Abstract
The aim of this study was to analyze the impact of metabolic syndrome (MetS) on outcome of patients with localized renal cell carcinoma (RCC). A retrospective database was compiled consisting of 646 patients who underwent surgery for localized RCC between 2005 and 2014. A total of 439 patients were eligible for final analysis. For diagnosis of MetS, the WHO criteria of 1998 were used. Median follow-up was 32 months (ranging from 2 to 119). Kaplan-Meier and log-rank analyses were performed to compare patients with and without MetS or its components. Univariate and multivariate logistic regression identified prognostic factors for progression-free survival (PFS), cancer-specific survival (CSS), and overall survival (OS). In our cohort, 9.8% (n = 43) of patients were diagnosed with MetS. There were no differences between patients with and without MetS regarding clinicopathological parameters with the exception of patients’ age (p = 0.002). Kaplan-Meier and log-rank analyses revealed a shorter PFS for patients with MetS (p = 0.018), whereas no differences were found for each of the single components of MetS, namely, diabetes mellitus (DM) (p = 0.332), BMI >30 kg/m2 (p = 0.753), hypertension (p = 0.451), and hypertriglyceridemia (p = 0.891). Logistic regression identified age (HR = 1.92, p = 0.03), tumor stage (HR = 4.37, p < 0.001), grading (HR = 4.57, p < 0.001), nodal status (HR = 3.73, p = 0.04), surgical margin (HR = 1.96, p = 0.04), concomitant sarcomatoid differentiation (HR = 5.06, p < 0.001), and MetS (HR = 1.98, p = 0.04) as independent factors for PFS. For CSS, only age (HR = 2.62, p = 0.035), tumor stage (HR = 3.06, p < 0.02), and grading (HR = 6.83, p < 0.001) were significant. In conclusion, patients with localized RCC and MetS show significantly reduced PFS and might profit from specific consultation and follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) is the second most lethal of the urological cancers, with at least 62,700 new cases and more than 14,000 cancer-related deaths in the USA in 2016 [1]. Several verified risk factors for RCC have been identified, including smoking, obesity, and hypertension [2]. Thus, for primary prevention of RCC, the European Association of Urology (EAU) Guidelines on RCC recommend elimination of cigarette smoking and weight reduction [2]. As well as disease prevention, certain prognostic factors can help clinicians to decide on therapy and follow-up of RCC patients. Here, clinical prognostic factors, such as performance status and symptoms, have been included in prognostic systems and nomograms of localized disease [3, 4] and are used in clinical practice.
RCC has been linked to various metabolic alterations that go far beyond the mutation of the VHL gene in clear-cell RCC (ccRCC) [5, 6]. In addition, growing evidence suggests that metabolic syndrome (MetS)—a combination of impaired glucose tolerance, obesity, hypertension, and dyslipidemia—has a strong association with increased RCC risk [7]. Among others, hormonal changes including insulin, insulin-like growth factor (IGF), and leptin have been suggested as underlying mechanisms for this observation [8]. However, the impact of MetS on prognosis of RCC is less investigated and seems to be more complex. Diabetes mellitus (DM) [9] and hypertriglyceridemia [10] have been associated with worse progression-free survival (PFS) and/or cancer-specific survival (CSS)/OS, whereas obesity has been associated with improved RCC outcome [11]. Until now, to our knowledge, no study on the survival outcome of RCC patients with concomitant MetS exists.
Given the diversity of data on oncological outcome of RCC in the presence of various components of MetS and the lack of data on outcome of RCC in patients with the manifestation of MetS, the aim of our work was to assess the effects of MetS on RCC in a comprehensive cohort study.
Patients and Methods
Design and Patients
Clinical data of patients (n = 646) who underwent radical or partial nephrectomy for localized RCC at our institution between 2005 and 2014 were consecutively pooled in a retrospective database. Patients with synchronous bilateral disease (n = 12), previous metachronous RCC (n = 36), or a history of a malignant tumor diagnosis before RCC (n = 159) were excluded. Furthermore, patients were censored at the time of occurrence of a second malignancy or metachronous RCC. Finally, clinicopathological data from 439 patients were analyzed.
