Abstract
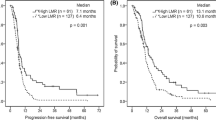
Lymphocyte to monocyte ratio (LMR) has shown prognostic value in different types of cancer. This study assessed the prognostic performance of LMR in early-stage non-small cell lung cancer (NSCLC) patients and investigated the influence of LMR on the treatment response in patients receiving first-line platinum-based chemotherapy. Four hundred eighty-eight NSCLC patients and 500 healthy donors were enrolled in this study. The cutoff value for LMR was chosen by receiver operating characteristic curve analysis. The prognostic significance of markers was assessed by univariate and multivariate Cox regression models. The median overall survival was 43 months, and the median progression-free survival was 38 months. LMR was associated with disease status and the treatment response of first-line platinum-based chemotherapy. Multivariate analysis showed that LMR was an independent prognostic factor for both overall survival (hazard ratio = 1.53, 95 % confidence interval = 1.09–2.14, P = 0.015) and progression-free survival (hazard ratio = 1.20, 95 % confidence interval = 1.02–1.67, P = 0.028). Furthermore, integration of LMR into a prognostic model including TNM stage, tumor status, chemotherapy, and histological type generated a nomogram, which predicted accurately overall survival for NSCLC patients. Decreased LMR may be a potential biomarker of disease status, worse response to first-line platinum-based chemotherapy, and worse survival for NSCLC patients. A prospective study is warranted for further validation of our findings.




Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
Casanovas O. Cancer: limitations of therapies exposed. Nature. 2012;484(7392):44–6. doi:10.1038/484044a.
Tanner NT, Sherman CA, Silvestri GA. Biomarkers in the selection of maintenance therapy in non-small cell lung cancer. Transl Lung Cancer Res. 2012;1(2):96–8. doi:10.3978/j.issn.2218-6751.2012.03.02.
Hwang JA, Song JS, Yu DY, Kim HR, Park HJ, Park YS, et al. Peroxiredoxin 4 as an independent prognostic marker for survival in patients with early-stage lung squamous cell carcinoma. Int J Clin Exp Pathol. 2015;8(6):6627–35.
Dotsch MM, Kloten V, Schlensog M, Heide T, Braunschweig T, Veeck J, et al. Low expression of ITIH5 in adenocarcinoma of the lung is associated with unfavorable patients’ outcome. Epigenetics. 2015. doi:10.1080/15592294.2015.1078049.
Donnem T, Bremnes RM, Busund LT, Andersen S, Pezzella F. Gene expression assays as prognostic and predictive markers in early stage non-small cell lung cancer. J Thorac Dis. 2012;4(2):212–3. doi:10.3978/j.issn.2072-1439.2012.03.02.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74. doi:10.1016/j.cell.2011.02.013.
Kim DK, Oh SY, Kwon HC, Lee S, Kwon KA, Kim BG, et al. Clinical significances of preoperative serum interleukin-6 and C-reactive protein level in operable gastric cancer. BMC Cancer. 2009;9:155. doi:10.1186/1471-2407-9-155.
Kishi Y, Kopetz S, Chun YS, Palavecino M, Abdalla EK, Vauthey JN. Blood neutrophil-to-lymphocyte ratio predicts survival in patients with colorectal liver metastases treated with systemic chemotherapy. Ann Surg Oncol. 2009;16(3):614–22. doi:10.1245/s10434-008-0267-6.
Deng Q, He B, Liu X, Yue J, Ying H, Pan Y, et al. Prognostic value of pre-operative inflammatory response biomarkers in gastric cancer patients and the construction of a predictive model. J Transl Med. 2015;13:66. doi:10.1186/s12967-015-0409-0.
Kumagai S, Marumo S, Shoji T, Sakuramoto M, Hirai T, Nishimura T, et al. Prognostic impact of preoperative monocyte counts in patients with resected lung adenocarcinoma. Lung Cancer. 2014;85(3):457–64. doi:10.1016/j.lungcan.2014.06.015.
Ozawa T, Ishihara S, Kawai K, Kazama S, Yamaguchi H, Sunami E, et al. Impact of a lymphocyte to monocyte ratio in stage IV colorectal cancer. J Surg Res. 2015. doi:10.1016/j.jss.2015.06.014.
