Abstract
People who are aware that they are gene-positive for Huntington’s disease (HD) may face an array of personal, relationship, social, financial and employment challenges prior to the onset of the disease. These challenges have been associated with increased psychological problems such as anxiety and depression. Information and support for people with pre-symptomatic HD is indicated, but there is a scarcity of research and service models to inform psychological interventions. We trialled an intervention strategy involving psychoeducation forums designed specifically for pre-symptomatic HD. In phase I of the study, we asked people with pre-symptomatic HD to identify their uppermost needs for information. Phase II involved the delivery of this information via a series of forums. The forums also provided an opportunity for interaction among the participants. Three forums were attended by 88 people with pre-symptomatic HD and significant others. Analysis of post-forum feedback questionnaires indicated high levels of satisfaction with the forums’ structure, content and relevance, and notably, the pre-symptomatic specificity of focus. Additional qualitative data from recordings of forum discussion groups revealed that participants greatly valued the opportunity to meet similar others, and share their concerns and strategies for addressing these concerns. There was an abundance of requests for more forums on a wide range of relevant topics. It is recommended that this model of intervention may be of value for implementation in other HD services or community groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Huntington’s disease (HD) is an autosomal dominant neurodegenerative disease, characterised by a triad of cognitive, psychiatric and motor symptoms that progress over time (Reiner et al. 2011). Pre-symptomatic HD is the period of time prior to the development of HD symptoms in HD gene-positive individuals (Duff et al. 2008). With predictive testing available at age 18 (CGE 2017), and an average disease age onset of 40 (Myers 2004), a gene-positive individual could spend a significant portion of their life in the pre-symptomatic period. The name ‘pre-symptomatic’ can give a false impression of a time untroubled by the disease. While the actual disease symptoms may not yet have manifested, this period may in fact pose significant personal, social, psychological, work and familial HD-related challenges. These may develop even prior to having a gene test and can include a sense of hopelessness, powerlessness and self-restriction of life choices, and then further adverse psychological effects may develop subsequent to the gene test, regardless of the test result being positive or negative (Tilleras et al. 2020). For those who are gene-positive, they then face living with uncertainty about the timing of illness onset and a foreshortened lifespan; hypervigilance for early signs of the disease; the impact of being gene positive on personal identity, relationships and reproductive choices; the burden of care of a parent with HD; the widespread lack of understanding about HD and societal barriers to openness in discussing these issues (Ho and Hocaoglu 2011; Timman et al. 2004). Research has documented an increased risk of psychological difficulties in the pre-symptomatic period, including anxiety, hostility, interpersonal sensitivity, obsessive-compulsiveness, irritability, depression and suicide risk, with indications of intensified symptoms prior to the onset of manifest disease (Duff et al. 2007; Honrath et al. 2018).
Despite the breadth and depth of these challenges, there has been minimal research into the range of support needs specific to people with pre-symptomatic HD. One significant exception is a large international study by Braisch et al. (2016) that surveyed 683 young adults from HD families, of whom 54% were at risk of HD but not tested, and 28% were confirmed as gene positive. The findings showed that aside from general information about HD and predictive testing, the majority of participants lacked vital information about and support with multiple important issues. These issues pertained to legal concerns, lifestyle recommendations (exercise, diet, stress management), caregiving, relationship issues and knowing how to talk with their children about HD. This lack of information and support suggests a need for intervention programs specific to pre-symptomatic HD, and these also appear lacking in the literature.
Only three intervention studies were identified in a literature search focussed on pre-symptomatic HD needs (A’Campo et al. 2012; Eccles et al. 2020; Stopford et al. 2020). A’Campo et al. (2012) conducted an 8-week psychoeducation and cognitive behaviour therapy program to improve coping skills in HD and created a separate group for pre-symptomatic individuals. Unfortunately, there was a large drop-out rate and limited evidence of positive impact. In a second study, Eccles et al. (2020) explored the feasibility of an 8-week mindfulness-based cognitive therapy group program. Participants found the program helpful, with reductions in stress and improvements in some elements of mindfulness noted. A third study assessed group narrative therapy for a small sample (n = 6) of people with pre-symptomatic HD, with results indicating that participants found the experience normalising and de-isolating (Stopford et al. 2020). Recently, Zarotti et al. (2020) have made a ‘call to arms’ encouraging further psychological intervention research for people across the clinical trajectory of HD. They highlighted that the mental health benefits of psychological interventions are likely to be greatest for those in the pre-symptomatic, prodromal and early stages.