MetS was diagnosed according to the WHO criteria of 1998, which defines MetS as impaired glucose tolerance, impaired fasting glucose or DM and/or insulin resistance together with two or more additional components from hypertension (blood pressure ≥ 160/90 mmHg), raised plasma triglycerides (≥150 mg/dl) and/or low HDL cholesterol (<35 mg/dl for men, <39 mg/dl for women), central obesity (body mass index (BMI) >30 kg/m2 or waist-to-hip ratio >0.9 for males, >0.85 for females), and microalbuminuria [12]. Surgical specimens were evaluated by experienced genitourinary pathologists, according to the current classification of renal tumors [5, 13]. Tumor stage was readjusted to the TNM staging system of 2009 [14]. Preoperative staging of patients included abdominal computed tomography or magnetic resonance imaging, chest imaging, serum chemistry, and bone scans. Brain imaging was performed when indicated by symptoms. None of the patients received (neo)adjuvant therapy. In cases of recurrence and/or metastatic disease, surgical removal, administration of immunotherapy or targeted therapy was used as therapeutic approach. Cause of death was determined by the physician or by chart review. Before inclusion of parameters into the database, local ethics committee approval (No. 2014-811R-MA) was obtained.
Outcome Measurements and Statistical Analysis
Statistical analysis was performed with JMP 11.0 (SAS Institute, Cary, NC, USA). PFS (time to relapse, progression, or death from any cause, whichever occurred first), CSS (time to death due to cancer), and OS (time to death, irrespective of the cause) were the endpoints of the study. For comparison of patient and tumor characteristics of RCC patients with or without MetS or its components, t tests and two-sided exact Fisher tests were used. To illustrate CSS, Kaplan-Meier curves and univariate Cox models were computed. To investigate the role of MetS or its components as independent prognostic factors, we used multivariate Cox models, adjusting for age (<65 years vs. ≥65 years), sex, Fuhrman grade (G1–2 vs. G3–4), tumor stage (pT1–2 vs. pT3–4), nodal stage (pN0 vs. pN+), surgical margin (R0 vs. R+), histology (ccRCC vs. non-ccRCC), and concomitant sarcomatoid differentiation as nominal variables. In the logistic regression models, either the parameter MetS or one single component (hypertension, BMI >30 kg/m2, hypertriglyceridemia) was regarded. Finally, we checked for multicollinearity between the predictors by calculating the corresponding variance inflation factors and the respective condition number. A p value <0.05 was considered significant.
Results
Patient characteristics of the cohort are shown in Table 1. Median age was 63 years (range 27–88) and male gender was predominant (72.4%, n = 318). Radical and partial nephrectomy balanced each other as the surgical approach for RCC (46.2%, n = 203 and 53.1%, n = 233). Overall, 85 (19.4%) patients had a recurrence (n = 15) and/or metastasis (n = 79) during the follow-up period. Median time to progression was 13.5 months (range 0.5–96). At the time of analysis, 54 patients in the cohort had died and 53.8% (n = 29) of the deaths were cancer related. DM was identified in 74 (16.9%) patients. Altogether, MetS was diagnosed in 43 (9.8%) of the patients, mostly due to the presence of hypertension and a BMI >30 kg/m2 in addition to DM (n = 26, 5.9%). Only 5 patients had the combination of DM, hypertension, hypertriglyceridemia, and a BMI >30 kg/m2 (Table 1). The medical treatment details of the patients with MetS and DM are displayed in Table 2. An insulin-dependent impaired glucose tolerance was found in 8 (18.6%) and 16 (21.6%) patients, and oral antidiabetics were taken by 27 (62.6%) and 50 (67.6%) patients, respectively.
As shown in Table 3, patient and tumor characteristics did not differ between patients with and without MetS except for age. The proportion of patients ≥65 years was significantly higher in the group with MetS (65.1 vs. 40.4%, p = 0.002). In addition, patients were stratified by the MetS components DM, hypertension, high BMI, and dyslipidemia. Similar to patients with MetS, diabetic patients (68.9 vs. 40.3%, p = 0.001), and patients with hypertension (56.2 vs. 23.8%, p = 0.001) were significantly older (age ≥ 65 years). The proportion of male patients was significantly higher in patients with a BMI >30 kg/m2 (77.0 vs. 61.5%, p = 0.003). and the respective patients were more likely to have a clear-cell histology (79.8 vs. 67.7%, p = 0.016). In contrast, patients with hypertriglyceridemia had a reduction in the frequency of ccRCC (53.8 vs. 75.6%, p = 0.006) and a lower frequency of higher grading (G3-G4) (53.8 vs. 75.6%, p = 0.006).
