Abstract
Introduction
The aim of the study was to determine the level of metabolic control in type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) patients in the Czech and Slovak Republics.
Methods
A non-interventional prospective (observational) study was conducted from January 2015 until April 2016 in routine clinical practice settings at 141 centers in the Czech and Slovak Republics. Data were analyzed from a total of 425 patients with T1DM and 1034 patients with T2DM, proportionally corresponding to the number of patients in both countries. The primary objective of the study was to determine the percentage of patients with HbA1c < 7% (53 mmol/mol).
Results
Patients with T1DM: In this group of patients (55.8% males, mean age 45.9 ± 14.83 years, BMI 25.8 ± 4.21 kg/m², diabetes duration 12.1 ± 9.44 years), 29.9% reached HbA1c levels < 53 mmol/mol. Patients with T2DM: In this group of patients (50.3% male, mean age 63.9 ± 9.65 years, BMI 31.0 ± 5.19 kg/m², diabetes duration 12.4 ± 7.47 years, duration of insulin therapy 5.8 ± 4.71 years), 33.4% reached HbA1c levels < 53 mmol/mol.
Conclusion
The overall percentage of patients with HbA1c < 53 mmol/mol in the T1DM group was 29.9% and in the T2DM group was 33.4%. Despite an increasing number of treatment options, most patients still fail to reach the recommended HbA1c targets.
Funding
Sanofi, Czech Republic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The results of the DCCT and UK Prospective Study studies have shown that achieving the recommended glycemic targets reduces the morbidity in patients with diabetes mellitus (DM) [1,2,3]. Uncontrolled diabetes mellitus is also associated with worsening quality of life [4,5,6].
The diabetic medical standards defined by the American Diabetes Federation recommend a reduction in HbA1c < 7% (< 53 mmol/mol), which in most patients will lead to a decrease in the incidence of microvascular complications. In some patients, especially those with short-term diabetes, long life expectancy, and no cardiovascular disease, more stringent treatment goals, such as < 6.5%, can be proposed if these can be achieved without hypoglycemia or other adverse treatment consequences. Conversely, higher than recommended HbA1c values, e.g., < 8.0% or even slightly higher, may be tolerated on an individual basis in patients with a history of severe hypoglycemia, advanced micro- and macrovascular complications, low expected survival periods, or where better results cannot be achieved despite maximum care including extensive education, sufficient self-monitoring of glycemia, and use of combined treatment with available preparations, including insulin [7]. These recommendations are also supported in the case of type 2 diabetes mellitus by the consensual views of the European Association for the Study of Diabetes and the American Diabetes Association [8].
However, despite the continuously improving treatment options, many patients still do not achieve the recommended treatment goals. The results of the recently published multinational cross-sectional study, carried out in seven countries of the European Union and Turkey between 2009 and 2010 in patients with type 2 diabetes mellitus (T2DM), showed the mean (SD) HbA1c of the total patient population was 6.9% (± 1.1%) and 37.4% of patients had HbA1c ≥ 7%. The proportion of patients with HbA1c ≥ 7% ranged from 25.9% in The Netherlands to 36.3% in Germany to 52.0% in Turkey [9].
The only published cross-sectional multinational study published to date from the Central and Eastern European region, carried out between 2006 and 2007, showed that only a minority of diabetic patients [13.1% for type 1 diabetes (T1DM) and 21.4% for type 2 diabetes mellitus] had reached the then defined treatment goals (HbA1c < 6.5%), with an average attained HbA1c value of 8.2% for T1DM and 7.7% for T2DM [10]. However, neither of the above-mentioned studies investigated the extent to which treatment targets were achieved specifically in patients with T2DM treated with insulin.
The results of the NHANES analysis conducted on data from 2005–2012 in the USA showed that an HbA1c value < 7% was reached by 31.4% of patients and < 8% value by 61.7% of patients treated with insulin, however, regardless of the type of diabetes. Therefore, this study does not indicate the extent to which treatment targets have been achieved specifically in patients with T2DM treated with insulin [11].
The aim of the DIAINFORM study was thus to verify glycemic control measured by HbA1c values separately in patients with T1DM and in patients with T2DM treated with at least one daily insulin injection. Concurrently, it aimed to describe the factors that could influence this control and to determine the quality of life of the patients with the intention to provide guidance on potential future policies to improve the care of these patients. The data analysis presented here describes the current rate of achieving the HbA1c target values and evaluates the progress of HbA1c values over the previous 3 years.