Chang Y, An H, Xu L, Zhu Y, Yang Y, Lin Z, et al. Systemic inflammation score predicts postoperative prognosis of patients with clear-cell renal cell carcinoma. Br J Cancer. 2015;113(4):626–33. doi:10.1038/bjc.2015.241.
Cannon NA, Meyer J, Iyengar P, Ahn C, Westover KD, Choy H, et al. Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors after stereotactic radiation therapy for early-stage non-small-cell lung cancer. J Thorac Oncol. 2015;10(2):280–5. doi:10.1097/JTO.0000000000000399.
Botta C, Barbieri V, Ciliberto D, Rossi A, Rocco D, Addeo R, et al. Systemic inflammatory status at baseline predicts bevacizumab benefit in advanced non-small cell lung cancer patients. Cancer Biol Ther. 2013;14(6):469–75. doi:10.4161/cbt.24425.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. doi:10.1016/j.ejca.2008.10.026.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44. doi:10.1038/nature07205.
King PT. Inflammation in chronic obstructive pulmonary disease and its role in cardiovascular disease and lung cancer. Clin Transl Med. 2015;4(1):68. doi:10.1186/s40169-015-0068-z.
Germano G, Allavena P, Mantovani A. Cytokines as a key component of cancer-related inflammation. Cytokine. 2008;43(3):374–9. doi:10.1016/j.cyto.2008.07.014.
Dunn GP, Bruce AT, Ikeda H, Old LJ, Schreiber RD. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002;3(11):991–8. doi:10.1038/ni1102-991.
Siveen KS, Kuttan G. Role of macrophages in tumour progression. Immunol Lett. 2009;123(2):97–102. doi:10.1016/j.imlet.2009.02.011.
Heusinkveld M, van der Burg SH. Identification and manipulation of tumor associated macrophages in human cancers. J Transl Med. 2011;9:216. doi:10.1186/1479-5876-9-216.
Gordon S, Martinez FO. Alternative activation of macrophages: mechanism and functions. Immunity. 2010;32(5):593–604. doi:10.1016/j.immuni.2010.05.007.
Heusinkveld M, de Vos van Steenwijk PJ, Goedemans R, Ramwadhdoebe TH, Gorter A, Welters MJ, et al. M2 macrophages induced by prostaglandin E2 and IL-6 from cervical carcinoma are switched to activated M1 macrophages by CD4+ Th1 cells. J Immunol. 2011;187(3):1157–65. doi:10.4049/jimmunol.1100889.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7. doi:10.1038/nature01322.
Zhang J, Huang SH, Li H, Li Y, Chen XL, Zhang WQ, et al. Preoperative lymphocyte count is a favorable prognostic factor of disease-free survival in non-small-cell lung cancer. Med Oncol. 2013;30(1):352. doi:10.1007/s12032-012-0352-3.
Go SI, Kim RB, Song HN, Kang MH, Lee US, Choi HJ, et al. Prognostic significance of the lymphocyte-to-monocyte ratio in patients with small cell lung cancer. Med Oncol. 2014;31(12):323. doi:10.1007/s12032-014-0323-y.
Hu P, Shen H, Wang G, Zhang P, Liu Q, Du J. Prognostic significance of systemic inflammation-based lymphocyte-monocyte ratio in patients with lung cancer: based on a large cohort study. PLoS One. 2014;9(9), e108062. doi:10.1371/journal.pone.0108062.
Lin GN, Peng JW, Xiao JJ, Liu DY, Xia ZJ. Prognostic impact of circulating monocytes and lymphocyte-to-monocyte ratio on previously untreated metastatic non-small cell lung cancer patients receiving platinum-based doublet. Med Oncol. 2014;31(7):70. doi:10.1007/s12032-014-0070-0.
Author contributions
Conceived and designed the experiments: JT and YJS
Performed the experiments: YJS, LXW, YQH, ZHL, QT, and XZF
Analyzed the data: YJS and LXW
Contributed reagents/materials/analysis tools: LXW and YQH
Wrote the manuscript: YJS and JT
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Song, YJ., Wang, LX., Hong, YQ. et al. Lymphocyte to monocyte ratio is associated with response to first-line platinum-based chemotherapy and prognosis of early-stage non-small cell lung cancer patients. Tumor Biol. 37, 5285–5293 (2016). https://doi.org/10.1007/s13277-015-4397-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4397-8