) and 673.39 € (maximum 5843.60 €), respectively. The mean standardized occupancy cost was 772.09 € per episode (maximum 5708.56 €). On average, the total direct cost per episode was 2042.52 €, ranging from 1551.47 € in the secretagogue-based therapy group to 2267.76 € in the insulin-based group.
Indirect Costs Due to Absenteeism
Assuming a null indirect cost for all non-active workers, a mean wage/day of 117.24 € was estimated by the human capital approach, resulting in an average indirect cost of 140.44 € (maximum 6296.26 €). This cost increases to 1901.31 € when considering only the subset of patients reporting work absence (13 of 16). Since there was only one case of family member absenteeism, related to an 82-year-old female patient, it was not included as part of the general analysis. This case would have accounted for 3 days of work absence and a total cost of 291.05 €.
Total Cost
Overall, the hospitalized hypoglycemic episode cost averaged 2042.52 € (range 194.76–16,762.87 €) from the NHS perspective, which corresponds to the total direct costs. Regarding the distribution by categories, time spent by healthcare professionals (both physicians and nurses) was the main driver representing 46.1% of the total cost per episode. The standardized occupancy cost accounted for 37.8%; laboratory tests and other examinations represented 13.9%; and drugs represented 2.2% of the total cost. The breakdown of the mean cost per resource type component and the mean cost per episode are presented in Table 3 and Fig. 1, respectively. Overall mean cost per episode is displayed at Fig. 2.
Costs per Gender and Age Group
The average costs were lower for patients aged at least 65 years old (1937.54 €, [194.76–16,762.87 €]) vs. 2277.13 €, [278.07–9234.44 €] for those aged less than 65 years old, and higher for male patients (2260.82 €) than female patients (1827.07 €).
Costs per DM Type and AHA Therapy Group
Patients with DM2 showed a higher average cost per episode (2051.29 €) in comparison with patients with DM1 (1840.90 €), but lower than other diabetes types (2426.27 €). Insulin-based therapy was the AHA therapy class with the highest average total cost (2267.76 € per episode), having an additional cost of 716.30 € (+ 46.2%) when compared to the least costly, the secretagogue-based regimen (1551.47 €). On the other hand, the mean cost attributed to patients receiving insulin-based therapy is very close to the mean cost estimated for the non-secretagogue group (2191.33 €) and combined therapy group (2246.65 €). The breakdown of cost per resource type is presented per DM type and per therapy regimen in Tables 3 and 4, respectively.
Impact of Complications of Hypoglycemia Event on Costs
The average costs per patient with a previous hypoglycemic episode in the previous 12 months (n = 58) and in the last 30 days (n = 38) were 1576.82 € and 1495.47 €, respectively. These costs are approximately 25% lower than the overall average (2042.52 €). The average costs increased to 2191.67 € in patients with repeated hypoglycemic events during hospitalization, to 2109.26 € in the group that recovered with complications, and up to 5253.38 € in patients whose discharge destination was registered as death.
Discussion
Hypoglycemia episodes are still a relevant concern when managing patients with DM in terms of clinical, humanistic, and economic aspects. The HIPOS-WARD study demonstrates the economic impact of hospitalizations due to hypoglycemia among people with DM in Portugal. From the NHS perspective, the average cost of a hospitalization due to hypoglycemia episode was estimated as 2042.52 €, regardless the DM type or ongoing therapy. The main cost driver was the time spent by healthcare professionals (both physicians and nurses), representing about 46.1% of the total cost per episode. Although it was not the most costly subgroup, the greater percentage of older patients (at least 65 years of age, 75.5%) and its extensive variability of cost may have been influenced by the overall average result. This could be also a confounding factor in the gender-specific analysis, since 84% of the female group were at least 65 years old. Thus, the median of costs is a more reliable parameter for an age-stratified analysis, being closer between both age groups (1391.60 € for patients less than 65 years old vs. 1469.73 € for those at least 65 years old).