The present study aimed to address the identified need for improved access to information and support for individuals with pre-symptomatic HD. A consumer-informed approach was adopted in developing the psychoeducational intervention, in line with the Australian health-care policy impetus to partner with consumers in the planning, design and evaluation of health initiatives (ACSQHC 2017). The benefits of consumer-driven research include improvements to the patient-centredness of research design and outcomes, better recruitment and retention rates, greater relevance of the research and greater accountability to and empowerment of the consumer group (Harrison et al. 2019). We aimed to maximise the relevance for people with pre-symptomatic HD, so began with a survey of the information and support needs that are specific to this consumer group. Based on the survey results, we then developed and delivered a psychoeducational intervention that targeted the top consumer-identified needs. Participant experiences and feedback about the intervention were documented in order to evaluate the program.
Methods
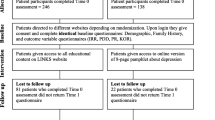
The study comprised two phases. In the first phase, we surveyed people with pre-symptomatic HD about their perceived needs for information and support relevant to HD. In the second phase, we responded to the survey data by developing and delivering a series of three targeted psychoeducation and support forums (Fig. 1).
Phase I: Psychoeducation needs identification
Potential participants for this study phase included individuals with pre-symptomatic HD who consecutively attended routine consultations with an HD nurse (LM, second author) over a one-month period at the Statewide Progressive Neurological Diseases Service (SPNDS), Calvary Healthcare Bethlehem. The SPNDS provides assessment and treatment for a range of progressive neurological diseases including HD, using the skills of a multidisciplinary team comprising neurologists, psychiatrists, nurses and allied health clinicians. Information about the study was provided at the HD nurse consultation, and those who agreed to participate provided written informed consent. Twenty-two individuals agreed to participate and were sent an online survey.
The survey was developed by the authors. It requested that respondents indicate their preferences for information about a range of possible topics, including many that are frequent subjects of inquiry and interest during phone and clinic consultations, such as HD research updates, anxiety about symptom onset, and disclosure obligations. The survey also provided scope for respondents to add their own additional topics of interest. Respondents were invited to nominate their top three information preferences. We also asked four scoping questions exploring participants’ perceived level of knowledge about HD, their frequency of communication with family and friends about HD and their interest in meeting others with pre-symptomatic HD. They were asked to respond to these four questions on a 4-point Likert rating scale (low/minimal/moderate/high). A final question asked participants whether they would be interested in attending information and support forums.
Phase II: Psychoeducation intervention
Topics that were rated as of greatest interest to consumers in Phase I were chosen for the intervention phase (Phase II). Phase II provided a series of information forums, addressing these top topics of interest and inviting those with pre-symptomatic HD that attend the SPNDS. Experts in the identified specialist topics were sourced from within and outside our service and were invited to present at the relevant forum by the research team. The first two forums occurred bi-monthly over the subsequent months. The final forum was delayed due to the onset of COVID-19 pandemic restrictions and was ultimately delivered via videoconference.
For each of the forums, we sent an initial email invitation to people with pre-symptomatic HD who attend our clinic. Those who replied with an ‘expression-of-interest’ response were sent additional information, including consent details and advice that the forums would be audio recorded. Further to requests from respondents, attendance was opened to significant others including family members or partners. For each forum, a completed consent form was necessary for the provision of an entry ticket.
