Abstract
Studies show decreased risk of breast cancer recurrence and improved survival with statin use, but data on racial disparities regarding breast cancer prognosis and statin use are lacking. Our objective was to investigate if racial disparities in breast cancer prognosis can be partially explained by differences in pre-diagnosis statin use. Patients were identified from a prospective, multicenter study examining the effects of metabolic factors on breast cancer prognosis in Black and White women. Statin use, prognosis (as measured by Nottingham Prognostic Index), anthropometric, tumor, and socio-demographic characteristics were examined. Five hundred eighty-seven women (487 White, 100 Black) with newly diagnosed primary invasive breast cancer were recruited. Obesity was more prevalent in Black women than White women (47 vs 19%, p < 0.01); both groups had similar low-density lipoprotein (LDL) cholesterol levels (113 ± 41 vs 113 ± 36 mg/dl, p = 0.90). More Black women used statins than White women (18 vs 11%, p = 0.06). Black women had a worse prognosis in an adjusted model than White women (OR 2.13 95% CI 1.23–3.67). Statin use was not associated with prognosis in unadjusted (OR 1.03, 95% CI 0.53–2.0) and adjusted models (OR 1.14, 95% CI 0.56–2.31). In women with newly diagnosed breast cancer, Black women were more likely to be treated with statins than White women, contrary to previous studies. Black women had worse prognosis than White women, but this difference was not explained by differences in pre-diagnosis statin use. Our study suggests that differences in pre-diagnosis statin use do not contribute to racial disparities in breast cancer prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While breast cancer mortality is improving overall, the disparity in breast cancer mortality between Black and White women is increasing [1]. Black women are more likely than White women to have breast cancer with poor prognostic features [2]. This disparity cannot be completely explained by differences in established risk factors for breast cancer mortality [2]. Additionally, Black women have higher rates of obesity, insulin resistance, and dyslipidemia when compared with White women [3, 4]. Dyslipidemia has been associated with increased cancer risk [5].
Statins (a class of lipid-lowering drugs) are used by approximately one fourth of women over the age of 40 in the USA [6]. Pre-clinical studies have demonstrated that statins have an anti-proliferative effect on breast tumor cells [7,8,9]. Furthermore, five large retrospective cohort studies (which included different types of statins—both lipophilic and hydrophilic) have shown reduced risk of breast cancer recurrence [10,11,12,13,14]. In regard to mortality, some investigations have shown that statin use in women with breast cancer has been associated with improved survival [15,16,17], while others have shown no significant survival benefit [18,19,20].
In patients with hypercholesterolemia and coronary artery disease, Black patients are less likely than White patients to use statins [21, 22]. Among patients eligible for cholesterol treatment according to the 2013 American College of Cardiology and the American Heart Association (ACC/AHA) guidelines, Black patients were less likely to take cholesterol-lowering medications than White patients [23]. Barriers to taking cholesterol-lowering medications and statins include fewer doctors’ visits, decreased awareness of high cholesterol, and decreased adherence [23, 24].
As statins have an association with decreased breast cancer recurrence, as well as potentially improved survival, disparities in statin use between Black and White women with breast cancer are important to investigate. Our objective was to elucidate whether or not statin use differs between Black and White women with breast cancer and if racial disparities in breast cancer prognosis can be partially explained by differences in pre-diagnosis statin use.
Materials and Methods
Study Population
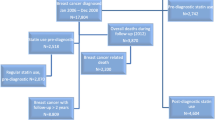
We prospectively identified 587 women (487 White, 100 Black) with newly diagnosed primary invasive breast cancer. Participants were recruited from multiple medical centers in New York, New Jersey, and Baltimore at the time of their breast cancer surgery. Data were collected primarily for a study investigating the role of insulin resistance in breast cancer prognosis in Black and White Women (National Cancer Institute (NCI) grant 1R01CA171558-01) [25]. Participants were enrolled between March 2013 and March 2017 and recruitment was still ongoing for the insulin resistance study.
Eligibility criteria included age over 21 years and women self-identifying as White or Black. Hispanic Black women were also included, but Hispanic White were excluded since this group is more likely to have estrogen receptor (ER)-/progesterone receptor (PR)-negative tumors than non-Hispanic White women, which might influence the association between race and hormone receptor status. This sample excluded women with diabetes treated with oral or injected glucose-lowering therapies, as these conditions influence insulin levels, one of the primary endpoints of the main study.