Reviriego et al. [29] described a similar study, based on a retrospective review of patient charts from 100 patients with DM1 treated with insulin-based therapy. In that study, data were collected for patient characterization, resource usage, and correlated specific costs incurred by three Spanish hospitals. The average hospitalization cost was estimated as 183 € (223.31 €, inflated to 2018), including the preliminary ER visit and all inpatient treatments. Although hospitalizations were the main driver cost, accounting for 50% of the total cost of treating a hypoglycemic event, the results should be carefully interpreted as only 7% of cases required hospitalization. A Japanese study performed by Ikeda et al. [30] had estimated a mean hospitalization cost of 385,149 JPY (as proxy, 3176.35 € in 2018) for DM2 inpatients whose main cause of hospitalization was severe hypoglycemia using the receipt costs of each resource from public insurance databases, rather than DRG code costs (as performed in this study). This corresponded to 74.2% of the total cost, which is even higher than presented by Reviriego et al. [29].
In the USA, Liu et al. [31, 32] followed a microcosting approach, but based on resource consumption and associated payment costs from the private health insurance Truven MarketScan database, which covers approximately 33 million commercially insured population. Data from 2010 to 2015 were used to estimate a hypoglycemia-related hospitalization cost of 3551 USD (as proxy, 3273.70 € in 2018) for inpatients with DM1 using basal-bolus insulin regimen; 5802 USD for inpatients with DM2 using basal-bolus insulin and 6896 USD for inpatients with DM2 using basal insulin (equivalent to 5348.92 € and 6357.49 € in 2018, respectively). Patient enrollment was based on age (at least 18 years old), DM diagnosis code (ICD-9), insulin regime registries, and time since plan acquisition. Several clinical characteristics (e.g., HbA1c, body mass index, renal function, comorbid conditions, etc.) were not assessed or described, which may have resulted in selection bias. In 2011, Quilliam et al. [33] conducted a similar study based on the Medstat MarketScan database, which compiles data on 69 million Americans. All payments for patients with DM2 made to the provider, including copayments, coinsurance, and deductibles, were captured for cost estimations.
For inpatients, mean cost of hypoglycemia admissions was 17,564.25 USD (17,825.48 € in 2018), including the cost of the ER visit that led to the hospitalization. The clear difference between both studies could be due to the population selected: the whole DM2 population covered by Liu et al. was under insulin-based therapy and most of them were aged at least 65 years old with at least one comorbidity, whereas of those in Quilliam’s study, only 6% received insulin and 0.1% patients with DM2 were at least 65 years old. Patients’ comorbidities were not described, which may have a significant clinical and economic impact. Additionally, the exact structure of costs compiled was not described in either study nor was the year of USD quoted in Liu et al.’s study, making it challenging to confirm the correlation. Alternative study designs, such as literature reviews [34, 35], physicians’ surveys [36] or patients’ surveys [37], or those based on general DM hospitalization DRG code costs [34, 35, 38, 39], have limited comparability with the HIPOS-WARD study, as a cross-sectional microcosting approach.
Several studies are exclusively population-based (DM type, therapy specific, etc.) and focused on specific spheres of care (self-care for non-severe episodes or hospital care for severe episodes), making the analysis less generalizable. Additionally, most studies presented the cost per year, not per episode, and, in some of them [30,31,32], the year of quotation was not presented. Therefore, to project the cost to euros in 2018, the last year of data collection described was assumed as the currency year. Finally, hospitalization costs usually appear as a fraction of the total cost, mostly based on diabetes with complications rather than specific for hypoglycemic events, which compromised comparison with our analysis. Despite all the differences in health services and the costing methodologies used, overall conclusions are qualitatively similar, confirming the significant clinical and economic burden of the drug-related hypoglycemia events to the healthcare system. In the HIPOS-ER study [18], the mean hospitalization cost was estimated as 2880 € (2981.22 € in 2018) for patients whose hypoglycemia episode led to hospitalization after ER attendance (44.1%).
