Abstract
We previously reported that an accelerated decline in circulating testosterone level is associated with a higher risk of prostate cancer (PCa). This study is to examine whether testosterone change rate is related to serum prostate-specific antigen (PSA) concentration among PCa-free men. Longitudinal data were derived from electronic medical records at a tertiary hospital in the Southeastern USA. PCa-free men with initial-PSA < 4 ng/mL and ≥ 2 testosterone measurements were included (n = 632). Three PSA measures (peak, the most recent, and average PSA) during the study period (from first testosterone measurement to the most recent hospital visit) were examined using multivariable-adjusted geometric means and were compared across quintiles of testosterone change rate (ng/dL/month) and current testosterone level (cross-sectional). Mean (standard deviation, SD) age at baseline was 59.3 (10.5) years; mean study period was 93.0 (55.3) months. After adjusting for covariates including baseline testosterone, the three PSA measures all significantly increased across quintile of testosterone change rate from increase to decline (peak PSA: quint 1 = 1.09, quint 5 = 1.41; the most recent PSA: quint 1 = 0.85, quint 5 = 1.00; average PSA: quint 1 = 0.89, quint 5 = 1.02; all Ptrend < 0.001). But current testosterone level was not associated with PSA levels. Stratified analyses indicated men with higher adiposity (body mass index > 24.1 kg/m2) or lower baseline testosterone (≤ 296 ng/dL) were more sensitive to testosterone change in regard to PSA. Among PCa-free men, accelerated testosterone decline might correlate with higher serum PSA concentration. It will help to elucidate the mechanisms relating aging-accompanying testosterone dynamics to prostate carcinogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Testosterone is essential for prostate development during early life and maintains a tropic and differentiating effect throughout childhood and adult life [1]. A normal level of testosterone is important to maintain a high quality of life, including normal libido and sexual function, stable mood, muscle mass and strength, normal bone mineral density, and fat metabolism [2]. However, testosterone level declines progressively with aging, resulting in a significant percentage (20–39%) of men aged > 45 years have a testosterone level below the normal range for adult men (280–800 ng/dL) recommended by the American Association of Clinical Endocrinologist (AACE) [3, 4]. Therefore, there is a growing awareness to compensate the aging-accompanying testosterone decline through endogenous (e.g., physical activity) and/or exogenous mechanisms (e.g., testosterone replacement therapy).
A major concern for enhanced testosterone level is its association with the risk of prostate cancer (PCa). Despite numerous studies have been reported over the past several decades [5,6,7,8,9], the relationship between testosterone and PCa risk remains controversial. One possible explanation for this long-lasting controversy is that most of the previous studies on this relationship were based on testosterone level measured at a cross-sectional time point, lacking a dynamic perspective. Therefore, a dynamic theory stating that it is the aging-accompanying dynamics in testosterone level, rather than cross-sectional testosterone levels that impact PCa risk has been proposed [10] and was supported in one of our recent reports [11]. In that study, an annual testosterone decline of ≥ 30 ng/dL (vs. < 30 ng/dL) in men was associated with more than 5-fold increase in PCa risk. Another study by Xu et al. [12] reporting that a younger age at which circulating testosterone declines to be below 350 ng/dL was associated with a higher PCa risk also supported this dynamic theory.
Though prostate-specific antigen (PSA)-based screening for PCa is not recommended by the latest US Preventive Services Task Force (USPSTF) guideline [13], PSA level is still one important consideration in the decision-making of prostate biopsy and estimation of prognosis [14,15,16]. Given testosterone decline rate has been suggested to be associated with PCa risk [10,11,12], whether it is also related to serum PSA in PCa-free men is unknown. Addressing this question is of great significance in elucidating the mechanistic role of testosterone dynamics in prostate carcinogenesis and improving the prediction of prostate cancer.
In the current study, we applied a longitudinal design and examined the association of testosterone change rate with serum PSA among PCa-free men, using data derived from the electronic medical records at a tertiary hospital in the Southeastern USA. As part of our analytical strategy, testosterone measured at cross-sectional time points was also analyzed.