The structure of the forums included a 40-min presentation on the selected topic, followed by a 10-min refreshment break, small discussion groups for 30 min and finally re-joining the larger group for closure and completion of the Forum Feedback Questionnaire. The written questionnaire used in the first two forums was translated into an online version for the third (videoconference) forum. The alteration to videoconference delivery for the third forum meant that while no small discussion groups occurred, participants were still able to ask questions and make comments. These were communicated verbally (via a moderator) and in writing (via chat box) during and after the course of the presentation.
The Forum Feedback Questionnaire consisted of two sections. In the first section, we asked the participants to rate their satisfaction (low/mild/moderate/high) with five aspects of the forum. Specifically, ratings were sought in relation to (1) the quality of the speaker’s presentation, (2) the speaker’s responses to comments and questions, (3) the opportunity to meet others in a similar situation (first two forums only), (4) their perceived increase in knowledge of HD and (5) the relevance of the content to their needs. We analysed and summarised these results using descriptive statistics.
The second section of the Forum Feedback Questionnaire inquired about participants’ experience of the forum and included questions about the following: the choice to restrict the focus to pre-symptomatic HD, the timing and length of the forum, the best aspect of the forum, barriers to attendance and additional topics of interest for potential future forums. We obtained further qualitative data from the audio recordings of the small discussion groups that occurred in the first two forums. Each small discussion group was facilitated by a member of the SPNDS HD team. They were semi-structured, with guiding questions that were derived from the presentation. Participants were invited to reflect these questions and how the topic related to their lived experience. The audio recordings were transcribed and subjected to thematic analysis by the first author. A modified phenomenological approach was followed, which involved reflecting on the meaning of the transcribed text responses, paying attention to the similarities and differences in experiences, summarising descriptions of the text in a table, identifying core themes and providing examples of the themes (Smith 2003).
This project received ethics approval from the Calvary Health Care Bethlehem Research Ethics and Ethics Committee (HREC number 19041801).
Results
Phase I: Psychoeducation needs identification
Fifteen individuals responded to the online survey out of the twenty-two that had agreed to participate (response rate: 68%). The issues that were nominated as of greatest interest included (1) HD research (67%); (2) preparing for financial and legal issues such as superannuation, insurance and employment discrimination (53%); (3) the value of exercise (47%); (4) managing fears of future HD (47%); (5) family care pressures (33%); (6) an update of HD knowledge (27%) and (7) dealing with disclosure and stigma (20%). Other topics raised by respondents included reproductive choices, differentiating normal ageing from HD progression, HD treatments, access to assisted dying, impact of diet and alcohol, how to delay disease onset and quality of life at the different stages of HD. The top four topics were selected to be covered in the three planned forums.
In relation to the four scoping questions about HD knowledge and communication, the modal response for each issue was as follows: ‘moderate’ for their current level of knowledge about HD (n = 10), ‘minimal’ for their likelihood of discussing HD with friends (n = 8), ‘moderate’ for their likelihood of discussing HD with family (n = 9) and ‘minimal’ for the importance to them of meeting others with HD (n = 6). Ninety two per cent indicated interest in attending the forums.
Phase II: Psychoeducation intervention
The top four topics identified in phase I were chosen as the focus of three psychoeducational forums. Topics and presenters were:
-
Forum 1— The Value of Physical Activity and Managing HD Future Fears: senior clinicians in physiotherapy and clinical psychology from SPNDS
-
Forum 2— HD Research: an international specialist in the cognitive neuroscience of HD
-
Forum 3— Preparing for Financial and Legal Issues: a lawyer and specialist in financial issues pertaining to genetic and terminal illness, together with a senior consultant nurse from the HD service at the SPNDS.
Eighty-eight people participated in at least one of the three forums: n = 20 (15 HD, 5 significant others) at forum 1, n = 31 (21 HD, 10 significant others) at forum 2 and n = 37 (32 HD, 5 significant others) at forum 3. Eight additional people provided prior consent but did not attend forums, with reasons provided including work or child-care demands. Of the 88 attendees, 72 (82%) completed the Forum Feedback Questionnaire relating to the forum that they attended. In summarising ratings across all three forums, responses indicated predominantly moderate or high satisfaction with the content of the speakers’ presentations (90% participants) and with their responses to questions posed by participants (95% of participants). Satisfaction with meeting similar others was rated as moderate or high by 88% of participants. Satisfaction that the forum increased HD knowledge was rated as moderate to high by 57% of participants. The relevance of the presentation to their individual needs was reported as moderate or high by 87% of participants.