Methods
Study Design
Detailed information about the DIAINFORM study design has been previously reported [12]. The study aims to evaluate glycemic control as measured by HbA1c in T1DM and T2DM patients treated with at least one insulin injection daily and to describe factors affecting the achievement of this control. The study enrolled patients from 141 study centers in the Czech Republic and Slovak Republic.
Study Population
The study was carried out between 2 January 2015 and 14 April 2016. The inclusion criteria were T1DM or T2DM, patients aged > 18 years, treatment with at least one insulin injection daily for > 1 year (to allow enough time for insulin titration), willingness to fill in the study questionnaires, and a signed patient informed consent form. The exclusion criteria were insulin therapy for < 12 months, current insulin pump therapy or the use of this treatment in the last 12 months, unavailability of the Hb1Ac test results in the last 3 months before the V1, pregnancy, inability to be present at the follow-up visit, inability to complete the study questionnaires, and participation in another clinical study within the last 3 months.
Compliance with Ethics Guidelines
All study procedures were carried out in accordance with the International Conference on Harmonisation/Good Clinical Practice, and the final study protocol was approved by the Ethics Committee of the National Institute of Endocrinology and Diabetology in Lubochna, Slovak Republic (approval date 4 February 2015). All participants provided written informed consent.
Insulins Involved in the Study
None of the insulins available in the Czech Republic during the study period were excluded. The basal insulins included an intermediate-acting insulin (neutral protamine Hagedorn, NPH) and long-acting insulin analogs (glargine 100 U/ml, detemir, and in the Slovak Republic also deglutec). The short-acting insulin was recombinant human insulin, and fast-acting insulins included insulin analogs (aspart, glulisin, and lispro). Premixed insulin preparations were the proportionate mixtures of a short- or fast-acting insulin and intermediate-acting insulins (in proportions of 25/75, 30/70 and 50/50) produced commercially by Eli Lilly, Novo Nordisk, or Sanofi.
Outcomes
The primary objective was to determine the prevalence of diabetes patients achieving HbA1c < 7.0% (53 mmol/mol) as obtained in the enrollment visit (V1). The secondary objective was to determine HbA1c values during the period of 3 years prior to V1.
Data Collection
Patients were enrolled into the study consecutively; at the end of the study, the recruitment of patients with type 2 diabetes mellitus was controlled so that the proportion of patients between individual regimens corresponded to their estimated population number. The maximum number of patients per center was 14. HbA1c values were listed by a physician from medical records. The current value of HbA1c at V1 was the last value obtained over the previous 3 months.
Statistical Methods
The primary objective of the study was to separately determine the prevalence of insulin-treated diabetic patients with HbA1c levels < 7.0% (53 mmol/mol) in patients with type 1 and type 2 diabetes. The prevalence was calculated as a percentage of the patients with HbA1c levels < 7.0% (obtained at V1) accompanied by a two-sided 95% Wilson score confidence interval. HbA1c values during the period of the previous 3 years and current HbA1c values at visit 1 were analyzed via descriptive statistics for numerical variables (mean, standard deviation, median, upper and lower quartiles, minimum, maximum) and accompanied by a profile figure (mean profile for each group).
Study Interventions
The study was non-interventional.
Results
Study Sample
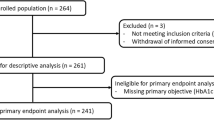
A total of 1508 patients were enrolled in the study with the final eligible population consisting of 1459 patients, of which 425 had T1DM and 1034 T2DM. Among patients with T2DM, 242 (23.4%) were treated with the regimens of two doses of premixed insulin, 320 (31.0%) with basal insulin and oral antidiabetic drugs (OADs), and 448 (43.3%) with multiple daily insulin doses (MDI). The number of patients treated with a regimen other than the above-mentioned ones was low (n = 24), so we did not include this group in the evaluation. An overview of patient, disease, and treatment characteristics for the total sample is shown in Table 1.
Level of Glycemic Control
The proportion of patients with type 1 diabetes mellitus with HbA1c values < 7% (53 mmol/mol) was 29.9% (95% CI 25.73–34.40). The proportions of patients divided according to the HbA1c values for the whole set and separately for the Czech and Slovak Republics are listed in Fig. 1. The average HbA1c value (SD) in the whole set was 7.9 (1.9) % [62.3 (15.14) mmol/mol]; the average fasting plasma glucose value (SD) in type 1 diabetes patients was 8.1 ± 3.3 mmol/l and in type 2 diabetes was 7.8 ± 2.6 mmol/l.