Materials and Methods
Study Population and Sample
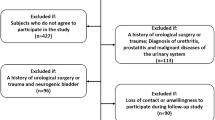
This study targeted PCa-free men with initial PSA < 4 ng/mL. The study sample was nested in a hospital-based retrospective observational cohort consisting of men with at least one record of circulating testosterone test at a tertiary care hospital in the Southeastern USA. For any man having one or more records of total testosterone measurement in the electronic medical records (EMR) system, all of his medical records (up to the most recent hospital visit) were reviewed. The reviewed medical records included outpatient visits and hospitalizations. A unique de-identified patient ID was used to link the data of demographics, medical diagnoses, lab results, drug prescription, and other clinical information. In the current study, we included patients (1) without history of PCa diagnosis throughout all hospital visits, (2) having two or more testosterone measurements with at least 1 month apart (for measuring testosterone change over time), (3) serum PSA level < 4 ng/mL at the first PSA measurement during the study period (for exclusion of any undiagnosed PCa cases), and (4) without history of testosterone replacement therapy (TRT). For eligible participants, date of his first testosterone measurement served as baseline, and study period was defined to be the time interval from baseline to the most recent hospital visit. A total of 632 participants with a mean (standard deviation, SD) study period of 93.0 (55.3) months were included in this study, after exclusion of 25 patients with baseline PSA ≥ 4 ng/mL, 285 with 1 testosterone measurement or > 1 testosterone measurement but within 1 month, 35 with history of TRT, and 45 with PCa diagnosis. The included medical records ranged from January 1995 to October 2015.
This study has been performed in accordance with the Declaration of Helsinki. The research protocol was approved by the institutional review board at the University of Florida.
Circulating Testosterone Change Rate
The exposure of interest was the change rate in circulating total testosterone level. We calculated average change per month in testosterone level (ng/dL/month) as proxy of testosterone change rate. This variable was created in two ways depending on the number of data points. For participants with only two testosterone measurements, average change in testosterone per month was calculated by firstly subtracting baseline testosterone level from the second testosterone measurement, then dividing the difference by time interval (months) between the two measurements. For participants with more than two testosterone measurements, we firstly regressed testosterone level to time interval (months) between that testosterone measurement and baseline, then took the beta regression coefficient (slope) as the testosterone change rate (ng/dL/month) for that participant. For this variable, positive values indicated testosterone increase, while negative values indicated testosterone decline. During the study period, a mean (SD) of 4.3 (3.5) testosterone measurements had be conducted.
In addition to testosterone change rate, baseline testosterone level (analyzed as a covariate) and current testosterone level (the most recently measured testosterone level) were included as proxy of cross-sectional testosterone measures. Number of testosterone measurements and time interval over these measurements were also included as covariates in the modeling analysis to control for potential confounding effect.
Serum PSA Level
The outcome of interest was serum total PSA level. We analyzed PSA level in 3 measures: peak PSA, the most recent PSA, and average PSA over the study period. The PSA levels were log-transformed to account for skewed distribution and analyzed as continuous variables. During the study period, a mean (SD) of 4.8 (3.5) PSA measurements had be conducted. Likewise, number of PSA measurements and time interval over these measurements, as well as time interval between the first PSA measurement and baseline were also included as covariates in the modeling analysis to control for potential confounding effect.
Covariates
A number of other variables with potential to confound the association between testosterone and PSA were also assessed. These variables included age (years), race (White, Black, other), smoking status (current smoker, former smoker, never smoke), body mass index (BMI) (< 25, 25 to < 30, ≥ 30 kg/m2), family history of PCa (yes/no), and diabetes diagnosis (yes/no).
Statistical Analysis
Characteristics of the study sample were assessed using descriptive statistical methods, including mean, SD, and proportions. Wald chi-square test for proportions and one-way ANOVA for means were used to compare differences across quintile of baseline testosterone level. We also estimated Ptrend for continuous variables using Wald F-tests by modeling median value of baseline testosterone level by quintile.