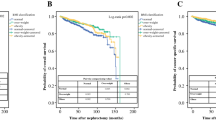
As displayed in Fig. 1a, Kaplan-Meier analysis showed a significantly decreased PFS in patients with MetS. Only 67.8% of the patients with MetS had no disease progression after 35 months compared to 83.1% of the patients without MetS (p = 0.018). No differences were observed when stratified for the various components of MetS individually (Fig. 1b–d). Kaplan-Meier analyses for CSS or OS showed no significant differences when stratified to MetS. However, OS was impaired in patients with DM (p = 0.021) and improved in patients with BMI >30 kg/m2 (p = 0.051) (Fig. S1 and S2).
To further assess factors involved in disease progression and survival, we performed uni- and multivariate analyses. As shown in Table 4, MetS was a significant factor in PFS using both uni- and multivariate regression (HR = 2.01, p = 0.032 and HR = 1.98, p = 0.047). Furthermore, independent factors for PFS were age (HR = 1.92, p = 0.031), tumor stage (HR = 4.37, p < 0.001), grading (HR = 4.57, p < 0.001), surgical margin (HR = 1.96, p = 0.042), nodal status (HR = 3.73, p = 0.038), and concomitant sarcomatoid differentiation (HR = 5.06, p = 0.002). In addition, we performed separate multivariate models including single components (DM, hypertension, high BMI, and hypertriglyceridemia) instead of MetS controlling for the same confounders. Here, no impact of the respective parameters on PFS was observed, although hypertriglyceridemia showed a tendency toward significance in multivariate analysis regarding PFS (HR = 2.84, p = 0.074). Respective analyses for CSS and OS are illustrated in Tables S1 and S2. Age (HR = 2.62, p = 0.035), tumor stage (HR = 3.06, p = 0.010), and grading (HR = 6.83, p < 0.001) were independent predictors of CSS, whereas only tumor stage (HR = 2.44, p = 0.016) and grading (HR = 4.36, p < 0.001) independently influenced OS. Finally, the variance inflation factors for all covariates were sufficiently small with a condition number of 5.4. Hence, any relevant collinearity effects can be ruled out.
Discussion
Our study demonstrates a significantly shorter PFS for RCC patients with MetS, whereas no differences in PFS were found for the single components of MetS when analyzed individually. To our knowledge, no study has yet analyzed the survival outcome of RCC patients who suffer from the complete spectrum of MetS factors. Whereas two previous studies described the association of MetS or its components with pathologic RCC features such as tumor size or grade [15, 16], the question of whether MetS itself influences the prognosis of RCC patients has not been resolved. In contrast, the single components of MetS have already been examined in relation to survival of RCC patients; in a recent meta-analysis, DM was associated with poor OS, CSS, and RFS [9]. However, several publications showed that the relation of DM and worse outcome was not significant, which is in accordance to our results [17–19]. Hypertension was shown to negatively affect cancer-specific and overall mortality in one study [20], whereas other studies revealed a non-significant coherence between hypertension and CSS/OS [21] or even a favorable outcome of RCC patients with a history of hypertension [22]. The only study on dyslipidemia showed that elevated serum triglycerides >250 mg/dl were independently associated with worse PFS [10]. Here, a trend toward significance regarding PFS was seen in our multivariate analysis (HR = 2.84, p = 0.074), with a cutoff of ≥150 mg/dl according to the WHO criteria of 1998 [12]. Interestingly, despite being one of the major risk factors for RCC development, numerous studies found obese RCC patients to have improved outcome compared to patients with normal weight [11, 23, 24]. No clear explanation has been brought forward for this paradox. However, some researchers question the “obesity paradox” hypothesis due to possible reverse causation, selection bias, or other forms of bias rather than being a true biological association [25, 26]. Regardless of these possible explanations, our study suggests that the obesity paradox does not implicitly apply and remains questionable especially in the context of the MetS.