Regarding logistical aspects of the forum, the majority of participants (80%) indicated support for the 1.5-hour length of the forum, with a minority (16%) of those attending the first two ‘in-person’ forums commenting that they would have preferred a longer time allocation for the small group discussion. There was overall endorsement for conducting the forums after business hours to allow participants to attend after work. The venue of the SPNDS for the first two forums was generally supported, although a minority of participants indicated that the distance from their home was a disincentive. The videoconference format of the final forum was identified as beneficial for many, due to the convenience of not needing to travel to attend. Participants from rural or regional Victoria noted that they were only able to attend the final forum due to its availability via videoconference. Some participants stated that they missed the opportunity for ‘in-person’ interactions in the third forum. In the final forum, participants were asked to indicate their preference for forum delivery format, and two-thirds stated a preference for the videoconference over the in-person format. In addition to travel, some other barriers to attendance were identified, including securing child-minding and anxiety about meeting others with pre-symptomatic HD for the first time.
A wide range of topics were suggested by participants for future forums including peer support, support for partners, strategies for disclosing about HD with friends, risks of disclosure at work, family planning and reproductive technologies, HD treatments, how meditation might help, diet and gut health, how to delay onset, how to prepare for becoming symptomatic, couple relationship issues, caregiving for HD relatives, discussing HD with children, dispelling myths about HD, how to identify early symptoms and creating ways of connecting with other pre-symptomatic people (e.g. Facebook groups, camps).
The text responses from the Forum Feedback Questionnaires and the transcribed audio recordings of small group discussions were collated and classified into two general categories: the first involved comments specific to the structure and content of the forums, and the second involved comments pertaining to participants’ experience of pre-symptomatic HD. Thematic analysis of these two categories of comments can be seen in Tables 1 and 2.
The themes shown in Table 1 were derived from participants’ comments about the structure and content of the forums. Themes included the forums’ positive, hopeful energy; the comfortable setting; the security of knowing that information was current and reliable, sourced from HD specialists and focussed singularly on their needs, as a pre-symptomatic group. Some comments pointed to confronting aspects of attending a forum.
Table 2 highlights themes that were significant to the lived experience of people with pre-symptomatic HD, derived from their questionnaire and discussion comments. These themes include their sense of isolation and stigma, their overwhelming gratification in meeting similar others, feeling able to discuss significant shared challenges and their adaptations and strategies for living with these challenges.
Discussion
In this two-phase consumer-focused research, information forums that met key areas of identified need were found to be strongly valued by people with pre-symptomatic HD. In phase 1, the information needs identified by those with pre-symptomatic HD related to how to prepare now for a future that is likely to be affected by HD (e.g. financial and legal preparation), factors that may delay or mitigate HD onset (e.g. pharmacological research, impact of physical activity) and strategies to deal with their current emotional challenges (e.g. managing fears, stigma, caring for HD family members). As in the study by Braisch et al. (2016), basic knowledge of the disease and predictive testing were not paramount. Participants may have felt sufficiently well-informed about these areas.
In phase 2, forums based on topics of greatest interest (identified in phase 1) were delivered. These forums attracted strong attendance and were positively evaluated in participant feedback data. The structure of the forums, the selection of speakers with specific HD professional or research experience, the actual content of the presentations and the quality of speakers’ responses to participant questions were all rated highly. Forum acceptability was increased by its familiar location, being timed in a way that minimised interference with participants’ work or family lives, and the availability of small group facilitated interactions with people who faced similar issues. Participants expressed great appreciation of the rare opportunity for sharing their experiences, their common HD challenges and strategies they used to deal with these issues. Indeed, this specificity of the forums to pre-symptomatic HD was frequently highlighted and valued in the written and audio-recorded responses.