However, there are also methodological differences compared to HIPOS-WARD. First, in the ER analysis, only patients with DM2 over 40 years old (average 76 years) were included and, since the ER cost was the primary objective, hospitalization was only part of the total cost. Moreover, the ER initial visit cost was exceptionally included in the HIPOS-ER estimate and hospitalization cost was limited to the daily costs from the Hospitals Accountability Report per ward unit, which is the source used only for the bed occupancy in the HIPOS-WARD microcosting analysis, thereby hindering a direct correlation. Thus, when limiting HIPOS-WARD data to the disease type and age group as in HIPOS-ER, an average total cost of 2224.77 € is achieved, which was close but still probably affected by differences in the methodology (microcosting vs. disease-unspecific database).
On the other hand, the official Portuguese datasource for hospital reimbursement (Portaria 254/2018) [25] corroborates the costs estimated in the HIPOS-WARD study. This source provides the mean hospitalization cost and mean duration of diabetes DRG codes per grade [1,2,3,4], regardless of DM type, therapy, or hospitalization cause. The mean duration of 9.2 days in the primary ward and the mean direct cost of 2042.52 €, from our microcosting approach, could be directly compared to the diabetes DGR tariff for grade 3 episode, for which the mean duration (10.88 days) and the average cost (2377.77 €) are both slightly higher. As expected, the mean hypoglycemic hospitalization cost obtained in HIPOS-WARD is much higher than the International Diabetes Federation (IDF) estimated mean diabetes-related expenditure per person in Portugal (i.e., approximately 1694 €, when inflected to 2018) [40] and to the public expenditure on healthcare per capita in Portugal (i.e., approximately €1740 by World Health Organization (WHO)’s estimate adjusted for purchasing power parity, 2014).
Absenteeism-related costs due to hospitalization summed only 140.44 € on average, which is not surprising given that the mean age of HIPOS-WARD patients (72 years) was much higher than the current retirement age in Portugal (66 years). Although there were 45 (26%) potential economically active patients (aged between 18 and 65 years), only 16 (9.1%) reported current employment. Of these, 81.2% had work absence periods. Moreover, the only response regarding the caregiver absenteeism is likely to be underestimated considering the hospitalization setting and that approximately 75% patients were elderly (at least 65 years old). Therefore, as a result of the data fragility and uncertainties related to the indirect costs, iit was noted as a limitation and it was dealt with separately in the present analysis. Nevertheless, an increase in the economic and clinical burden of the disease it is expected when extrapolating to the general economically active population with DM and caregivers.
Regarding AHA therapy groups, the insulin-based group has the highest mean expenditure, while the secretagogue-based group has the lowest, mainly due the reduced cost spent on the bed occupancy and lowest physician time.
No correlation with the patient’s profile (e.g., DM type, age, previous and multiple hypoglycemic events) could be attributed to a longer hospital stay and costs, although male patients with DM1 receiving insulin-based therapy presented the longest stay. Additionally, patients’ characterization did not statistically differ between AHA therapy groups, but again the insulin-based group presented the highest frequency of chronic DM complications, lowest glycemia at entry, and higher median values of HbA1c at baseline. An indirect effect of the overall patient condition is expected on hospitalization prognosis; however, it is difficult to be precise considering so many confounding factors. Thus, it reinforces the importance to periodically review the therapeutic scheme and to consider other drugs with great potential to achieve glucose level target but with reduced risk of hypoglycemia, allowing one to minimize costs attributed to this adverse event. Performing an individualized therapy approach and keeping the patient well informed about the required self-care may avoid recurrent hypoglycemic events.