Our study found a significant reduction in OS in patients with DM and improved OS in patients with BMI >30 kg/m2 in the Kaplan-Meier analyses in accordance to previous studies in patients with RCC [9, 11, 23]. However, in contrast to PFS, CSS and OS were not independently influenced by MetS in our study population. This can possibly be explained by the relatively short median follow-up of patients in our study and the limited number of events due to localized disease. Nevertheless, the reduced PFS in patients with MetS in combination with the lack of influence on PFS of the single components of MetS highlights the importance of including the complete picture of MetS in the assessment of RCC patients. Furthermore, this emphasizes the requirement to specially assign comprehensive therapy and follow-up for this patient population. Therapeutic options for patients with MetS in general include lifestyle modifications with diet, exercise, and behavioral therapy, optionally accompanied by a pharmacological approach (e.g. appetite suppressants, anti-diabetic agents, antihypertensive drugs, lipid lowering medications) and/or bariatric surgery [27, 28]. In other entities such as breast cancer, a positive effect of diet and weight loss has already been reported [29], and in diabetic RCC patients, cholesterol-lowering pharmacotherapy use was associated with a borderline significant RCC survival benefit [30]. Furthermore, bariatric surgery is associated with a significant reduction of cancer incidence and mortality and this cancer-protective role is strongest for female obesity-related tumors [31]. The question of whether therapeutic intervention for MetS can generate improved survival for RCC patients should be evaluated in randomized prospective trials.
Furthermore, our results emphasize the need for more investigation of the molecular mechanisms underlying our findings. This may not only increase our understanding about RCC biology but might also help to prevent its progression and identify possible targets of new cancer therapies. Various mechanisms have been put forward as explanation for the link between MetS and cancer progression. These include alterations in various hormone-regulated pathways such as insulin signaling or imbalances in the insulin-like growth factor (IGF) axis, and also altered adiponectin, leptin, and estrogen levels [8]. Since agents that modulate these respective hormonal signaling cascades are available, they should be considered as possible treatment strategies in patients with RCC and MetS. For example, in vitro experiments suggest that clinical application of anti-IGF antibodies may be effective in combination with mTOR inhibitors [32]. Besides endocrine disorders, the release of proinflammatory cytokines such as TNF-α or IL-6 by adipose tissue promotes angiogenesis and cell proliferation or hyperglycemia allowing fast tumor growth [8]. In RCC, the situation is even more complex. Its various biological features result in metabolic dysfunctions involving almost every metabolic pathway [6]. Many metabolic abnormalities of RCC can be linked to VHL loss, which causes alterations in pathways including glycolysis and oxidative phosphorylation [33]. Generally, a shift toward a Warburg-effect like state with dependency of anaerobic metabolism can be observed in RCC [34]. In addition, downregulation of AMP-activated kinase and increased acetyl CoA carboxylase is another frequent metabolic change causing increased fatty acid synthesis [35]. Hence, through metabolic reprogramming, RCC cells experience an anaerobic and thus less efficient catabolism with increased anabolism using alternative substrates. Therefore, tumor cells may extensively profit from the oversupply of metabolic substrates found in patients with MetS allowing faster disease progression. Consequently, a combined approach with cutting off the nutrient supply (by dietary or medical approaches e.g. metformin, bariatric surgery) and molecular inhibition of relevant metabolic pathways (e.g., mTOR inhibitors) should be the subject of prospective studies [36, 37]. In addition, targeting alternative sources of energy or lipogenesis may be promising and should be further investigated [38].
Our work is based on retrospective data with a relatively short median follow-up, which certainly has an impact on our findings regarding CSS and OS. However, our strict exclusion criteria provided a well-selected study cohort and reduced the risk of underlying biases. This work is to date the first study on outcome of localized RCC in the presence of MetS. Our results add to the understanding of RCC prognosis in this highly prevalent situation and will help to assign improved therapies and follow-up for RCC patients with concomitant MetS.
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66(1):7–30
Ljungberg B. Bensalah K, Bex A., Canfield S., Giles R.H., Hora M., Kuczyk M.A., Lam T., Merseburger A.S., Powles T., Staehler M., Volpe A.: members of the EAU Renal Cell Cancer Guidelines Panel. Guidelines Associates: Dabestani A., Fernández-Pello Montes S., Hofmann F., Marconi L., Tahbaz R. . EAU Renal Cell Cancer Guidelines. . In: Office EG, editor. EAU Guidelines 2016 ed. Arnhem, The Netherlands: EAU Guidelines Office 2016.