We then estimated crude and multivariable-adjusted geometric means of the three PSA measures (peak, the most recent, and average) and 95% confidence intervals (CI) across quintile of testosterone change rate. Multivariable-adjusted geometric means were estimated using the predicted margins from linear regression models controlling for covariates as shown in Table 1, as well as baseline testosterone level in the models of testosterone change rate. We evaluated the trend in geometric mean PSA levels across testosterone change rate by modeling natural log-transformed PSA level and testosterone change rate as a single ordinal variable. Each participant was assigned the median value within his quintile, and the statistical significance was evaluated using Student’s t test. As an analytical strategy, we also analyzed the relationships of current testosterone level as a proxy of cross-sectional testosterone measure with the three PSA measures.
Additionally, stratified analyses were conducted by race (White, Black) in dummy variables, adiposity (low: BMI at or below the median of 24.10 kg/m2; high: BMI > 24.10 kg/m2), age (young: at or below the median of 64 years; old: > 64 years), and baseline testosterone level (low: at or below the median of 295.75 ng/dL; high: > 295.75 ng/dL). Interactions were tested by including the main effect of testosterone change rate, the stratification factor, along with a product term of the two, the coefficient for which was evaluated by Wald test.
All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC). P values < 0.05 (two-sided) were reported as statistically significant.
Results
Characteristics of the Study Sample
Characteristics of the 632 men are presented in Table 1, overall and by quintile of baseline testosterone level. At baseline, the participants had a mean (SD) age of 59.3 (10.5) years; 75.0% were White; almost half of them (46.1%) were current or former smokers; 47.3% had a BMI < 25 kg/m2; 3.2% had a family history of PCa; 13.1% had a history of diabetes. Mean (SD) PSA at the first PSA measurement was 1.1 (0.8) ng/mL, with a mean (SD) time interval of 12.3 (23.1) months between baseline and the first PSA measurement.
Association of Cross-Sectional Testosterone Level with PSA
Table 2 presents the crude and multivariable-adjusted geometric means of peak PSA, the most recent PSA, and average PSA by quintiles of current testosterone level. After controlling for covariates, current testosterone level was positively but marginally associated with the most recently measured PSA (Ptrend = 0.049), whereas was not associated with peak PSA (Ptrend = 0.965) or average PSA (Ptrend = 0.502).
Association of Testosterone Change Rate with PSA
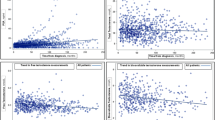
Table 3 presents the crude and multivariable-adjusted geometric means of the three PSA measures by quintile of testosterone change rate from increase to decline. After adjusting for covariates including baseline testosterone level, the three PSA measures all significantly increased across quintile of testosterone change rate (increase to decline) (peak PSA: quint 1 = 1.09, quint 5 = 1.41, Ptrend < 0.001; the most recent PSA: quint 1 = 0.85, quint 5 = 1.00, Ptrend < 0.001; average PSA: quint 1 = 0.89, quint 5 = 1.02, Ptrend < 0.001) (Fig. 1). Given the similar patterns of the three PSA measures, we focused on peak PSA in stratified analyses.
Stratified Analysis
Multivariable-adjusted geometric mean of peak PSA by testosterone change rate (ng/dL/month) stratified by race, adiposity, age, and baseline testosterone level is shown in Table 3. The association between testosterone change rate and peak PSA level was significant for the White (Ptrend < 0.001), but not for the Black (Ptrend = 0.520); marginally significant for participants with high adiposity (BMI > 24.10 kg/m2) (Ptrend = 0.059), but not for those with low adiposity (≤ 24.10 kg/m2) (Ptrend = 0.298); significant for participants with low baseline testosterone level (≤ 295.75 ng/dL) (Ptrend < 0.001), but not for those with high baseline testosterone level (> 295.75 ng/dL) (Ptrend = 0.305); and significant for both the young (≤ 59 years) (Ptrend < 0.001) and the old (> 59 years) (Ptrend < 0.001).