Finally, the present study, together with the HIPOS-PHARMA and HIPO-ER studies, reflects the real-world setting related to hospitalization due to hypoglycemia episodes in patients with DM in Portugal, improving the general knowledge on its economic and clinical burden and supporting the decision-makers’ assessment regarding new therapies when reviewing the disease protocols of conduct. The main strength of this economic analysis was the microcosting methodological rigor, corroborated by increased external validity. Furthermore, as the primary objective of the study was the estimation of DM type and AHA therapy prevalence, inclusion criteria were kept minimal and, to minimize selection bias, patients were enrolled in a consecutive manner. Although data were from official Portuguese databases, assumptions and extrapolations were necessary to adjust the format of different unitary costs from the different sources; this is a limitation. Additionally, the indirect costs might have been underestimated, mainly regarding caregiver’s absenteeism, but also presenteeism, early retirement due to incapacity, and premature death. Out-of-pocket expenditures with private assistance, pharmacy, and transportation were likewise not included in the study protocol in order to not increase the complexity with extensive patient interviews and uncertainty.
Overall, the findings presented herein reinforce the importance of an individualized therapy goal, continuous development of medical education programs, and orientations for patients’ self-management. Nevertheless, in complement to the HIPOS project, this study particularly aimed to measure the costs of hypoglycemic events leading to hospitalization, therefore further investigation is needed to cover other settings and the limitations assessed, such as homecare management, the period beyond hospitalization discharge, rest-of-life consequences, and the correlated impact on quality of life.
Conclusion
This microcosting study provides detailed, real-world, observational data, contributing to the characterization of the burden of hypoglycemia-related hospitalizations in Portugal and the need for close assistance with DM medication treatment. Preventing hypoglycemic episodes that would evolve to hospitalizations could reduce both the clinical and economic burden to the NHS.
References
World Health Organization. World health statistics overview 2019: monitoring health for the SDGs, sustainable development goals. World Health Organization; 2019. https://www.who.int/gho/publications/world_health_statistics/2019/en/.
WHO. Diabetes. 2018. https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed Mar 16 2020.
International Diabetes Federation. IDF Diabetes Atlas. 8th ed. 2017. https://www.diabetesatlas.org/.
Roglic G. WHO global report on diabetes: a summary. Int J Noncommun Dis. 2016;1:3–8.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35:1364–79.
International Diabetes Federation. Global guideline for type 2 diabetes. Brussels: International Diabetes Federation; 2005. https://www.idf.org/e-library/guidelines/79-global-guideline-for-type-2-diabetes.
Direção Geral de Saúde. Prescrição e determinação da hemoglobina glicada A1c. 2011. Report No. 033/2011. https://www.dgs.pt/directrizes-da-dgs/normas-e-circulares-normativas/norma-n-0332011-de-30092011-atualizada-a-06122012-jpg.aspx.
Morales J, Schneider D. Hypoglycemia. Am J Med. 2014;127:S17–24.
Karter AJ, Warton EM, Lipska KJ, et al. Development and validation of a tool to identify patients with type 2 diabetes at high risk of hypoglycemia-related emergency department or hospital use. JAMA Intern Med. 2017;177:1461–70.
Cryer PE, Axelrod L, Grossman AB, et al. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2009;94:709–28.
Ha WC, Oh SJ, Kim JH, et al. Severe hypoglycemia is a serious complication and becoming an economic burden in diabetes. Diabetes Metab J. 2012;36:280.
Brackenridge A. Emergency management of diabetes and hypoglycaemia. Emerg Med J. 2006;23:183–5.
Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174:1116–24.
Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–16.
Sociedade Portuguesa de Diabetologia. Diabetes: factos e números-o ano de 2015. 2016, p. 68. https://www.spd.pt/images/bolsas/dfn2015.pdf.
Torre C, Guerreiro JP, Romano S, et al. Real-world prevalence of mild to moderate hypoglycemic episodes in type 2 diabetes in Portugal: results from the HIPOS-PHARMA study. Primary Care Diabetes. 2018;12:537–46.
Conceição J, Dores J, Araújo F, et al. Severe hypoglycaemia among patients with type 2 diabetes requiring emergency hospital admission: the Hypoglycaemia In Portugal Observational Stud-Emergency Room (HIPOS-ER ). Diabetes Obes Metab. 2018;20:50–9.