Data Collection
Eligible patients were identified and consented prior to breast cancer surgery. Participants were surveyed regarding socio-demographic characteristics, medical comorbidities, menstrual history, behavioral characteristics, including physical activity, diet, and access to care. Access to care was measured by screening mammography less than 2 years prior to breast cancer diagnosis [26]. Comorbidities were measured via the Charlson Comorbidity Index [27]. Patients were also surveyed about medication use and were categorized as statin users or not statin users. Anthropometric data, including blood pressure, weight, height, waist circumference, were recorded at the initial study visit, or within 1 month of surgery. Fasting lipids, including total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides (TGs), were collected at the time of surgery. Fasting glucose was also collected at the time of surgery. Metabolic syndrome was determined for women using waist circumference, fasting glucose, triglycerides, HDL cholesterol, and blood pressure according to the American Heart Association and National Heart, Lung, and Blood Institute guidelines [28]. Additionally, final pathology reports containing ER, PR, human epidermal growth factor receptor 2 (HER2) status, lymph node status, tumor size, and tumor grade were obtained. The pathology data (tumor size, number of positive nodes, and histology grade) were used to calculate the Nottingham Prognostic Index (NPI). NPI was used rather than tumor stage for prognosis, as NPI is less influenced by health care access than stage and has been validated in multiple countries [29,30,31]. A study that dichotomized NPI at 4.4 showed significant differences in biomarkers between the good and poor prognosis groups [32], and thus, participants were dichotomized into two categories: better prognosis (NPI ≤ 4.4) and worse prognosis (NPI > 4.4). Eligibility for statin use was measured according to the 2013 American College of Cardiology/American Heart Association (ACC/AHA) and Adult Treatment Panel III (ATP III) guidelines [33, 34]. Both guidelines were included, as patient data collection started in March 2013 spanning the time when the 2013 ACC/AHA guidelines were published. The study was in accordance with the ethical standards of all institutions’ institutional review boards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statistical Analysis
Descriptive analyses were conducted for all baseline characteristics and statin use, including proportions, means and medians, and variability (standard deviations and ranges). Baseline patient characteristics, eligibility for statin use, and statin use if eligible were compared using the chi-square test for categorical variables and t test for continuous variables by race.
Multiple logistic regression analysis was used to predict worse prognosis while controlling for potential confounders. Univariate logistic regression analysis was used to determine association between individual variables and worse prognosis. The multivariate models included covariates associated with tumor prognosis, as well as covariates shown in the literature to be strong confounders.
Results
Sociodemographic, behavioral, and health characteristics compared by race are shown in Table 1. Black and White women were similar in age (58.6 ± 13 vs 58.2 ± 12, p = 0.78) and proportionally similar in post-menopausal status (46.5 vs 49.3%, p = 0.60). In regard to socio-demographics, fewer Black women than White women had an income ≥ $50,000 (58.5 vs 80%, p < 0.01), but were similar in regard to education (education ≥ college) (59 vs 64%, p = 0.31). No statistically significant difference in smoking prevalence was found between Black and White women (15.6 vs 7.1%, p = 0.10). More Black women had a mammogram within 2 years of breast cancer diagnosis (81.6 vs 76.3%, p = 0.03). Furthermore, more Black women had blood pressure ≥ 140/90 mmHg (71 vs 45%, p < 0.01), had a body mass index (BMI) ≥ 30 kg/m2 (47 vs 19%, p < 0.01), had a larger waist circumference (107.8 ± 15 cm vs 94.3 ± 13 cm, p < 0.01), and a higher proportion had the metabolic syndrome (40.0 vs 19.7%, p < 0.01) when compared with White women. More Black women had lower HDL (61 ± 16 vs 69 ± 19 mg/dL, p < 0.01), lower TGs (86 ± 37 vs 100 ± 91 mg/dL, p = 0.03), and more triple-negative (ER, PR, HER2 negative) breast cancer (14 vs 7%, p = 0.02) when compared with White women. Similar LDL levels (113 ± 41 vs 113 ± 36 mg/dL, p = 0.90) were found in both groups. In regard to tumor stage, differences between Black and White women were not statistically significant (stage I 55.0 vs 64.3%, stage II 41.0 vs 32.7%, stage III 4.0 vs 3.1%), p = 0.22.