Discussion
Expression of the PSA gene has been extensively studied as a model androgen-regulated gene [17, 18], but the association of circulating testosterone level with serum PSA is still ill defined. Most of the reported studies investigating this association have been conducted using simultaneously measured testosterone and PSA at cross-sectional time point [7,8,9, 19]. But using cross-sectional design to study the association of testosterone with PSA is limited considering the substantial aging-accompanying changes in testosterone level [20, 21]. In recent years, there has been a growing interest in studying the longitudinal profile of testosterone change in relation to the prostate health [10,11,12, 22,23,24]. In the current study among PCa-free men with initial-PSA < 4 ng/mL, we found evidence that an accelerated testosterone decline was associated with higher serum PSA level (Table 4).
Indirect evidence for the influence of circulating androgen on PSA comes from the observation that men receiving androgen deprivation therapy for PCa experience a decline in serum PSA level [9]. However, evidence for the association of testosterone to PSA among cancer-free men has been limited. A cross-sectional study based on the National Health and Nutrition Examination Survey (NHANES) reported that among men without history of PCa, serum total testosterone was positively associated with serum PSA [9]. However, a pooled analysis of 18 prospective epidemiological studies on hormones and PCa found that, among controls, total testosterone and PSA were not correlated (7143 men, r = 0.08, P > 0.05) [25]. In our current analysis of testosterone and PSA, we also found that the concurrently measured testosterone and PSA were not associated; however, we found testosterone decline rate was positively associated with PSA level. To our knowledge, this is the first study reporting the association between circulating testosterone change rate and serum PSA level. This finding is in line with our previous finding that an accelerated testosterone decline was associated with a higher PCa risk [11].
Circulating testosterone level in males has been demonstrated to fall substantially with aging, particularly after the age of 40 [26], and a dramatic decline in circulating testosterone level has been suggested to increase the expression of AR [22]. PSA, a single-chain 33-kD glycoprotein serine protease, is synthesized almost exclusively by the prostate epithelium in human [17], and the expression of PSA gene is positively regulated by AR [17]. Given these, an increased AR expression might mediate the association between an accelerated testosterone decline and upregulated PSA expression [27]. In addition, our finding is also in line with human study on finasteride, which has been demonstrated to have a marked inhibitive effect on PSA expression [28] as well as to reduce the age-related testosterone decline [29]. It is highly possible that the finasteride-induced slowdown in aging-accompanying testosterone decline is one of the mechanisms in the finasteride-PSA relationship. But more studies are needed to replicate this finding and elucidate pertinent mechanisms.
Stratified analyses suggest some potential modifiers of the association between testosterone change rate and PSA. In race-stratified analysis, the association was significant (Ptrend < 0.001) only among White men. But considering the small sample size in the stratum of Black males, further study is needed to replicate this finding. A significant association (Ptrend < 0.001) was observed in both young and old men, suggesting the positive association between testosterone decline rate and PSA might persist for a long time during lifetime. Also, the association was significant only in high-adipose men but not in the low-adipose, significant only in hypogonadal men but not in eugonadal men. Given low testosterone level is widely reported to be associated with increased fat mass [30], the two findings are mutually verified and suggest that obese and/or hypogonadal men might be more sensitive to testosterone decline in regard to the prostate health.
