Abstract
Purpose
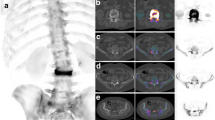
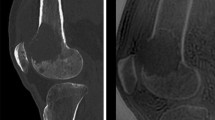
For the precise imaging diagnosis of osteoid osteoma (OO), the identification of the nidus and fibrovascular zone (FVZ) is essential. However, the latter sign has received little attention because it is difficult to demonstrate. We applied the recently introduced gamma correction (GC) to depict the FVZ on pinhole bone scan (PBS), conventional radiography (CR), and computed tomography (CT). Non-gamma correction MRI was also analyzed for reference.
Methods
Ten patients with histologically proven diagnoses of OO were enrolled in this retrospective study. PBS, CR, and CT were processed by GC to demonstrate the nidi and FVZ as distinct yet integrating components of OO. PBS was performed using a 4-mm pinhole collimator 3 h after iv injection of 925 to 1,110 MBq (25 to 30 mCi) of Tc-99m HDP, and anteroposterior and mediolateral CR and transverse CT were taken according to the standard technique. MRI sequences included T1- and T2-weighted images. For gamma correction, we utilized the Photo Correction Wizard program of ACD Photo Editor v3.1. A team of three qualified nuclear physician-radiologists, two nuclear physicians, and one MRI specialist read bone scans, radiographs, and MRIs of OO according to each specialty, and orthopaedic aspects and histology were reviewed by one qualified orthopedic surgeon and two qualified pathologists, respectively. Each observer first read the images separately with basic information about the aim of the study given and then in concert. Interpretive disagreement was settled by discussion and consensus.
Results
On pinhole scan, nidi were presented as areas of intense tracer uptake in all cases, and, importantly after GC, a thin ring-like zone with lower tracer uptake became visible in seven out of ten cases. GCCR also revealed a thin lucent zone that circumscribed the nidi in six out of ten cases and GCCT in two of four cases. MRI, without GC, presented nidi with high signal in the center and a thin ring-like zone with low signal in the periphery in five out of six cases. Ring-like zones were 1–2 mm in thickness and circumscribed the nidus as an integrated part and, hence, were morphologically interpreted as FVZ. Histologically, the presence of a variously mineralized FVZ was confirmed in four cases, but individual locus-by-locus image-histology correlation could not be accompolished because specimens were fragmentary. In the FVZ, tracer uptake was lower than in nidi, presumably reflecting that bone metabolism in the two parts differs as in their histology. Statistically, no significant correlation existed between the duration of symptoms and imaging demonstrability of the FVZ (Spearman’s test r = −0.057, p = 0.877), but parallelism existed in the demonstrability of the FVZ among GC PBS, CR, and CT, and non-correction MRI.
Conclusions
GC was useful to enhance the resolution of PBS, CR, and CT in OO so that both the nidi and FVZ were separately imaged. The use of CG PBS and CR in combination is recommended for the specific diagnosis of OO with information about bone metabolism and anatomical characteristics. PBS and CR are economical and widely available.







Similar content being viewed by others
References
Bahk YW, Jeon HS, Kim JM, Park JM, Chung YA, Kim EE, et al. Novel use of gamma correction for precise (99 m)Tc-HDP pinhole bone scan diagnosis and classification of knee occult fractures. Skeletal Radiol. 2010;39:807–13.
Picci P, Mirra JM. Osteoid Osteoma. In: Mirra JM, editor. Bone tumors. Philadelphia: Lea & Febiger; 1989. p. 226–48.
O'Connell JX, Nanthakumar SS, Nielsen GP, Rosenberg AE. Osteoid osteoma: the uniquely innervated bone tumor. Mod Pathol. 1998;11:175–80.
Hasegawa T, Hirose T, Sakamoto R, Seki K, Ikata T, Hizawa K. Mechanism of pain in osteoid osteomas: an immunohistochemical study. Histopathology. 1993;22:487–91.
Freiberger RH, Loitman BS, Helpern M, Thompson TC. Osteoid osteoma; a report on 80 cases. Am J Roentgenol Radium Ther Nucl Med. 1959;82:194–205.
Aisen AM, Glazer GM. Diagnosis of osteoid osteoma using computed tomography. J Comput Tomogr. 1984;8:175–8.
Assoun J, Richardi G, Railhac JJ, Baunin C, Fajadet P, Giron J, et al. Osteoid osteoma: MR imaging versus CT. Radiology. 1994;191:217–23.
Spouge AR, Thain LM. Osteoid osteoma: MR imaging revisited. Clin Imaging. 2000;24:19–27.
Harish S, Saifuddin A. Imaging features of spinal osteoid osteoma with emphasis on MRI findings. Eur Radiol. 2005;15:2396–403.
Helms CA, Hattner RS, Vogler 3rd JB. Osteoid osteoma: radionuclide diagnosis. Radiology. 1984;151:779–84.
Kim JY, Chung SK, Park YH, Kim SH, Shinn KS, Bahk YW. Pinhole bone scintigraphic appearances of osteoid osteoma. Korean J Nucl Med. 1992;26:160–3.
Mahboubi S. CT appearance of nidus in osteoid osteoma versus sequestration in osteomyelitis. J Comput Assist Tomogr. 1986;10:457–9.
Resnick D, Kyriakos M, Greenway GD. Tumors and tumor-like lesions of bone: imaging and pathology of specific lesions. In: Resnick D, Niwayama G, editors. Diagnosis of bone and joint disorders. 2nd ed. Philadelphia: WB Saunders; 1988. p. 3613–888.
Bahk YW, Bahk WJ. Malignant bone tumors. In: Bahk YW, editor. Combined scintigraphic and radiographic diagnosis of bone and joint diseases. 3rd ed. Springer: Heidelberg; 2007. p. 359–403.
Acknowledgments
Special thanks are due to Dr. Yoon Kwang Kim, Chairman of the Sung-Ae Medical Foundation, for his generous support. The authors are also grateful to Miss Mi Hye Chae for faithful secretarial contributions and Mr. Byong Heon Jeon for computer engineering.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bahk, YW., Kim, S.H., Chung, YA. et al. Depiction of Nidi and Fibrovascular Zones of Osteoid Osteomas Using Gamma-Correction Tc-99m HDP Pinhole Bone Scan and Conventional Radiograph, and Correlation with CT, MRI, and PVC Phantom Imaging. Nucl Med Mol Imaging 45, 21–29 (2011). https://doi.org/10.1007/s13139-010-0073-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-010-0073-5