The proportion of patients with type 2 diabetes mellitus with HbA1c values < 7% (53 mmol/mol) was 33.4% (95% CI 30.56–36.30). The proportions of patients divided according to the HbA1c values for the whole set and separately for the Czech Republic and the Slovak Republic are listed in Fig. 2. The average HbA1c value (SD) in the whole set was 7.7 (1.8) % [60.2 (14.05) mmol/mol].
The proportion of patients with type 2 diabetes mellitus with HbA1c values < 7% (53 mmol/mol) treated with two doses of premixed insulin was 31.0% (95% CI 25.50–37.08), treated with basal insulin and OADs was 35.9% (30.88–41.33), and treated with MDI was 31.9% (27.77–36.37).
Mean Insulin Dose
The mean insulin dose in T1DM patients was 0.59 (0.22) IU/kg/day and in T2DM patients was 0.50 (0.28) IU/kg/day. The mean insulin dose in the group of patients treated with basal insulin and OADs was 0.28 (0.17), in those treated with premixed insulin 0.50 (0.21) and in those treated with MDI 0.65 (0.27) IU/kg/day.
The Development of HbA1c Values over the 3 Years Prior the Study
In T1DM patients, the mean HbA1c value (SD) in the 33–36-month period prior to the study visit was 8.1 (2.1) % [64.8 (17.27) mmol/mol]. The difference between this value and the average value during a study visit was 0.2% (2.4 mmol/mol).
In T2DM patients, the mean HbA1c value (SD) in the 33–36-month period prior to the study visit was 7.9 (2.1) % [63.0 (14.52) mmol/mol]. The difference between this value and the average value during a study visit was 0.2% (2.8 mmol/mol). Average HbA1c values in each 3-month period during the 3 years prior to the study visit in patients with both types of diabetes are shown in Fig. 3.
Discussion
The DIAINFORM study provides important data showing the level of metabolic control in patients with T1DM and T2DM treated with insulin in the Czech and Slovak Republics. The mean HbA1c value in patients with T1DM in the DEPAC study [7], which was carried out approximately 10 years earlier in the EU accession countries including the Czech Republic and Slovak Republics, was 8.2% (66 mmol/mol), the proportion of patients with HbA1c < 7% (53 mmmol/mol) was 23.9%, and the proportion of patients with HbA1c ≥ 8% (64 mmol/mol) was 48.2%. These data suggest an improvement in the level of metabolic control up to the present time. However, the comparison is distorted by the fact that only values from the eight countries together are available from the DEPAC study. It can be speculated that this improvement in metabolic control could be caused by higher levels of education, more frequent self-monitoring of glycemia due to the decrease in test strip prices resulting in their wider availability, and perhaps also the new types of insulin, especially long-acting insulin analogs, which were less available at the time of the above-mentioned DEPAC study. However, more research is needed before any definitive statement can be made.
The comparison of our results in T2DM patients is even more complicated as similar studies are not available. In the DEPAC study, insulin-treated patients were not analyzed individually, and the mean HbA1c value in all patients without treatment difference was 7.7% (60.7 mmol/mol) and therefore similar to that in our study. The proportion of patients with HbA1c < 7% (53 mmmol/mol) was 36.7%, i.e., only slightly higher than our data results, and the proportion of patients with HbA1c ≥ 8% (64 mmol/mol) was 37.6%, i.e., higher than in our study. Comparing such differing sets is difficult, especially if we know that the proportion of insulin-treated patients was only 14.3% in the DEPAC study. However, given that in most patients who have been treated with insulin, which is the last-choice drug, the achievement of HbA1c target values is usually the most complicated, and it can be speculated that even here metabolic control is likely to have improved.
Similarly, we could interpret one of the results of the PANORAMA study [6] in which a group of patients with T2DM treated with insulin and/or GLP-1 analog was individually analyzed; the proportion of patients with HbA1c < 7% (53 mmmol/mol) was 36.1%, similar to what our study has shown.