There are several strengths and limitations in our study. First, the data were extracted from medical records, thereby avoiding the probability of recall bias. Second, to our knowledge, this is the first study exploring the association of testosterone change rate with serum PSA. Also, results of this study were robust because we simultaneously analyzed cross-sectional level and longitudinal change in circulating testosterone, and comprehensively analyzed three PSA measures as outcomes. However, our study has several limitations. First, we used linear regression in calculating testosterone change rate, but obviously testosterone change is hard to be linear under the impact of lifestyle factors. But due to the limitation of electronic medical records data, we were only able to adjust for BMI but not for other lifestyle factors impacting testosterone level. Thus, bias cannot be ruled out without a more rigorously designed study. Second, the study sample was from patients with two or more testosterone measurements, which may not be random. Though we have limited the included patients to be PCa-free throughout the entire study period and have baseline PSA of < 4 ng/mL to improve their comparability with the general population, caution is still needed in generalizing our study conclusion. Third, in the current study, even though the increase in circulating PSA level was statistically significant based on P values, the level increase between the lowest and highest quintiles was marginal, e.g., from 1.09 (95% CI, 1.03–1.14) to 1.41 (95% CI, 1.34–1.49). More studies are needed to further explore the biological significance and clinical relevance of such a marginal PSA increase.
Despite these limitations, the current study, for the first time, reports that an accelerated decline in circulating testosterone level was associated with a higher serum PSA, and men with high adiposity and/or low baseline testosterone level might be more sensitive to this association. It will help to elucidate the mechanisms relating the aging-accompanying testosterone dynamics to risk of prostate carcinogenesis.
References
Isaacs JT. Testosterone and the prostate. Testosterone: action, deficiency, substitution 2004;3:347–74
Wang C, Cunningham G, Dobs A, Iranmanesh A, Matsumoto AM, Snyder PJ et al (2004) Long-term testosterone gel (AndroGel) treatment maintains beneficial effects on sexual function and mood, lean and fat mass, and bone mineral density in hypogonadal men. J Clin Endocrinol Metab 89(5):2085–2098
Araujo AB, Esche GR, Kupelian V, O'Donnell AB, Travison TG, Williams RE et al (2007) Prevalence of symptomatic androgen deficiency in men. J Clin Endocrinol Metab 92(11):4241–4247
Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, O'Neill TW et al (2008) Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab 93(7):2737–2745
Schenk JM, Till C, Hsing AW, Stanczyk FZ, Gong Z, Neuhouser ML et al (2016) Serum androgens and prostate cancer risk: results from the placebo arm of the Prostate Cancer Prevention Trial. Cancer Causes Control 27(2):175–182
Klap J, Schmid M, Loughlin KR (2015) The relationship between total testosterone levels and prostate cancer: a review of the continuing controversy. J Urol 193(2):403–413
Mustafa M, Horuz R, Celik M, Kucukcan A (2014) Is there an association between serum prostate-specific antigen values and serum testosterone levels in healthy men? Korean J Urol 55(7):465–468
Boyle P, Koechlin A, Bota M, d'Onofrio A, Zaridze DG, Perrin P et al (2016) Endogenous and exogenous testosterone and the risk of prostate cancer and increased prostate-specific antigen (PSA) level: a meta-analysis. BJU Int 118(5):731–741
Peskoe SB, Joshu CE, Rohrmann S, McGlynn KA, Nyante SJ, Bradwin G et al (2015) Circulating total testosterone and PSA concentrations in a nationally representative sample of men without a diagnosis of prostate cancer. Prostate 75(11):1167–1176
Xu X, Chen X, Hu H, Dailey AB, Taylor BD (2015) Current opinion on the role of testosterone in the development of prostate cancer: a dynamic model. BMC Cancer 15(806):015–1833
Wang K, Chen X, Bird VY, Gerke TA, Manini TM, Prosperi M (2017) Association between age-related reductions in testosterone and risk of prostate cancer-an analysis of patients’ data with prostatic diseases. Int J Cancer 141(9):1783–1793