A comparison of statin use and eligibility in Black and White women is shown in Table 2. In our sample, more Black women used statins than White women (18 vs 11%; p = 0.06), but this difference was not statistically significant. Similar proportions of Black women and White women were eligible for statin therapy according to ATP III and 2013 ACC/AHA guidelines (11.0 vs 9.2%, p = 0.60 and 40.7 vs 33.8%, p = 0.21, respectively). In general, more women were eligible for statin therapy with the 2013 ACC/AHA criteria compared with ATP III criteria. For women eligible for statin therapy (according to ATP III and 2013 ACC/AHA guidelines), there was no statistically significant difference in statin use between Black and White women (30.0 vs 23.8%, p = 0.70 for ATPIII and 27.0 vs 24.0%, p = 0.70 for 2013 ACC/AHA guidelines).
Based on their NPI scores, 17% of the women had worse prognosis breast cancer (NPI > 4.4). More Black women than White women had worse prognosis breast cancer (27 vs 15%, p = 0.009) (Table 1). Unadjusted and adjusted analyses of the association of statin use, race, and other variables with prognosis are shown in Table 3. Statin use was not associated with prognosis in unadjusted (OR 1.03, 95% CI 0.53–2.0) or adjusted (OR 1.14, 95% CI 0.56–2.31) models. Black race was associated with poor prognosis in the multivariate model (OR 2.13 95% CI 1.23–3.67) adjusting for age, LDL, menopausal status, metabolic syndrome, and mammography ≤ 2 years before breast cancer diagnosis (a measure of access to care).
Discussion
In this study of women with primary invasive breast cancer, a higher proportion of Black women used statins than White women and statin use was not associated with breast cancer prognosis. We also found that Black race was associated with worse breast cancer prognosis. To our knowledge, this study is the first to investigate racial disparities in statin use and its relationship with breast cancer prognosis.
In our investigation, we observed that a higher proportion of Black women used statins than White women, though this difference was not statistically significant. In regard to dyslipidemia, our study found similar LDL levels in Black and White women and lower HDL and TGs in Black women than White women, which is consistent with prior population-based studies [3, 4]. Additionally, we found that there was no significant racial difference in treatment eligibility for statin use. There was also no racial difference in statin use if eligible according to ATP III and ACC/AHA guidelines. Our findings contrast with prior population studies that reported that Black patients with coronary artery disease and high cholesterol were less likely to take statins than White patients [21, 22]. Our results also contrast with a study that showed that treatment eligibility for lipid-lowering drugs was similar in White and Black patients, yet Black patients were less likely to take lipid-lowering drugs even when eligible [23]. Our study population includes only women diagnosed with breast cancer and perhaps reflects a patient cohort who is more engaged with the health care system and more likely to be prescribed medications as indicated than other cohorts. Our study also excludes women being medically treated for diabetes, which excludes many women in the population who would be treated with statins and might explain the lower rate of statin use in our patient population when compared with the general population. Interestingly, in studies investigating statin use and breast cancer outcomes that included race data, only one showed decreased post-diagnosis statin use in Black women compared with White women, while two other studies reported similar rates of statin use in both groups [10, 12, 17].
Pre-clinical studies have strongly demonstrated that statins have an anti-proliferative effect on breast cancer cells [7,8,9], but epidemiologic studies examining statins and breast cancer outcomes have had inconsistent results. Our finding that statin use is not associated with breast cancer prognosis is consistent with several previous investigations that did not demonstrate a significant relationship between statin use and breast cancer mortality [18, 19] and recurrence. [10, 13, 14] However, there are several studies that have found that both pre- and post-diagnosis statin use improves breast cancer recurrence rates [11, 12], as well as mortality [15,16,17]. These studies did not investigate if outcomes differed by race.
