Abstract
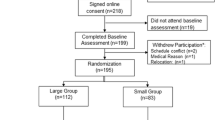
While group interventions for weight management have been shown to be efficacious, adherence is often low, especially among men. This pilot study seeks to test whether group interventions using web-based group video conferencing (VC) technology is effective for weight loss. We adapted a 12-week curriculum based on the Diabetes Prevention Program, and delivered this intervention to a small group of men (BMI ≥30 kg/m2), using web-based group VC. Participants were randomized to intervention (n = 32) or delayed-intervention control group (n = 32). The intervention group lost 3.5 % (95 % CI 2.1 %, 4.9 %) of their initial body weight. Difference in mean weight loss was 3.2 kg (p = 0.0002) and mean BMI decrease was 1.0 kg/m2 (p = 0.0010) between the two groups. Virtual small groups may be an effective means of allowing face-to-face group interaction, while overcoming some barriers to access.



Similar content being viewed by others
References
Flegal KM et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012; 307(5): 491-7.
Rao G, Kirley K. The future of obesity treatment: comment on “integrating technology into standard weight loss treatment: a randomized controlled trial”. JAMA Int Med. 2013; 173(2): 111-112.
Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet. 2009; 374(9702): 1677-86.
Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the look AHEAD trial. Arch Intern Med. 2010; 170(17): 1566-75.
Sarwer DB et al. Behavior therapy for obesity: where are we now? Curr Opin Endocrinol Diabetes Obes. 2009; 16(5): 347-52.
Pi-Sunyer X et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007; 30(6): 1374-83.
Knowler WC et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346(6): 393-403.
Knowler WC et al. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet. 2009; 374(9702): 1677-86.
Wadden TA et al. The look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring). 2006; 14(5): 737-52.
DePue JD et al. Maintenance of weight loss: a needs assessment. Obes Res. 1995; 3(3): 241-8.
Verheijden MW et al. Role of social support in lifestyle-focused weight management interventions. Eur J Clin Nutr. 2005; 59(Suppl 1): S179-86.
Black DR, Gleser LJ, Kooyers KJ. A meta-analytic evaluation of couples weight-loss programs. Health Psychol. 1990; 9(3): 330-47.
Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol. 1988; 7(3): 269-97.
Paul-Ebhohimhen V, Avenell A. A systematic review of the effectiveness of group versus individual treatments for adult obesity. Obes Facts. 2009; 2(1): 17-24.
Appel LJ, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011
Ockene IS et al. Outcomes of a Latino community-based intervention for the prevention of diabetes: the Lawrence Latino diabetes prevention project. Am J Public Health. 2012; 102(2): 336-342.
Palaniappan LP et al. Shared medical appointments: promoting weight loss in a clinical setting. J Am Board Fam Med. 2011; 24(3): 326-8.
Sabinsky MS et al. Overweight men’s motivations and perceived barriers towards weight loss. Eur J Clin Nutr. 2007; 61(4): 526-31.
Wolfe BL, Smith JE. Different strokes for different folks: why overweight men do not seek weight loss treatment. Eat Disord. 2002; 10(2): 115-24.
Knowler WC et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346(11832527): 393-403.
Orchard TJ et al. The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: the diabetes prevention program randomized trial. Ann Intern Med. 2005; 142(8): 611-9.
Wing RR et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res. 2004; 12(15483207): 1426-1434.
Hamman RF et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006; 29(9): 2102-7.
Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the diabetes prevention program? Health Aff (Millwood). 2012; 31(22232096): 67-75.
Tsai AG, Wadden TA. Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med. 2005; 142(1): 56-66.
Zickuhr K, Smith A, Home Broadband. Pew research center’s internet & American life project2013. Washington D.C: Pew Research Center; 2013.
Pew Internet & American Life Project. Latinos Online, 2006-2008: Narrowing the Gap. 2009 [cited 2010 January 5]; Available from: http://pewhispanic.org/files/reports/119.pdf.
Sarasohn-Kahn J. How Smarphones Are Changing Health Care for Consumers and Providers, April 2010, California HealthCare Foundation.
Birden H, Page S. Teaching by videoconference: a commentary on best practice for rural education in health professions. Rural Remote Health. 2005; 5(2): 356.
Gagnon MP et al. Implementing telehealth to support medical practice in rural/remote regions: what are the conditions for success? Implement Sci. 2006; 1: 18.
Moehr JR et al. Success factors for telehealth—a case study. Int J Med Inform. 2006; 75(10–11): 755-63.
Augestad KM, Lindsetmo RO. Overcoming distance: video-conferencing as a clinical and educational tool among surgeons. World J Surg. 2009; 33(7): 1356-65.
McLean S et al. Telehealthcare for asthma. Cochrane Database Syst Rev. 2010; 10, CD007717.
Vyzula R. Oncologists use a communication system for videoconferencing. Klin Onkol. 2010; 23(2): 124.
Kitamura C, Zurawel-Balaura L, Wong RK. How effective is video consultation in clinical oncology? a systematic review. Curr Oncol. 2010; 17(3): 17-27.
Hassija C, Gray MJ. The effectiveness and feasibility of videoconferencing technology to provide evidence-based treatment to rural domestic violence and sexual assault populations. Telemed J Eng Health. 2011; 17(4): 309-15.
Kobak KA, Williams JB, Engelhardt N. A comparison of face-to-face and remote assessment of inter-rater reliability on the Hamilton depression rating scale via videoconferencing. Psychiatry Res. 2008; 158(1): 99-103.
Kobak KA et al. Face-to-face versus remote administration of the Montgomery-Asberg depression rating scale using videoconference and telephone. Depression Anxiety. 2008; 25(11): 913-9.