Laires PA, Conceição J, Araújo F, et al. The cost of managing severe hypoglycemic episodes in type 2 diabetic patients. Expert Rev Pharmacoecon Outcomes Res. 2016;16:315–25.
American Diabetes Association Workgroup on Hypoglycemia. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association workgroup on hypoglycemia. Diabetes Care. 2005;28:1245–9.
Direção Geral de Saúde. Abordagem terapêutica farmacológica na diabetes mellitus tipo 2 no adulto. 2011. Report No.: 052/2011. https://nocs.pt/wp-content/uploads/2015/11/Abordagem-Terap%C3%AAutica-Farmacol%C3%B3gica-na-Diabetes-Mellitus-Tipo-2-no-Adulto.pdf. Accessed 28 Nov 2018.
Sindicato Independentes dos Médicos. Tabelas salariais 2018. 2018. https://www.simedicos.pt/pt/gabinete-juridico/tabelas-salariais/. Accessed 28 Nov 2018.
Sindicato dos Enfermeiros Portugueses. Tabela salarial de enfermagem. 2017. https://www.sep.org.pt/files/uploads/2017/06/sep_23062017_TSEnfermagem_2017_35horas_a_partir_1abril.pdf. Accessed 28 Nov 2018.
BaseGov - Contratos Públicos Online. https://www.base.gov.pt. Accessed Nov 28 2018.
INFARMED. InfoMed - Base de dados de medicamentos. https://app7.infarmed.pt/infomed/inicio.php. Accessed Nov 28 2018.
Diário da República. Portaria no 254/2018. Sect. 1st serie, 254 Sep 7, 2018 p. 210.
Administração Central do Sistema de Saúde. Base de Dados de Elementos Analíticos (BDEA). https://www.acss.min-saude.pt/bdea/. Accessed Nov 28 2018.
Instituto Nacional de Estatística. Tabela de ganho mensal médio. 2020. https://www.ine.pt/xportal/xmain?xpid=INE&xpgid=ine_indicadores&indOcorrCod=0006914&contexto=bd&selTab=tab2. Accessed Nov 28 2018.
Autoridade Tributária e Aduaneira. Tabelas de retenção do IRS. 2018. https://info.portaldasfinancas.gov.pt/pt/apoio_contribuinte/tabela_ret_doclib. Accessed Nov 28 2018
Reviriego J, Gomis R, Marañés JP, Ricart W, Hudson P, Sacristán JA. Cost of severe hypoglycaemia in patients with type 1 diabetes in Spain and the cost-effectiveness of insulin lispro compared with regular human insulin in preventing severe hypoglycaemia: SH in patients with type 1 diabetes in Spain. Int J Clin Pract. 2008;62:1026–32.
Ikeda Y, Kubo T, Oda E, Abe M, Tokita S. Retrospective analysis of medical costs and resource utilization for severe hypoglycemic events in patients with type 2 diabetes in Japan. J Diabetes Investig. 2019;10:857–65.
Liu J, Wang R, Ganz ML, Paprocki Y, Schneider D, Weatherall J. The burden of severe hypoglycemia in type 1 diabetes. Curr Med Res Opin. 2018;34:171–7.
Liu J, Wang R, Ganz ML, Paprocki Y, Schneider D, Weatherall J. The burden of severe hypoglycemia in type 2 diabetes. Curr Med Res Opin. 2018;34:179–86.
Quilliam BJ, Simeone JC, Ozbay AB, Kogut SJ. The incidence and costs of hypoglycemia in type 2 diabetes. Am J Manag Care. 2011;17:8.
Parekh WA, Ashley D, Chubb B, Gillies H, Evans M. Approach to assessing the economic impact of insulin-related hypoglycaemia using the novel local impact of hypoglycaemia tool. Diabet Med. 2015;32:1156–66.
Foos V, Varol N, Curtis BH, et al. Economic impact of severe and non-severe hypoglycemia in patients with type 1 and type 2 diabetes in the United States. J Med Econ. 2015;18:420–32.