Analysis of the NHANES registry data for the 2005–2012 period showed that the proportion of patients treated only with insulin with HbA1c < 7% (53 mmmol/mol) was 31.4%, i.e., similar or just slightly worse than our results. However, the analysis in this study was not carried out individually for patients with T1DM and T2DM, so this comparison also has its limitations. The proportions of patients with HbA1c < 7% (53 mmmol/mol) in the subgroups treated with MDI, two doses of mixed insulin, and the combination of basal insulin and OADs did not differ significantly. One of the reasons why, unlike in clinical studies, more patients did not reach the HbA1c recommended values could be that the average therapeutic dose of insulin was lower in our study than in a number of other studies [13, 14, 15]. This difference reflects the genuine possibilities of real clinical practice as opposed to clinical studies, where the usual patient care is extended by a precise protocol, extended education, sufficient amount of test strips, telephone consultations, etc. Of course, the fear of hypoglycemia may also play a role in increasing the dose, which is true for both the patient and the physician [16].
The analysis of the development of HbA1c values over the last 3 years produced an interesting result, showing that there has been no clinically significant improvement of metabolic control in either T1DM or T2DM during this time. It seems to be clear, therefore, that there is a high degree of clinical inertia in both patient groups, probably due to common factors on both the physician’s and patient’s side, as well as in the medical system [17].
The rate of achievement of target values in patients with T1DM and T2DM treated with insulin is unsatisfactory in the Czech and Slovak Republics. However, based on an indirect comparison with several similar studies, it does not seem to be worse than in other countries in which such types of data are available.
What can we do for those who do not achieve the target values? We should definitely try harder to uncover the real barriers to controlling their diabetes and offer them related education or treatment. These may range from simple insulin injection technique mistakes to a lack of knowledge regarding insulin titration and hypoglycemia prevention to complicated psychologic issues. The newest therapeutical drugs and instruments designed for the treatment of diabetes are available in both republics, and these should be used when appropriate.
There are some limitations to consider in this study. First, the number of patients is lower than usually presented in “register studies,” but it was carefully calculated prior to beginning our study; the study protocol was developed through a peer-review process [8]. Second, illiterate patients or those otherwise unable or not willing to complete a questionnaire were excluded, which could cause a population bias. Nevertheless, we believe that our study provides relevant and valuable results.
Conclusion
The DIAINFORM study provided real-world data showing that the overall percentage of patients with HbA1c < 53 mmol/mol in the T1DM group was 29.9% and in the T2DM group was 33.4%. Despite an increasing number of treatment options, most patients still fail to reach the recommended HbA1c targets.
References
DCCT Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
Nathan DM. DCCT/EDIC Research Group. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care. 2014;37(1):9–16. https://doi.org/10.2337/dc13-2112.
Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes UK prospective diabetes study (UKPDS 35): prospective observational study. Br Med J. 2000;321:405–12.
Vanstone M, Rewegan A, Brundisini F, Dejean D, Giacomini M. Patient perspectives on quality of life with uncontrolled type 1 diabetes mellitus: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2015;15(17):1–29.
da Mata AR, Álvares J, Diniz LM, et al. Quality of life of patients with Diabetes Mellitus Types 1 and 2 from a referal health centre in Minas Gerais, Brazil. Expert Rev Clin Pharmacol. 2016;9(5):739–46. https://doi.org/10.1586/17512433.2016.1152180.
Kuznetsov L, Griffin SJ, Davies MJ. Diabetes-specific quality of life but not health status is independently associated with glycaemic control among patients with type 2 diabetes: a cross-sectional analysis of the addition-Europe trial cohort. Diabetes Res Clin Pract. 2014;104:281–7.
American Diabetes Association. Glycemic targets. Sec. 6. In standards of medical care in diabetes 2017. Diabetes Care 2017;40(Suppl. 1):S48–56.
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care. 2015;38(1):140–9. https://doi.org/10.2337/dc14-2441.
Pablos-Velasco P, Parhofer KG, Bradley C, Eschwege E, Gonder-Frederick L, Maheux P, et al. Current level of glycaemic control and its associated factors in patients with type 2 diabetes across Europe: data from the PANORAMA study. Clin Endocrinol. 2014;80:47–56.
Andel M, Grzeszczak W, Michalek J, Medvescek M, Norkus A, Rasa I, et al. A multinational, multi-centre, observational, cross-sectional survey assessing diabetes secondary care in central and Eastern Europe (DEPAC survey). Diabet Med. 2008;25(10):1195–203. https://doi.org/10.1111/j.1464-5491.2008.02570.x.
Selvin E, Parrinello ChM, Daya N, Bergenstal RM. Trends in insulin use and diabetes control in the US: 1988–1994 and 1999–2012. Diabetes Care. 2016;39(3):e33–5. https://doi.org/10.2337/dc15-2229.