In our study, Black women had worse prognosis than White women in a non-adjusted model and a model that adjusted for metabolic syndrome, LDL, menopausal status, breast cancer screening patterns, and triple-negative breast cancer. The difference in prognosis could not be explained by differences in statin use. This is consistent with previous studies showing that Black women are more likely to present initially with breast cancer with aggressive features and have worse breast cancer prognosis [2, 35]. Black women were more likely than White women to have the metabolic syndrome, poor diet, lower HDL, higher number of comorbidities, and triple-negative disease, which could have a multifactorial impact on breast cancer prognosis [5, 36, 37].
Our analysis has several limitations. Some major limitations are the cross-sectional nature of our data analysis and that determination of statin use was based upon self-reported medication lists. Data regarding statin treatment duration and treatment were not collected, so we were not able to analyze any dose-dependent effects. Additionally, our population size and the proportion of recruited Black women were too small to assess the differences between lipophilic and hydrophilic statins.
In summary, in a population of women with newly diagnosed breast cancer, our study shows that Black women have a worse prognosis than White women, which could not be explained by differences in statin use. Black women were more likely than White women to be obese, have metabolic syndrome, and low HDL cholesterol, yet few studies have specifically investigated how these differences are associated with racial disparities in breast cancer outcomes. Further studies with larger populations and longer follow-up should investigate the differential effects of dyslipidemia and statin use on breast cancer tumor characteristics, prognostic features, and outcomes in Black and White women.
References
Hunt BR, Whitman S, Hurlbert MS (2014) Increasing Black:White disparities in breast cancer mortality in the 50 largest cities in the United States. Cancer Epidemiol 38(2):118–123. https://doi.org/10.1016/j.canep.2013.09.009
Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA (2015) Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA 313(2):165–173. https://doi.org/10.1001/jama.2014.17322
Liu J, Coady S, Carr JJ, Hoffmann U, Taylor HA, Fox CS (2014) Differential associations of abdominal visceral, subcutaneous adipose tissue with cardiometabolic risk factors between African and European Americans. Obesity (Silver Spring) 22(3):811–818. https://doi.org/10.1002/oby.20307
Frank AT, Zhao B, Jose PO, Azar KM, Fortmann SP, Palaniappan LP (2014) Racial/ethnic differences in dyslipidemia patterns. Circulation 129(5):570–579. https://doi.org/10.1161/circulationaha.113.005757
Mainous AG 3rd, Wells BJ, Koopman RJ, Everett CJ, Gill JM (2005) Iron, lipids, and risk of cancer in the Framingham Offspring cohort. Am J Epidemiol 161(12):1115–1122. https://doi.org/10.1093/aje/kwi131
Gu Q, Paulose-Ram R, Burt VL, Kit BK (2014) Prescription cholesterol-lowering medication use in adults aged 40 and over: United States, 2003-2012. NCHS Data Brief 177:1–8
Ghosh-Choudhury N, Mandal CC, Ghosh-Choudhury N, Ghosh Choudhury G (2010) Simvastatin induces depression of PTEN expression via NFkappaB to inhibit breast cancer cell growth. Cell Signal 22(5):749–758. https://doi.org/10.1016/j.cellsig.2009.12.010
Campbell MJ, Esserman LJ, Zhou Y, Shoemaker M, Lobo M, Borman E, Baehner F, Kumar AS, Adduci K, Marx C, Petricoin EF, Liotta LA, Winters M, Benz S, Benz CC (2006) Breast cancer growth prevention by statins. Cancer Res 66(17):8707–8714. https://doi.org/10.1158/0008-5472.can-05-4061
Park YH, Jung HH, Ahn JS, Im YH (2013) Statin induces inhibition of triple negative breast cancer (TNBC) cells via PI3K pathway. Biochem Biophys Res Commun 439(2):275–279. https://doi.org/10.1016/j.bbrc.2013.08.043
