Abstract
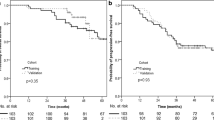
Inflammation has been demonstrated to be widely involved in the carcinogenesis of nasopharyngeal carcinoma (NPC). However, the prognostic significance of lymphocyte to monocyte ratio (LMR) in metastatic NPC is not fully addressed. The purpose of the study is to investigate the prognostic impact of pre-treatment absolute lymphocyte count (ALC), absolute monocyte count (AMC), and LMR on patients with newly diagnosed metastatic NPC undergoing chemotherapy. Between January 2006 and December 2010, patients with newly diagnosed metastatic NPC undergoing chemotherapy were retrospectively collected. The prognostic significance of baseline clinical features and inflammatory markers was investigated. A total of 256 patients were eligible for the study. The best cut-off value of ALC, AMC, and LMR was 2.25 × 109/L, 0.35 × 109/L, and 5.07, respectively. Patients in the high LMR group had a significantly longer overall survival (OS) (25.0 months [24.50–25.49]) than patients in the low LMR group (16.0 months [15.51–16.49]; p < 0.001). In addition, ALC ≥ 2.25 × 109/L (HR, 0.59; 95 % CI, 0.43–0.81; p = 0.001) and LMR ≥5.07 (HR, 0.42; 95 % CI, 0.30–0.59; p < 0.001) remained as independent prognostic factors for superior OS, while AMC did not retained its prognostic significance in COX multivariate analysis. Pre-treatment ALC and LMR were demonstrated to be independent prognostic factors in patient with newly diagnosed metastatic NPC receiving chemotherapy. Future prospective studies are needed to validate the findings.

Similar content being viewed by others
References
Jia WH, Huang QH, Liao J, et al. Trends in incidence and mortality of nasopharyngeal carcinoma over a 20–25 year period (1978/1983-2002) in Sihui and Cangwu counties in southern China. BMC Cancer. 2006;6:178.
Chen L, Hu CS, Chen XZ, et al. Concurrent chemoradiotherapy plus adjuvant chemotherapy versus concurrent chemoradiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma: a phase 3 multicenter randomized controlled trial. Lancet Oncol. 2012;13:163–71.
Lee AW, Lau WH, Tung SY, et al. Preliminary results of a randomized study on therapeutic gain by concurrent chemotherapy for regionally-advanced nasopharyngeal carcinoma: NPC-9901 Trial by the Hong Kong Nasopharyngeal Cancer Study Group. J Clin Oncol. 2005;23:6966–75.
Ma BB, Hui EP, Wong SC, et al. Multicenter phase II study of gemcitabine and oxaliplatin in advanced nasopharyngeal carcinoma–correlation with excision repair cross-complementing-1 polymorphisms. Ann Oncol. 2009;20:1854–9.
Li ZM, Huang JJ, Xia Y, et al. Blood lymphocyte-to-monocyte ratio identifies high-risk patients in diffuse large B-cell lymphoma treated with R-CHOP. PLoS One. 2012;7:e41658.
Koh YW, Kang HJ, Park C, Yoon DH, et al. The ratio of the absolute lymphocyte count to the absolute monocyte count is associated with prognosis in Hodgkin’s lymphoma: correlation with tumor-associated macrophages. Oncologist. 2012;17:871–80.
Li J, Jiang R, Liu WS, et al. A large cohort study reveals the association of elevated peripheral blood lymphocyte-to-monocyte ratio with favorable prognosis in nasopharyngeal carcinoma. PLoS One. 2013;8:e83069.
Liao Q, Zeng Z, Guo X, et al. LPLUNC1 suppresses IL-6-induced nasopharyngeal carcinoma cell proliferation via inhibiting the Stat3 activation. Oncogene. 2014;33:2098–109.
Liao Q, Guo X, Li X, et al. Analysis of the contribution of nasopharyngeal epithelial cancer cells to the induction of a local inflammatory response. J Cancer Res Clin Oncol. 2011;138:57–64.
Lee YY, Choi CH, Sung CO, et al. Prognostic value of pre-treatment circulating monocyte count in patients with cervical cancer: comparison with SCC-Ag level. Gynecol Oncol. 2012;124:92–7.
Shi C, Pamer EG. Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 2011;11:762–74.
Pollard JW. Tumor-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer. 2004;4:71–8.
Condeelis J, Pollard JW. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell. 2006;124:263–6.
Qian B, Deng Y, Im JH, et al. A distinct macrophage population mediates metastatic breast cancer cell extravasation, establishment and growth. PLoS One. 2009;4:e6562.
Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51.
Huh JW, Lee JH, Kim HR. Prognostic significance of tumor-infiltrating lymphocytes for patients with colorectal cancer. Arch Surg. 2012;147:366–72.
Mahmoud SM, Paish EC, Powe DG, et al. Tumor-infiltrating CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin Oncol. 2011;29:1949–55.
Tang Y, Xu X, Guo S, et al. An increased abundance of tumor-infiltrating regulatory T cells is correlated with the progression and prognosis of pancreatic ductal adenocarcinoma. PLoS One. 2014;9:e91551.
Teo PM, Kwan WH, Lee WY, Leung SF, Johnson PJ. Prognosticators determining survival subsequent to distant metastasis from nasopharyngeal carcinoma. Cancer. 1996;77:2423–31.
Hui EP, Leung SF, Au JS, et al. Lung metastasis alone in nasopharyngeal carcinoma: a relatively favorable prognostic group. A study by the Hong Kong Nasopharyngeal Carcinoma Study Group. Cancer. 2004;101:300–6.
Acknowledgments
The authors would like to thank the patients and their families.
Conflicts of interest
None
Author contributions
Conception and design: Xiao-Qin Chen, Gui-Nan Lin.
Collection and assembly of data: Gui-Nan Lin, Jie-Wen Peng, Jian-jun Xiao, Yue-Qiong Chen, Dong-Ying Liu.
Data analysis and interpretation: Xiao-Qin Chen, Gui-Nan Liu.
Manuscript writing: Xiao-Qin Chen, Gui-Nan Lin.
Final approval of manuscript: Gui-Nan Lin, Jie-Wen Peng, Dong-Ying Liu, Jian-jun Xiao, Yue-Qiong Chen, Xiao-Qin Chen.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, GN., Peng, JW., Liu, DY. et al. Increased lymphocyte to monocyte ratio is associated with better prognosis in patients with newly diagnosed metastatic nasopharyngeal carcinoma receiving chemotherapy. Tumor Biol. 35, 10849–10854 (2014). https://doi.org/10.1007/s13277-014-2362-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2362-6