The forum feedback in phase 2 provided an opportunity for participants to expand on the topics of interest already identified in phase 1. These ranged from more information about reproductive choices, to ways of improving physical and mental health factors that may impact HD onset or course (diet, alcohol and other drugs, stress management), assisted dying legislation, strategies for communication with family and significant others about HD, caregiving for HD relatives, ways to get support with maintaining intimate relationships, preparing for becoming symptomatic, identifying early symptoms and increasing peer support connections, including via social media. These topics align with, and further develop, the information and support needs identified in two other studies. Ho and Hocaoglu (2011) found a predominance of social (stigma, family), emotional (future anxiety) and legal issues were most significant to those in the pre-symptomatic stage of HD. Stigma and genetic discrimination in the domains of insurance, employment and relationships were pinpointed as a concern by 46% people at risk for HD in the large international RESPOND-HD study (Erwin et al. 2010). These extensive needs for support and information in a wide range of topics present worthy directions for future forums for people with pre-symptomatic HD.
Valuable insights into the lived experience of people with pre-symptomatic HD were revealed during the forums. Meeting similar others and sharing their lived experiences appeared to facilitate a normalising and supportive process. Participants spoke of a longstanding familial and social imperative to maintain secrecy about their gene-positive status, commonly associated with a sense of shame and stigma. The forums’ unique opportunities for disclosure in a safe space that was specific to their needs seemed to generate a powerful and welcome sense of connection and positive identification, facilitating a potential community antidote to broader societal stigma. They shared some of their on-going concerns, such as uncertainty about when and how symptoms will manifest, an anxious tendency to attribute normal cognitive or motor errors (such as forgetting or dropping something) to HD early symptoms, concerns about whether their children might be affected and a yearning for research to discover effective treatments. Great variability was seen in their emotional response to learning of their gene-positive status, ranging from devastation to relief (from previous uncertainty). Strategies for dealing with their shared concerns were also discussed by participants, including approaches to maintaining their emotional health, regular physical activity, use of online resources and preparing for future financial security. That these coping strategies were recommended by people with authentic lived experiences was likely to be quite compelling for participants. The range of significant psychological challenges and potential coping strategies described by participants with pre-symptomatic HD certainly warrants further research attention.
Participant descriptions of the sense of unity and hope generated within the forum discussion groups provide an initial indication of the potential for such interventions to have positive psychological effects. This contrasts with a pervasive belief that psychological symptoms associated with HD are solely biologically determined, even in pre-symptomatic stage (Theed et al. 2018). It is likely that this longstanding belief has been a disincentive to research exploring psychological interventions. A recent article by Zarotti et al. (2020) has challenged the belief. They have strongly encouraged both individual and group-based psychological intervention research into anxiety, depression, improving coping strategies and quality of life, especially amongst those who are pre-symptomatic. Future research is needed to explore whether regular access to the type of group-based information and support sessions described in this paper may have a positive impact on psychological problems associated with pre-symptomatic HD.
Another important aspect of this study to consider is the degree to which it was guided by consumer involvement. The identification of topics relevant to those with pre-symptomatic HD informed the intervention, and this consumer group provided feedback about their experience of the intervention. That 87% of participants regarded the forum intervention as closely aligned with their individual needs affirmed the value of consumer involvement in developing the project. Our approach adhered to the guidelines for consumer involvement in health research (NHMRC 2016). Consumer involvement is vital for increasing the relevance of research for pre-symptomatic HD consumers, as well as instilling greater confidence in and engagement with the resulting interventions. This project has provided consumer-generated recommendations for future topics and consumer feedback that can inform the structure and delivery of future forums. There are multiple opportunities for even more extensive consumer involvement to be developed, including more collaboration between people with pre-symptomatic HD and the research team in improving the design and running of future forums, in evaluating their efficacy and in disseminating the research results, possibly through social media that is developed by the consumer group.