Brož J, Janíčková Žďárská D, Urbanová J, Brabec M, Křivská B, Doničová V, et al. An international, multicenter, observational survey to evaluate diabetes control in subjects using insulin for the treatment of type 1 and type 2 diabetes mellitus in the Czech Republic and Slovakia: study protocol for a cross-sectional survey. Open Access J Clin Trials. 2016. https://doi.org/10.2147/OAJCT.S103459.
Riddle MC, Bolli GB, Ziemen M, Muehlen-Bartmer I, Bizet F, Home PD. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37(10):2755–62. https://doi.org/10.2337/dc14-0991.
Rosenstock J, Hollander P, Bhargava A, Ilag LL, Pollom RK, Zielonka JS, et al. Similar efficacy and safety of LY2963016 insulin glargine and insulin glargine (Lantus®) in patients with type 2 diabetes who were insulin-naïve or previously treated with insulin glargine: a randomized, double-blind controlled trial (the ELEMENT 2 study). Diabetes Obes Metab. 2015;17(8):734–41. https://doi.org/10.1111/dom.12482.
Riebenfeld D, Spirk D, Mathis A, Villiger L, Gerber PA, Gasser UE, Lehmann R. Treatment intensification with insulin glargine in patients with inadequately controlled type 2 diabetes improves glycaemic control with a high treatment satisfaction and no weight gain. Swiss Med Wkly. 2015;145:w14114. https://doi.org/10.4414/smw.2015.14114 (eCollection 2015).
Reach G, Pechtner V, Gentilella R, Corcos A, Ceriello A. Clinical inertia and its impact on treatment intensification in people with type 2 diabetes mellitus. Diabetes Metab. 2017;43(6):501–11. https://doi.org/10.1016/j.diabet.2017.06.003
Fisher SJ, Huang X, Pawaskar M, et al. Hypoglycemia in type 2 diabetes: understanding patients’ and physicians’ knowledge and experience. Endocrine. 2018;60:435–44. https://doi.org/10.1007/s12020-018-1545-0.
Acknowledgements
We thank the study participants.
Funding
This study and associated article processing charges were funded by Sanofi, Czech Republic. The role of the sponsor was to appoint an independent research company and carry out the study (ADDS sro). All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Editorial Assistance
Special thanks go to Dion Pritchard for language editing.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Jan Brož initiated the study and contributed to the study design, data analysis and interpretation, as well as the drafting, review, and editing of the manuscript, and in doing so led all of the efforts. Denisa Janíčková Žďárská, Jana Urbanová, Marek Brabec, Viera Doničová and Emil Martinka contributed to the study design, data analysis and interpretation, as well as the drafting, review, and editing of the manuscript. Radka Štěpánová contributed to the data analysis, drafting of the manuscript, and the review and editing of the manuscript. Milan Kvapil is a guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
The results of this study were presented in abstract form at the Annual National Congress of the Czech Diabetes Society in Luhačovice, Czech Republic, from 4–7 April 2017.
Disclosures
Jan Brož has received payment for being an adviser to and a speaker for Sanofi-Aventis and Eli Lilly. He has also received payment for being the international coordinator of the study.
Denisa Janíčková Žďárská disclosed the receipt of financial support for the research, authorship, being a speaker, and being an educator for Sanofi-Aventis, AstraZeneca, Eli Lilly, Novo Nordisk, Merc Sharp and Dohme, and Johnson & Johnson.
Radka Štěpánová works as a statistician for CRO Aprova, which was contracted by Sanofi-Aventis for the statistical analysis of this study.
The authors Jana Urbanová, Marek Brabec, Viera Doničová, Emil Martinka, and Milan Kvapil report no other conflicts of interest in this work.
Compliance with Ethics Guidelines
All study procedures were carried out in accordance with the International Conference on Harmonisation/Good Clinical Practice and the final study protocol was approved by the Ethics Committee of the National Institute of Endocrinology and Diabetology in Lubochna, Slovak Republic (approval date 4 February 2015). All participants provided written informed consent.
Data Availability
The data sets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article, go to https://doi.org/10.6084/m9.figshare.6887195.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Brož, J., Janíčková Žďárská, D., Urbanová, J. et al. Current Level of Glycemic Control and Clinical Inertia in Subjects Using Insulin for the Treatment of Type 1 and Type 2 Diabetes in the Czech Republic and the Slovak Republic: Results of a Multinational, Multicenter, Observational Survey (DIAINFORM). Diabetes Ther 9, 1897–1906 (2018). https://doi.org/10.1007/s13300-018-0485-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-018-0485-2