Abstract
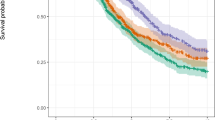
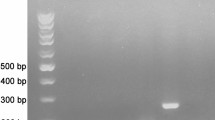
Altered expression of centromere protein-A (CENP-A) is observed in various types of human cancers. However, the clinical significance and pathological role of CENP-A in epithelial ovarian cancer (EOC) remains unclear. The main objective of this investigation was to clarify the relationships between CENP-A expression and the clinicopathological features of patients with EOC. Real-time quantitative PCR and Western blot were performed to examine CENP-A expression in 20 pairs of fresh-frozen EOC tissues and corresponding noncancerous tissues. Using immunohistochemistry, we performed a retrospective study of the CENP-A expression levels on 120 archival EOC paraffin-embedded samples. Prognostic outcomes correlated with CENP-A were examined using Kaplan–Meier analysis and Cox proportional hazards model. Our results showed that the expression levels of CENP-A mRNA and protein in EOC tissues were both significantly higher than those in noncancerous tissues. By immunohistochemistry, the data revealed that high CENP-A expression was significantly correlated with pathological grade (P = 0.02) and International Federation of Gynecology and Obstetrics stage (P = 0.006). Consistent with these results, we found that high expression of CENP-A was significantly correlated with poor survival in EOC patients (P < 0.001). Furthermore, Cox regression analyses showed that CENP-A expression was an independent predictor of overall survival. Our data suggest that CENP-A could play an important role in EOC and might serve as a valuable prognostic marker and potential target for gene therapy in the treatment of EOC.




Similar content being viewed by others
References
Tang L, Yang J, Ng SK, Rodriguez N, Choi PW, Vitonis A, et al. Autoantibody profiling to identify biomarkers of key pathogenic pathways in mucinous ovarian cancer. Eur J Cancer. 2010;46:170–9. doi:10.1016/j.ejca.2009.10.003.
Wu J, Liu Z, Shao C, Gong Y, Hernando E, Lee P, et al. HMGA2 overexpression-induced ovarian surface epithelial transformation is mediated through regulation of EMT genes. Cancer Res. 2011;71:349–59. doi:10.1158/0008-5472.CAN-10-2550.
Chambers SK, Clouser MC, Baker AF, Roe DJ, Cui H, Brewer MA, et al. Overexpression of tumor vascular endothelial growth factor A may portend an increased likelihood of progression in a phase II trial of bevacizumab and erlotinib in resistant ovarian cancer. Clin Cancer Res. 2010;16:5320–8. doi:10.1158/1078-0432.CCR-10-0974.
Lu L, Schwartz P, Scarampi L, Rutherford T, Canuto EM, Yu H, et al. MicroRNA let-7a: a potential marker for selection of paclitaxel in ovarian cancer management. Gynecol Oncol. 2011;122:366–71. doi:10.1016/j.ygyno.2011.04.033.
Noske A, Kaszubiak A, Weichert W, Sers C, Niesporek S, Koch I, et al. Specific inhibition of AKT2 by RNA interference results in reduction of ovarian cancer cell proliferation: increased expression of AKT in advanced ovarian cancer. Cancer Lett. 2007;246:190–200. doi:10.1016/j.canlet.2006.02.018.
Black BE, Jansen LE, Maddox PS, Foltz DR, Desai AB, Shah JV, et al. Centromere identity maintained by nucleosomes assembled with histone H3 containing the CENP-A targeting domain. Mol Cell. 2007;25:309–22. doi:10.1016/j.molcel.2006.12.018.
Li Y, Zhu Z, Zhang S, Yu D, Yu H, Liu L, et al. ShRNA-targeted centromere protein A inhibits hepatocellular carcinoma growth. PLoS One. 2011;6:e17794. doi:10.1371/journal.pone.0017794.
Tomonaga T, Matsushita K, Yamaguchi S, Oohashi T, Shimada H, Ochiai T, et al. Overexpression and mistargeting of centromere protein-A in human primary colorectal cancer. Cancer Res. 2003;63:3511–6.
Wu Q, Qian YM, Zhao XL, Wang SM, Feng XJ, Chen XF, et al. Expression and prognostic significance of centromere protein A in human lung adenocarcinoma. Lung Cancer. 2012;77:407–14. doi:10.1016/j.lungcan.2012.04.007.
McGovern SL, Qi Y, Pusztai L, Symmans WF, Buchholz TA. Centromere protein-A, an essential centromere protein, is a prognostic marker for relapse in estrogen receptor-positive breast cancer. Breast Cancer Res. 2012;14:R72. doi:10.1186/bcr3181.
Jordan SJ, Cushing-Haugen KL, Wicklund KG, Doherty JA, Rossing MA. Breast-feeding and risk of epithelial ovarian cancer. Cancer Causes Control. 2012;23:919–27. doi:10.1007/s10552-012-9963-4.
Rota M, Pasquali E, Scotti L, Pelucchi C, Tramacere I, Islami F, et al. Alcohol drinking and epithelial ovarian cancer risk. a systematic review and meta-analysis. Gynecol Oncol. 2012;125:758–63. doi:10.1016/j.ygyno.2012.03.031.
Wang M, He Y, Shi L, Shi C. Multivariate analysis by Cox proportional hazard model on prognosis of patient with epithelial ovarian cancer. Eur J Gynaecol Oncol. 2011;32:171–7.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qiu, JJ., Guo, JJ., Lv, TJ. et al. Prognostic value of centromere protein-A expression in patients with epithelial ovarian cancer. Tumor Biol. 34, 2971–2975 (2013). https://doi.org/10.1007/s13277-013-0860-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-013-0860-6