In addition to increasing the input of consumers, the participants had suggestions for other improvements to the forums. A number of participants in the first two forums noted that they would have preferred more time in the small discussion groups. Some described anxiety about attending the forums. These individuals may require some extra targeted support to facilitate their well-being during forums. Participants recommended that accessing the forums via videoconference should be routinely offered, allowing the involvement of those who live at geographic distance or who have other care responsibilities. A comparison of the experience of in-person versus videoconference delivery of forums would be of future interest. Developing options for break-out discussion groups within videoconference forums may increase the possibility of peer support in that modality. Independent analysis of the experience of the pre-symptomatic individuals compared with their significant others would also be valuable. The study was restricted to those who were pre-symptomatic and aware of their gene status and did not include those who are at risk of developing HD but have not yet had predictive testing. This is an important group that also have unique needs for information and support and should not be overlooked. Understanding the reasons for not attending forums is also important: Are non-attenders fearful, disinterested, avoidant, unavailable or not see forums as relevant? What features distinguish those who attend information and support forums from those who do not? Finally, the present study drew on the experience of pre-symptomatic individuals who attended a single, large, government-funded clinic. Their experience may differ from those who attend, for instance, private-health practitioners, and as such, the results may be limited in their generalisability.
In summary, a consumer-driven research focus allowed the issues and information needs of greatest significance for pre-symptomatic HD to be addressed in a series of forums. This enabled a stigmatized and silenced group to discover a sense of community, shared concerns, helpful strategies and support and reduce their sense of isolation. They received up-to-date information that potentially empowered them with knowledge that is relevant to current and future decision-making and quality of life. Opportunities for this model to be developed should be encouraged, with many more key issues — already identified in this study — to be addressed to meet the needs of the pre-symptomatic HD group.
Data availability
The authors confirm that the non-patient-identifying raw data supporting the findings of this study are available from the corresponding author.
References
A’Campo L, Spliethoff-Kamminga N, Roos R (2012) The patient education program for Huntington’s disease (PEP-HD). J Huntingtons Dis 1(1):47–56. https://doi.org/10.3233/JHD-2012-120002
Australian Commission on Safety and Quality in Health Care (ACSQHC) (2017) Partnering with Consumers Standard. https://www.safetyandquality.gov.au/standards/nsqhs-standards/partnering-consumers-standard. Accessed 12 Aug 2021
Braisch U, Martinez-Horta S, MacDonald M, Orth M (2016) Important but not enough–information about HD related topics and peer and professional support for young adults from HD families. J Huntington’s Dis 5(4):379–387. https://doi.org/10.3233/JHD-160218
Centre for Genetics Education (CGE) (2017) Huntington’s disease and genetic testing. https://www.genetics.edu.au/publications-and-resources/booklets-and-pamphlets/huntington-disease-and-genetic-testing. Accessed 04 Sept 2021
Duff K, Paulsen JS, Beglinger LJ, Langbehn DR, Stout JC, Predict-HD Investigators of the Huntington Study Group (2007) Psychiatric symptoms in Huntington’s disease before diagnosis: the predict-HD study. Biol Psychiatry 62(12):1341–1346. https://doi.org/10.1016/j.biopsych.2006.11.034
Duff K, Beglinger LJ, Paulsen JS (2008) “Pre-symptomatic” Huntington’s disease. Handb Clin Neurol 89:589–598. https://doi.org/10.1016/S0072-9752(07)01255-9
Eccles F, Craufurd D, Smith A et al (2020) Pilot and Feasibility Studies 6(1):1–13. https://doi.org/10.1186/s40814-020-00631-z