Kim G, Lee Y, Han MH, et al. Economic burden of hypoglycemia in patients with type 2 diabetes mellitus from Korea. PLoS One. 2016;11:0151282.
Hammer M, Lammert M, Mejías SM, Kern W, Frier BM. Costs of managing severe hypoglycaemia in three European countries. J Med Econ. 2009;12:281–90.
Leese GP, Wang J, Broomhall J, et al. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Diabetes Care. 2003;26:1176–80.
Holbrook T, Tang Y, Das R, et al. Direct medical costs of severe hypoglycaemic events in patients with type 2 diabetes in England: a retrospective database study. Int J Clin Pract. 2017;71:e12958.
International Diabetes Federation. IDF Diabetes Atlas. 6th ed. 2013. https://www.idf.org/e-library/epidemiology-research/diabetes-atlas/19-atlas-6th-edition.html. Accessed 28 Nov 2018.
Acknowledgements
The authors would like to acknowledge the contribution of all hospital department staff of the hospitals mentioned above.
Funding
Sponsorship for this study and Rapid Service Fee were funded by MSD Portugal, although the publication of study results was not contingent on the sponsor’s approval or censorship.
Medical Writing, Editorial and Other Assistance
Economic analysis and medical writing assistance were provided by Victoria Genovez Soares, Market Access Associate II; editorial assistance was provided by Catarina Alves, Research Scientist II; and statistical support was provided by Vera Vicente, Senior Statistician, all of them employees at CTI Clinical Trial and Consulting Services. All assistance was funded by MSD Portugal.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
FA, JD, LS, JC, PAL, SA made substantial contributions to the study conception, design, and planning; EP, MR, AC, EN, AB, VP, CM, ASL contributed to data acquisition, JPF to the analysis and FA, JD, LS, EP, MR, AC, EN, AB, VP, CM, ASL, JC, JPR, SA interpretation of the data. All authors have revised the publication critically for important intellectual content and approved the manuscript for publication.
List of Investigators
The full list of study investigators can be found in the Supplementary Material.
Disclosures
Sílvia Alão is an employee of MSD Portugal. Lèlita Santos has served as a paid lecturer and/or a consultant to Merck Sharp & Dohme, Lda, Portugal and AstraZeneca Portugal. Jorge Dores has served as a paid lecturer and/or a consultant to Merck Sharp & Dohme, Lda, Portugal, Abbott Diagnostics, Portugal, AstraZeneca Portugal, Boehringer Ingelheim, Portugal, Lilly Produtos Farmacêuticos, Portugal, Novartis Farma, Novo Nordisk Portugal and Sanofi, Portugal. Francisco Araújo has served as a paid lecturer and/or research grant to Merck Sharp & Dohme, Lda, Portugal, AstraZeneca Portugal, Medinfar Portugal. Estevão Pape, Mónica Reis, Árcia Chipepo, Edite Nascimento, Ana Baptista, Vanessa Pires, Carlos Marques, Adriana De Sousa Lages have nothing to disclose. João Conceição is an employee of MSD International GmbH (Singapore Branch). João Pelicano-Romano is an employee of MSD Portugal. João Ferreira is an employee of MSD Portugal. Pedro Almeida Laires was an employee of MSD Portugal at the time the study was conducted.
Compliance with Ethics Guidelines
The study was approved by the ethics committees of each participating center (Supplementary Material) and by the National Committee for Data Protection. All procedures were conducted in accordance with the Declaration of Helsinki and the Good Pharmacoepidemiology. All participants of the study or their legally acceptable representative signed an informed consent form, which adhered to IRB/ERC requirements, applicable laws and regulations, and sponsor requirements.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author [SA] on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12490214.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ferreira, J.P., Araújo, F., Dores, J. et al. Hospitalization Costs Due to Hypoglycemia in Patients with Diabetes: A Microcosting Approach. Diabetes Ther 11, 2237–2255 (2020). https://doi.org/10.1007/s13300-020-00868-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-020-00868-0