Kwan ML, Habel LA, Flick ED, Quesenberry CP, Caan B (2008) Post-diagnosis statin use and breast cancer recurrence in a prospective cohort study of early stage breast cancer survivors. Breast Cancer Res Treat 109(3):573–579. https://doi.org/10.1007/s10549-007-9683-8
Ahern TP, Pedersen L, Tarp M, Cronin-Fenton DP, Garne JP, Silliman RA, Sorensen HT, Lash TL (2011) Statin prescriptions and breast cancer recurrence risk: a Danish nationwide prospective cohort study. J Natl Cancer Inst 103(19):1461–1468. https://doi.org/10.1093/jnci/djr291
Chae YK, Valsecchi ME, Kim J, Bianchi AL, Khemasuwan D, Desai A, Tester W (2011) Reduced risk of breast cancer recurrence in patients using ACE inhibitors, ARBs, and/or statins. Cancer Investig 29(9):585–593. https://doi.org/10.3109/07357907.2011.616252
Nickels S, Vrieling A, Seibold P, Heinz J, Obi N, Flesch-Janys D, Chang-Claude J (2013) Mortality and recurrence risk in relation to the use of lipid-lowering drugs in a prospective breast cancer patient cohort. PLoS One 8(9):e75088. https://doi.org/10.1371/journal.pone.0075088
Boudreau DM, Yu O, Chubak J, Wirtz HS, Bowles EJ, Fujii M, Buist DS (2014) Comparative safety of cardiovascular medication use and breast cancer outcomes among women with early stage breast cancer. Breast Cancer Res Treat 144(2):405–416. https://doi.org/10.1007/s10549-014-2870-5
Murtola TJ, Visvanathan K, Artama M, Vainio H, Pukkala E (2014) Statin use and breast cancer survival: a nationwide cohort study from Finland. PLoS One 9(10):e110231. https://doi.org/10.1371/journal.pone.0110231
Cardwell CR, Hicks BM, Hughes C, Murray LJ (2015) Statin use after diagnosis of breast cancer and survival: a population-based cohort study. Epidemiology 26(1):68–78. https://doi.org/10.1097/ede.0000000000000189
Brewer TM, Masuda H, Liu DD, Shen Y, Liu P, Iwamoto T, Kai K, Barnett CM, Woodward WA, Reuben JM, Yang P, Hortobagyi GN, Ueno NT (2013) Statin use in primary inflammatory breast cancer: a cohort study. Br J Cancer 109(2):318–324. https://doi.org/10.1038/bjc.2013.342
Desai P, Lehman A, Chlebowski RT, Kwan ML, Arun M, Manson JE, Lavasani S, Wasswertheil-Smoller S, Sarto GE, LeBoff M, Cauley J, Cote M, Beebe-Dimmer J, Jay A, Simon MS (2015) Statins and breast cancer stage and mortality in the Women’s Health Initiative. Cancer Causes Control: CCC 26(4):529–539. https://doi.org/10.1007/s10552-015-0530-7
Mc Menamin UC, Murray LJ, Hughes CM, Cardwell CR (2016) Statin use and breast cancer survival: a nationwide cohort study in Scotland. BMC Cancer 16:600. https://doi.org/10.1186/s12885-016-2651-0
Smith A, Murphy L, Sharp L, O'Connor D, Gallagher WM, Bennett K, Barron TI (2016) De novo post-diagnosis statin use, breast cancer-specific and overall mortality in women with stage I-III breast cancer. Br J Cancer 115(5):592–598. https://doi.org/10.1038/bjc.2016.232
Johansen ME, Hefner JL, Foraker RE (2015) Antiplatelet and statin use in US patients with coronary artery disease categorized by race/ethnicity and gender, 2003 to 2012. Am J Cardiol 115(11):1507–1512. https://doi.org/10.1016/j.amjcard.2015.02.052
Lipworth L, Fazio S, Kabagambe EK, Munro HM, Nwazue VC, Tarone RE, McLaughlin JK, Blot WJ, Sampson UK (2014) A prospective study of statin use and mortality among 67,385 blacks and whites in the Southeastern United States. Clin Epidemiol 6:15–25. https://doi.org/10.2147/clep.s53492
Mercado C, DeSimone AK, Odom E, Gillespie C, Ayala C, Loustalot F (2015) Prevalence of cholesterol treatment eligibility and medication use among adults—United States, 2005–2012. MMWR Morb Mortal Wkly Rep 64(47):1305–1311. https://doi.org/10.15585/mmwr.mm6447a1
Lewey J, Shrank WH, Bowry AD, Kilabuk E, Brennan TA, Choudhry NK (2013) Gender and racial disparities in adherence to statin therapy: a meta-analysis. Am Heart J 165(5):665–678, 678.e661. https://doi.org/10.1016/j.ahj.2013.02.011