Erwin C, Williams JK, Juhl AR, Mengeling M, Mills JA, Bombard Y, ... and I‐RESPOND‐HD Investigators of the Huntington Study Group (2010) Perception, experience, and response to genetic discrimination in Huntington disease: the international RESPOND‐HD study. Am. J. Med. Genet. B: Neuropsychiatric Genetics 153(5): 1081–1093. https://doi.org/10.1089/gtmb.2012.0288
Harrison JD, Auerbach AD, Anderson W et al (2019) Patient stakeholder engagement in research: a narrative review to describe foundational principles and best practice activities. Health Expect 22(3):307–316. https://doi.org/10.1111/hex.12873
Ho AK, Hocaoglu MB, European Huntington’s Disease Network Quality of Life Working Group (2011) Impact of Huntington’s across the entire disease spectrum: the phases and stages of disease from the patient perspective. Clin Genet 80(3):235–239. https://doi.org/10.1111/j.1399-0004.2011.01748.x
Honrath P, Dogan I, Wudarczyk O et al (2018) Risk factors of suicidal ideation in Huntington’s disease: literature review and data from Enroll-HD. J Neurol 265(11):2548–2561. https://doi.org/10.1007/s00415-018-9013-6
Myers RH (2004) Huntington’s disease genetics. NeuroRx 1(2):255–262. https://doi.org/10.1602/neurorx.1.2.255
National Health and Medical Research Council (NHMRC) (2016) Statement on Consumer and Community involvement in Health and Medical Research, Consumers Health Forum of Australia. https://www.nhmrc.gov.au/about-us/publications/statement-consumer-and-community-involvement-health-and-medical-research. Accessed 31 Aug 2021
Reiner A, Dragatsis I, Dietrich P (2011) Genetics and neuropathology of Huntington’s disease. Int Rev Neurobiol 98:325–372. https://doi.org/10.1016/B978-0-12-381328-2.00014-6
Smith JA (ed) (2003) Qualitative psychology: a practical guide to research methods. Sage Publications, Inc.
Stopford C, Ferrer-Duch M, Moldovan R, MacLeod R (2020) Improving follow up after predictive testing in Huntington’s disease: evaluating a genetic counselling narrative group session. J Community Genet 11(1):47–58. https://doi.org/10.1007/s12687-019-00416-9
Theed R, Eccles FJ, Simpson J (2018) Understandings of psychological difficulties in people with the Huntington’s disease gene and their expectations of psychological therapy. Psychol Psychother Theory Res Pract 91(2):216–231. https://doi.org/10.1111/papt.12157
Tilleras K, Kjoelaas S, Dramstad E et al (2020) Psychological reactions to predictive genetic testing for Huntington’s disease: a qualitative study. J Genet Couns 9(6):1093–1105. https://doi.org/10.1002/jgc4.1245
Timman R, Roos R, Maat-Kievit A, Tibben A (2004) Adverse effects of predictive testing for Huntington disease underestimated: long-term effects 7–10 years after the test. Health Psychol 23(2):189. https://psycnet.apa.org/doi/10.1037/0278-6133.23.2.189. Accessed 05 Sept 2021
Zarotti N, Dale M, Eccles F, Simpson J (2020) Psychological interventions for people with Huntington’s disease: a call to arms. J Huntington's Dis (Preprint) 1–13. https://doi.org/10.3233/JHD-200418
Acknowledgements
Nicholas Jackson and Roxanne Maule provided invaluable support with the logistics involved in conducting the forums. Dr. Fiona Fisher, Marie-Claire Davis and Dr Sarah Velissaris assisted with the preparation of the manuscript.
Funding
Prof Julie Stout of Monash University kindly provided funding for this project that enabled it to be conducted outside of business hours.
Author information
Authors and Affiliations
Contributions
The study’s conception and design involved Cathy Gluyas, Lisa Mottram and Rosie Gibb. Cathy Gluyas collated the data and completed the qualitative analysis. The first draft of the manuscript was written by Cathy Gluyas, and all the authors commented on subsequent versions of the manuscript. All the authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All work was conducted in accordance with the Declaration of Helsinki (1975). This research received ethics approval from the Calvary Health Care Bethlehem Ethics Committee (HREEC number 19041801).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gluyas, C., Mottram, L., Gibb, R. et al. Identification of psychoeducation needs and an intervention response for pre-symptomatic Huntington’s disease. J Community Genet 14, 175–183 (2023). https://doi.org/10.1007/s12687-022-00624-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-022-00624-w