Xu X, Zhang X, Zhong Y, Saad F, Perez-Patron MJ, Haider K et al (2018) Dynamic patterns of testosterone levels in individuals and risk of prostate cancer among hypogonadal men: a longitudinal study. J Urol 199(2):465–473
Grossman DC, Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB, Davidson KW et al (2018) Screening for prostate cancer: US Preventive Services Task Force recommendation statement. Jama 319(18):1901–1913
An H, Tao N, Li J, Guan Y, Wang W, Wang Y et al (2016) Detection of prostate cancer metastasis by whole body magnetic resonance imaging combined with bone scintigraphy and PSA levels. Cell Physiol Biochem 40(5):1052–1062
Tomioka A, Tanaka N, Yoshikawa M, Miyake M, Anai S, Chihara Y et al (2014) Nadir PSA level and time to nadir PSA are prognostic factors in patients with metastatic prostate cancer. BMC Urol 14(33):1471–2490
Verma A, St Onge J, Dhillon K, Chorneyko A (2014) PSA density improves prediction of prostate cancer. Can J Urol 21(3):7312–7321
Balk SP, Ko YJ, Bubley GJ (2003) Biology of prostate-specific antigen. J Clin Oncol 21(2):383–391
Yousef GM, Obiezu CV, Luo LY, Black MH, Diamandis EP (1999) Prostase/KLK-L1 is a new member of the human kallikrein gene family, is expressed in prostate and breast tissues, and is hormonally regulated. Cancer Res 59(17):4252–4256
Botelho F, Pina F, Figueiredo L, Cruz F, Lunet N (2012) Does baseline total testosterone improve the yielding of prostate cancer screening? Eur J Cancer 48(11):1657–1663
Hu H, Odedina FT, Reams RR, Lissaker CT, Xu X (2015) Racial differences in age-related variations of testosterone levels among US males: potential implications for prostate cancer and personalized medication. J Racial Ethn Health Disparities 2(1):69–76
Feldman HA, Longcope C, Derby CA, Johannes CB, Araujo AB, Coviello AD et al (2002) Age trends in the level of serum testosterone and other hormones in middle-aged men: longitudinal results from the Massachusetts male aging study. J Clin Endocrinol Metab 87(2):589–598
Zhou Y, Otto-Duessel M, He M, Markel S, Synold T, Jones JO (2013) Low systemic testosterone levels induce androgen maintenance in benign rat prostate tissue. J Mol Endocrinol 51(1):143–153
Zhou Y, Bolton EC, Jones JO (2015) Androgens and androgen receptor signaling in prostate tumorigenesis. J Mol Endocrinol 54(1):14–0203
Wang K, Chen X, Gerke TA, Bird VY, Ghayee HK, Prosperi M (2018) BMI trajectories and risk of overall and grade-specific prostate cancer: an observational cohort study among men seen for prostatic conditions. Cancer Med 7(10):5272–5280. https://doi.org/10.1002/cam4.1747
Roddam AW, Allen NE, Appleby P, Key TJ (2008) Endogenous sex hormones and prostate cancer: a collaborative analysis of 18 prospective studies. J Natl Cancer Inst 100(3):170–183
Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD et al (2010) Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med 363(2):123–135
Kerr JE, Allore RJ, Beck SG, Handa RJ (1995) Distribution and hormonal regulation of androgen receptor (AR) and AR messenger ribonucleic acid in the rat hippocampus. Endocrinology 136(8):3213–3221
Wang LG, Liu XM, Kreis W, Budman DR (1997) Down-regulation of prostate-specific antigen expression by finasteride through inhibition of complex formation between androgen receptor and steroid receptor-binding consensus in the promoter of the PSA gene in LNCaP cells. Cancer Res 57(4):714–719
Roehrborn CG, Lee M, Meehan A, Waldstreicher J (2003) Effects of finasteride on serum testosterone and body mass index in men with benign prostatic hyperplasia. Urology 62(5):894–899
Klaassen Z, Howard LE, Moreira DM, Andriole GL Jr, Terris MK, Freedland SJ (2017) Association of obesity-related hemodilution of prostate-specific antigen, dihydrotestosterone, and testosterone. Prostate 77(5):466–470
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, K., Chen, X., Cheng, TY.D. et al. Association of Long-Term Dynamics in Circulating Testosterone with Serum PSA in Prostate Cancer-Free Men with Initial-PSA < 4 ng/mL. HORM CANC 10, 168–176 (2019). https://doi.org/10.1007/s12672-019-00369-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-019-00369-y