Gallagher EJ, LeRoith D, Franco R, Antoniou IM, Nayak A, Livaudais-Toman J, Bickell N (2016) Metabolic syndrome and pre-diabetes contribute to racial disparities in breast cancer outcomes: hypothesis and proposed pathways. Diabetes Metab Res Rev. https://doi.org/10.1002/dmrr.2795
Elewonibi B, Miranda PY (2017) Using mammograms to predict preventive health services behavior and mortality in women. Prev Med Rep 5:27–32. https://doi.org/10.1016/j.pmedr.2016.10.012
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Fernando C (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: executive summary. Crit Pathw Cardiol 4(4):198–203
Balslev I, Axelsson CK, Zedeler K, Rasmussen BB, Carstensen B, Mouridsen HT (1994) The Nottingham Prognostic Index applied to 9,149 patients from the studies of the Danish Breast Cancer Cooperative group (DBCG). Breast Cancer Res Treat 32(3):281–290
Bates T, Evans T, Lagord C, Monypenny I, Kearins O, Lawrence G (2014) A population based study of variations in operation rates for breast cancer, of comorbidity and prognosis at diagnosis: failure to operate for early breast cancer in older women. Eur J Surg Oncol 40(10):1230–1236. https://doi.org/10.1016/j.ejso.2014.06.001
Albergaria A, Ricardo S, Milanezi F, Carneiro V, Amendoeira I, Vieira D, Cameselle-Teijeiro J, Schmitt F (2011) Nottingham Prognostic Index in triple-negative breast cancer: a reliable prognostic tool? BMC Cancer 11:299. https://doi.org/10.1186/1471-2407-11-299
Parisi F, Gonzalez AM, Nadler Y, Camp RL, Rimm DL, Kluger HM, Kluger Y (2010) Benefits of biomarker selection and clinico-pathological covariate inclusion in breast cancer prognostic models. Breast Cancer Res: BCR 12(5):R66. https://doi.org/10.1186/bcr2633
Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report (2002) Circulation 106(25):3143–3421
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129(25 Suppl 2):S1–45. https://doi.org/10.1161/01.cir.0000437738.63853.7a
Chen L, Li CI (2015) Racial disparities in breast cancer diagnosis and treatment by hormone receptor and HER2 status. Cancer Epidemiol Biomark Prev 24(11):1666–1672. https://doi.org/10.1158/1055-9965.epi-15-0293
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 348(17):1625–1638. https://doi.org/10.1056/NEJMoa021423
Silber JH, Rosenbaum PR, Clark AS, Giantonio BJ, Ross RN, Teng Y, Wang M, Niknam BA, Ludwig JM, Wang W, Even-Shoshan O, Fox KR (2013) Characteristics associated with differences in survival among black and white women with breast cancer. JAMA 310(4):389–397. https://doi.org/10.1001/jama.2013.8272
Funding
This work was supported by the National Cancer Institute (NCI) grant 1R01CA171558-01 (authors NAB and DL), NCI grant K08CA190779, and Tisch Cancer Institute Young Scientist Cancer Research Award, as funded by the JJR Foundation (author EJG).
Author information
Authors and Affiliations
Contributions
Conception and design: A. Leiter, N.A. Bickell, D. Leroith, K. Fei, R. Franco, E.J. Gallagher
Development of methodology: A. Leiter, N.A. Bickell, D. Leroith, K. Fei, E.J. Gallagher
Acquisition of data: N.A. Bickell, A. Nayak, S. Feldman, N.B. Friedman, A. Estabrook, T.A. King
Analysis and interpretation of data: K. Fei, A. Leiter, N.A. Bickell, D. Leroith, E.J. Gallagher
Writing, review, and/or revision of the manuscript: A. Leiter, N.A. Bickell, D. Leroith, A. Nayak, S. Feldman, N.B. Friedman, T.A King, K. Fei, R. Franco, E.J. Gallagher
Administrative, technical, or material support: R. Franco
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Leiter, A., Bickell, N.A., LeRoith, D. et al. Statin Use and Breast Cancer Prognosis in Black and White Women. HORM CANC 9, 55–61 (2018). https://doi.org/10.1007/s12672-017-0312-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-017-0312-7