Patard JJ, Kim HL, Lam JS, Dorey FJ, Pantuck AJ, Zisman A et al (2004) Use of the University of California Los Angeles integrated staging system to predict survival in renal cell carcinoma: an international multicenter study. J Clin Oncol 22(16):3316–3322
Karakiewicz PI, Briganti A, Chun FK, Trinh QD, Perrotte P, Ficarra V et al (2007) Multi-institutional validation of a new renal cancer-specific survival nomogram. J Clin Oncol 25(11):1316–1322
Eble J, Sauter G, Epstein J, Sesterhenn I (2004) World Health Organization classification of tumors. Pathology and genetics of tumors of the urinary system and male genital organs. IARC Press, Lyon
Massari F, Ciccarese C, Santoni M, Brunelli M, Piva F, Modena A et al (2015) Metabolic alterations in renal cell carcinoma. Cancer Treat Rev 41(9):767–776
Zhang GM, Zhu Y, Ye DW (2014) Metabolic syndrome and renal cell carcinoma. World J Surg Oncol 12:236
Micucci C, Valli D, Matacchione G, Catalano A (2016) Current perspectives between metabolic syndrome and cancer. Oncotarget 7(25):38959–38972
Chen L, Li H, Gu L, Ma X, Li X, Gao Y et al (2015) The impact of diabetes mellitus on renal cell carcinoma prognosis: a meta-analysis of cohort studies. Medicine (Baltimore) 94(26):e1055
Haddad AQ, Jiang L, Cadeddu JA, Lotan Y, Gahan JC, Hynan LS et al (2015) Statin use and serum lipid levels are associated with survival outcomes after surgery for renal cell carcinoma. Urology 86(6):1146–1152
Choi Y, Park B, Jeong BC, Seo SI, Jeon SS, Choi HY et al (2013) Body mass index and survival in patients with renal cell carcinoma: a clinical-based cohort and meta-analysis. Int J Cancer 132(3):625–634
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15(7):539–553
Srigley JR, Delahunt B, Eble JN, Egevad L, Epstein JI, Grignon D et al (2013) The International Society of Urological Pathology (ISUP) Vancouver classification of renal neoplasia. Am J Surg Pathol 37(10):1469–1489
Edge SB, editor. AJCC cancer staging manual. 7th ed. ed. New York, NY [u.a.]: Springer; 2010.
Kocher NJ, Rjepaj C, Robyak H, Lehman E, Raman JD. Hypertension is the primary component of metabolic syndrome associated with pathologic features of kidney cancer. World J Urol. 2016.
Ozbek E, Otunctemur A, Sahin S, Dursun M, Besiroglu H, Koklu I et al (2013) Renal cell carcinoma is more aggressive in Turkish patients with the metabolic syndrome. Asian Pac J Cancer Prev 14(12):7351–7354
Nayan M, Finelli A, Jewett MA, Juurlink DN, Austin PC, Kulkarni GS, et al. Diabetes and kidney cancer outcomes: a propensity score analysis. Endocrine. 2016.
Hofner T, Zeier M, Hatiboglu G, Eisen C, Schonberg G, Hadaschik B et al (2014) The impact of type 2 diabetes on the outcome of localized renal cell carcinoma. World J Urol 32(6):1537–1542
Antonelli A, Arrighi N, Corti S, Zanotelli T, Cozzoli A, Cosciani Cunico S et al (2013) Pre-existing type-2 diabetes is not an adverse prognostic factor in patients with renal cell carcinoma: a single-center retrospective study. Urol Oncol 31(7):1310–1315
Park B, Jeong BC, Seo SI, Jeon SS, Choi HY, Lee HM (2013) Influence of body mass index, smoking, and blood pressure on survival of patients with surgically-treated, low stage renal cell carcinoma: a 14-year retrospective cohort study. J Korean Med Sci 28(2):227–236
Lee S, Hong SK, Kwak C, Kim HH, Lee SE (2012) Prognostic significance of diabetes mellitus in localized renal cell carcinoma. Jpn J Clin Oncol 42(4):318–324
Parker A, Freeman LB, Cantor K, Lynch C (2000) Self-report of smoking, obesity and hypertension history and survival among a cohort of Iowa renal cell carcinoma cases. Ann Epidemiol 10(7):467–468
Donin NM, Pantuck A, Klopfer P, Bevan P, Fall B, Said J et al (2016) Body mass index and survival in a prospective randomized trial of localized high-risk renal cell carcinoma. Cancer Epidemiol Biomark Prev 25(9):1326–1332
Ritch C, Lee DJ, Desai M, McKiernan JM (2009) Role of obesity and race in predicting recurrence rates and survival in renal cell carcinoma. J Clin Oncol 27(15_suppl):e16052
Wilson KM, Cho E (2016) Obesity and kidney cancer. Recent Results Cancer Res 208:81–93
Gupta S (2016) Obesity: the fat advantage. Nature 537(7620):S100–S102
Kaur J (2014) A comprehensive review on metabolic syndrome. Cardiol Res Pract 2014:943162
Lam DW, LeRoith D. Metabolic syndrome. In: De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, et al., editors. Endotext. South Dartmouth (MA) 2000.