Modai I et al. Cost effectiveness, safety, and satisfaction with video telepsychiatry versus face-to-face care in ambulatory settings. Telemed J Eng Health. 2006; 12(5): 515-20.
O’Reilly R et al. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr Serv. 2007; 58(6): 836-43.
Strachan M et al. Home-based telehealth to deliver evidence-based psychotherapy in veterans with PTSD. Contemp Clin Trials. 2012; 33(2): 402-9.
Tuerk PW et al. A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. J Trauma Stress. 2010; 23(1): 116-23.
E, D.E.W., et al. Implementing video conferencing in mental health practice. J Psychiatr Ment Health Nurs. 2012.
Marhefka SL, et al. Interest in, concerns about, and preferences for potential video-group delivery of an effective behavioral intervention among women living with HIV. AIDS Behav. 2011.
Verhoeven F et al. The contribution of teleconsultation and videoconferencing to diabetes care: a systematic literature review. J Med Internet Res. 2007; 9(5): e37.
Morland LA et al. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress. 2011; 24(4): 465-9.
Ahrendt AD, et al. The Effectiveness of Telemedicine for Weight Management in the MOVE! Program. J Rural Health : Off J Am Rural Health Assoc Natl Rural Health Care Assoc. 2013.
Dehghani P et al. Management of adults with congenital heart disease using videoconferencing across Western Canada: a 3-year experience. Can J Cardiol. 2013; 29(7): 873-8.
Vadheim LM et al. Adapted diabetes prevention program lifestyle intervention can be effectively delivered through telehealth. Diabetes Educ. 2010; 36(4): 651-6.
Arain M et al. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol. 2010; 10(1): 67.
Kramer MK et al. Translating the diabetes prevention program: a comprehensive model for prevention training and program delivery. Am J Prev Med. 2009; 37(6): 505-11.
Kramer MK et al. A novel approach to diabetes prevention: evaluation of the group lifestyle balance program delivered via DVD. Diabetes Res Clin Pract. 2010; 90(3): e60-3.
Steinberg DM, et al. The efficacyof adaily self-weighing weight loss intervention using smart scales and email. Obesity. 2013.
Blackburn G. Effect of degree of weight loss on health benefits. Obes Res. 1995; 3(2): 211s-216s.
The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999; 22(4): 623-34.
The Diabetes Prevention Program (DPP). Description of lifestyle intervention. Diabetes Care. 2002; 25(12): 2165-71.
Ogden CL, et al. Prevalence of obesity in the United States, 2009-2010. NCHS Data Brief, 2012(82): 1–8.
Mozaffarian D et al. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011; 364(25): 2392-404.
Volkmar FR et al. High attrition rates in commercial weight reduction programs. Arch Intern Med. 1981; 141(4): 426-8.
Anderson JW et al. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001; 74(5): 579-84.
Dalle Grave R et al. Weight loss expectations in obese patients seeking treatment at medical centers. Obes Res. 2004; 12(12): 2005-12.
Venditti EM et al. First versus repeat treatment with a lifestyle intervention program: attendance and weight loss outcomes. Int J Obes. 2008; 32(10): 1537-44.
Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res. 2004; 12(Suppl): 151S-62S.
Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011; 111(21185970): 92-9102.
McGuire MT et al. Behavioral strategies of individuals who have maintained long-term weight losses. Obes Res. 1999; 7(4): 334-41.
Steinberg DM et al. The efficacy of a daily self-weighing weight loss intervention using smart scales and e-mail. Obesity. 2013; 21(9): 1789-97.
Arem H, Irwin M. A review of web-based weight loss interventions in adults. Obes Rev. 2011; 12(20804523): 236-243.
Centers for Medicare and Medicaid Services. Telehealth Services. 2009 [cited 2012 May]; Available from: http://www.telemedicine.com/pdfs/TelehealthSrvcsfctsht.pdf.
National Conference of State Legislatures. State Coverage for Telehealth Services. 2013 [cited 2013 October]; Available from: http://www.ncsl.org/issues-research/health/state-coverage-for-telehealth-services.aspx.
American Psychological Association Practice Organization. Reimbursement for telehealth services. 2011 [cited 2013 October]; Available from: http://www.apapracticecentral.org/update/2011/03-31/reimbursement.aspx.
American Telemedicine Association. Telemedicine in the Patient Protection and Affordable Care Act 2010; Available from: http://www.americantelemed.org/docs/default-source/policy/telehealth-provisions-within-the-patient-protection-and-affordable-care-act.pdf?sfvrsn=14.
Acknowledgments
This was an investigator-initiated study funded by a grant from the Verizon Foundation. The funders played no role in the design, conduct, or analysis of the study, nor in the interpretation and reporting of the study findings. The researchers were independent from the funders. The authors would like to thank Marina Dolginsky, BS, for her help in the administrative support of this study.
Conflict of interest
All authors declare that they have no conflicts of interest.
Adherence to ethical principles
All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000
Author information
Authors and Affiliations
Corresponding author
Additional information
Implications
Policy: Given the transformation of health care and payment models from being illness-centric to prevention-centric, the future of effective obesity treatment lies in the use of technology to improve clinical care.
Research: Video conferencing technology may be a cutting-edge alternative means of translating evidence-based, group behavioral weight management interventions into real-world setting.
Practice: Health care providers, peer support, and health services can be accessed in the convenience of your own home or office, providing the benefits of attending the in-person group meetings without the inconvenience of coming to the clinic.
About this article
Cite this article
Azar, K.M.J., Aurora, M., Wang, E.J. et al. Virtual small groups for weight management: an innovative delivery mechanism for evidence-based lifestyle interventions among obese men. Behav. Med. Pract. Policy Res. 5, 37–44 (2015). https://doi.org/10.1007/s13142-014-0296-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-014-0296-6