Abstract
Purpose
To look for endocrine abnormalities like thyroid disorders, hyperprolactinemia, hyperandrogenism and PCOS among adolescents with menstrual disorders and to compare the above endocrine status with those without menstrual disorders.
Methods
This was a case–control study carried out in adolescent girls aged 10–19 years in gynecology outpatient department of a tertiary care hospital. Sample of venous blood (5 ml) was taken for hormonal studies as clinically indicated—thyroid function test, serum prolactin, total testosterone, which were analyzed by chemiluminescence system.
Results
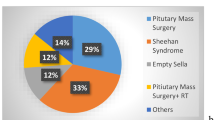
Oligomenorrhea was the most common menstrual abnormality in our study, the prevalence being 61.0% in cases followed by primary amenorrhea (16.4%). Thyroid dysfunction was found in 13.6% girls with menstrual disorders compared to 3.5% in those without menstrual disorders, and this was statistically significant (p = 0.006). Biochemical hyperandrogenism was seen in 9.04% cases compared to 0.7% controls (p = 0.001). The overall prevalence of hyperprolactinemia was 0.94%, and there was no statistically significant difference in girls with and without menstrual disorders. The prevalence of PCOS was 12.4% in the study population and 22.6% cases. Oligomenorrhea and PCOS were the most prevalent phenotypes in 52.5% of PCOS girls. No endocrine abnormality was detected in cases of polymenorrhea, hypomenorrhea and intermenstrual bleeding.
Conclusions
Although immaturity of hypothalamic pituitary ovarian axis is considered to be the most common cause of menstrual irregularities in adolescent girls, endocrine abnormalities, namely thyroid dysfunction and hyperandrogenism, may be responsible in some cases, thus warranting further evaluation.
Similar content being viewed by others
References
Parker MA, Sneddon AE, Arbon P. The menstrual disorder of teenagers (MDOT) study: determining typical menstrual patterns and menstrual disturbance in a large population-based study of Australian teenagers. BJOG. 2010;117(2):185–92.
Kakuno Y, Amino N, Kanoh M, et al. Menstrual disturbances in various thyroid diseases. Endocr J. 2010;57(12):1017–22.
Lee DY, Oh YK, Yoon BK, et al. Prevalence of hyperprolactinemia in adolescents and young women with menstruation-related problems. Am J Obstet Gynecol. 2012;206(3):213–5.
Nidhi R, Padmalatha V, Nagarathna R, et al. Prevalence of polycystic ovarian syndrome in Indian adolescents. J Pediatr Adolesc Gynecol. 2011;24(4):223–7.
Rigon F, De Sanctis V, Bernasconi S, et al. Menstrual pattern and menstrual disorders among adolescents: an update of the Italian data. Ital J Pediatr. 2012;38:38.
Rosenfield RL. Clinical review: adolescent anovulation: maturational mechanisms and implications. J Clin Endocrinol Metab. 2013;98(9):3572–83.
Chhabra S, Venkatraman S. Menstrual dysfunction in rural young women and the presence of polycystic ovarian syndrome. J Obstet Gynaecol. 2010;30(1):41–5.
Chung PW, Chan SS, Yiu KW, et al. Menstrual disorders in a paediatric and adolescent gynaecology clinic: patient presentations and longitudinal outcomes. Hong Kong Med J. 2011;17(5):391–7.
Zegeye DT, Megabiaw B, Mulu A. Age at menarche and the menstrual pattern of secondary school adolescents in northwest Ethiopia. BMC Womens Health. 2009;9:29.
Abraham R, Srinivasa Murugan V, Pukazhvanthen P, et al. Thyroid disorders in women of Pondicherry. Indian J Clin Biochem. 2009;24(1):52–9.
Joshi B, Mukherjee S, Patil A, et al. A cross-sectional study of polycystic ovarian syndrome among adolescent and young girls in Mumbai, India. Indian J Endocrinol Metab. 2014;18(3):317–24.
Chen X, Yang D, Mo Y, et al. Prevalence of polycystic ovary syndrome in unselected women from southern China. Eur J Obstet Gynecol Reprod Biol. 2008;139(1):59–64.
Hickey M, Doherty DA, Atkinson H, et al. Clinical, ultrasound and biochemical features of polycystic ovary syndrome in adolescents: implications for diagnosis. Hum Reprod. 2011;26(6):1469–77.
Acknowledgements
We acknowledge Dean research, JIPMER for granting intramural fund of Rs. 1 lakh for PG Project utilized for hormone kits, reagents, calibrators (Circular No. Edn. 7(1)/2012, dated 28.9.2012).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Informed consent in studies with human subjects
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Declaration of Helsinki of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
Additional information
Dr. Siddhesh R. Rajiwade is a Senior Resident in the Department of Obstetrics and Gynecology, JIPMER, Puducherry, 605006 India; Dr. Haritha Sagili is a Additional Professor in the Department of Obstetrics and Gynecology, JIPMER, Puducherry, 605005 India; Dr. R. Soundravally is a Additional Professor in the Department of Biochemistry, JIPMER, Puducherry, 605006 India; Dr. L. Subitha is a Assistant Professor, Department of Preventive and Social medicine, JIPMER, Puducherry, 605006 India.
Rights and permissions
About this article
Cite this article
Rajiwade, S.R., Sagili, H., Soundravally, R. et al. Endocrine Abnormalities in Adolescents with Menstrual Disorders. J Obstet Gynecol India 68, 58–64 (2018). https://doi.org/10.1007/s13224-017-1035-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-017-1035-y