Demark-Wahnefried W, Platz EA, Ligibel JA, Blair CK, Courneya KS, Meyerhardt JA et al (2012) The role of obesity in cancer survival and recurrence. Cancer Epidemiol Biomark Prev 21(8):1244–1259
Rabey JL, Yin J, Kublas TM, Mashtare T, Ceacareanu AC (2014) Management of comorbidities in diabetics with renal cell carcinoma: past utilization and current outcomes. J Pharm Pract 27(1):31–39
Ashrafian H, Ahmed K, Rowland SP, Patel VM, Gooderham NJ, Holmes E et al (2011) Metabolic surgery and cancer: protective effects of bariatric procedures. Cancer 117(9):1788–1799
Tracz AF, Szczylik C, Porta C, Czarnecka AM (2016) Insulin-like growth factor-1 signaling in renal cell carcinoma. BMC Cancer 16:453
Sudarshan S, Karam JA, Brugarolas J, Thompson RH, Uzzo R, Rini B et al (2013) Metabolism of kidney cancer: from the lab to clinical practice. Eur Urol 63(2):244–251
Cancer Genome Atlas Research N (2013) Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature 499(7456):43–49
Tong WH, Sourbier C, Kovtunovych G, Jeong SY, Vira M, Ghosh M et al (2011) The glycolytic shift in fumarate-hydratase-deficient kidney cancer lowers AMPK levels, increases anabolic propensities and lowers cellular iron levels. Cancer Cell 20(3):315–327
Psutka SP, Boorjian SA, Lohse CM, Stewart SB, Tollefson MK, Cheville JC et al (2015) The association between metformin use and oncologic outcomes among surgically treated diabetic patients with localized renal cell carcinoma. Urol Oncol 33(2):67 e15-23
Ciccarese C, Brunelli M, Montironi R, Fiorentino M, Iacovelli R, Heng D et al (2016) The prospect of precision therapy for renal cell carcinoma. Cancer Treat Rev 49:37–44
van der Mijn JC, Panka DJ, Geissler AK, Verheul HM, Mier JW (2016) Novel drugs that target the metabolic reprogramming in renal cell cancer. Cancer Metab 4:14
Acknowledgements
This study was supported in part by a grant from the Medical Faculty Mannheim, University of Heidelberg, Germany to N.W. (SabINe).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Electronic supplementary material
Figure S1
Kaplan-Meier curves for cancer specific survival probabilities stratified by metabolic syndrome (A) or its underlying components diabetes mellitus (B), high BMI (>30 kg/m2) (C), hypertension (D) or hypertriglyceridemia (>150 mg/dl) (E). (TIFF 14851 kb)
Figure S2
Kaplan-Meier curves for overall survival probabilities stratified by metabolic syndrome (A) or its underlying components diabetes mellitus (B), high BMI (>30 kg/m2) (C), hypertension (D) or hypertriglyceridemia (>150 mg/dl) (E). (TIFF 14718 kb)
ESM 3
(DOCX 13 kb)
ESM 4
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Kriegmair, M.C., Mandel, P., Porubsky, S. et al. Metabolic Syndrome Negatively Impacts the Outcome of Localized Renal Cell Carcinoma. HORM CANC 8, 127–134 (2017). https://doi.org/10.1007/s12672-017-0289-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-017-0289-2