Abstract
Prior reports identify higher serum concentrations of estrogens and androgens as risk factors for breast cancer, but steroids in nipple aspirate fluid (NAF) may be more related to risk. Incident breast cancer cases and mammography controls were recruited. Sex steroids were measured in NAF from the unaffected breasts of cases and one breast of controls. Menopausal status and menstrual cycle phase were determined. NAF steroids were purified by HPLC and quantified by immunoassays. Conditional logistic regression models were used to examine associations between NAF hormones and case-control status. NAF samples from 160 cases and 157 controls were evaluable for hormones. Except for progesterone and dehydroepiandrosterone (DHEA), the NAF and serum concentrations were not significantly correlated. NAF estradiol and estrone were not different between cases and controls. Higher NAF (but not serum) DHEA concentrations were associated with cases, particularly among estrogen receptor (ER)-positive cases (NAF odds ratio (OR) = 1.18, 95 % confidence interval (CI) 1.02, 1.36). NAF DHEA was highly correlated with NAF estradiol and estrone but not with androstenedione or testosterone. Higher progesterone concentrations in both NAF and serum were associated with a lower risk of ER-negative cancer (NAF OR = 0.69, 95 % CI 0.51, 0.92). However, this finding may be explained by case-control imbalance in the number of luteal phase subjects (2 cases and 19 controls). The significantly higher concentration of DHEA in NAF of cases and its correlation with NAF estradiol indicates a potentially important role of this steroid in breast cancer risk; however, the negative association of progesterone with risk is tentative.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of estradiol in the promotion of breast cancer is evidenced by the chemopreventive and therapeutic success of anti-estrogens and aromatase inhibitors [1, 2]. However, the association of serum estradiol with breast cancer risk [3] in postmenopausal women [4–6] and possibly in premenopausal women [7, 8] is relatively weak, perhaps because serum and tissue concentrations of estradiol are poorly correlated [9, 10]. For estradiol, several studies report correlations of 0.37 or less [11–13], although a higher correlation has been reported recently in BRCA1/2 carriers [14]. Overall, the results indicate that local formation of estradiol rather than simple diffusion from the blood is the primary source of estradiol in the breasts of both pre- and postmenopausal women. Androgens, which may serve as estrogen precursors or as risk factors themselves, have also been associated with a higher risk of breast cancer in both pre- and postmenopausal women [15–20], particularly in hormone receptor-positive breast cancer [18]. Estrogens can be synthesized in the breast from androgens of adrenal origin that diffuse into the breast [20] or from circulating estrogen sulfates [21] that are transported into the parenchymal tissue [22] and hydrolyzed by active sulfatase enzymes [11]. Regardless of whether hormones in nipple fluid represent local synthesis, or delivery through the circulation, the uniformity of nipple aspirate fluid (NAF) concentrations within individuals over time supports the contention that hormones in NAF are characteristic of individuals and should therefore be useful biomarkers of continued hormone exposure [23].
Despite the poor correlation between serum and NAF estradiol concentrations, the correlation between serum and NAF progesterone has been reported to be 0.70 and 0.69 in two previous studies [12, 24], suggesting that NAF progesterone may be significantly determined by uptake from serum. If factors within the breast microenvironment can indeed influence the amount of hormone available to breast cancer cells, then it is plausible that local hormone levels will show a stronger relation with cancer risk than circulating hormone levels. Since steroids are capable of diffusion across plasma membranes and the transfer into or out of cells is not dependent upon transport proteins [25], it is reasonable to assume that the concentration of the steroids in NAF is a reflection of the concentration in the tissue.
The contralateral unaffected breast of women with breast cancer is at increased risk for breast cancer [26, 27] and is a good model of the local breast environment that may influence breast cancer risk. NAF provides a relatively noninvasive sample of the breast environment and allows measurement of an important component of this environment, namely the steroid hormone content.
We obtained NAF samples from the contralateral breasts of breast cancer cases, and from screening mammography controls, using a case-control design with frequency matching for age, race, and menopause. We confirm previously observed patterns of steroids in NAF during the menstrual cycle and provide new information regarding the relationship of NAF hormones to breast cancer risk.
Methods
Subjects
Study participants were women with newly diagnosed unilateral breast cancer and screening mammography controls with normal mammograms and breast exams. There were 160 cases and 157 controls in the main study (2 premenopausal women did not have menstrual data, which were unavailable for this comparison). For this analysis, only women who provided NAF samples were included and women with current or past endocrine disorders or taking exogenous hormones were excluded. The study was conducted at the Lynn Sage Comprehensive Breast Center, under a protocol approved by the Northwestern Institutional Review Board. Consent was obtained from each patient after full explanation of the purpose and nature of all procedures used.
Data and Specimens
All subjects completed a health history questionnaire. In premenopausal subjects, the last menstrual period (LMP) and the next menstrual period (NMP) of the cycle in which NAF and blood were obtained were recorded. NAF collection was performed in a standard fashion; the breast was warmed and massaged, and a nipple aspirator was used to apply 10 cm3 of suction followed by manual stripping of the nipple. NAF was collected in calibrated capillary tubes (1 mm = 1 μl in volume) until no more could be expressed or more than 10 μl had been collected. The original study design stipulated luteal-phase NAF collection, but this quickly proved unfeasible in breast cancer patients who were trying to schedule their treatment procedures. NAF samples were therefore obtained at the subject’s convenience, and menstrual cycle phase was carefully assessed in the analyses. Menstrual cycle phase and menopausal status were confirmed post hoc based upon the following criteria: postmenopausal women reported no menstrual period within the last 12 months and had serum follicle-stimulating hormone (FSH) levels >30 mIU/ml, estradiol levels <30 pg/ml, and progesterone <3 ng/ml. The menstrual cycle was divided into three phases. Menstrual phase by dates was determined by counting back from the next menstrual period: in the follicular phase, days −20 through the first day of LMP; mid-cycle, days −19 through −12; and luteal phase, days −11 through 0. Menstrual phase assignment was confirmed based on serum hormone levels: follicular phase, serum estradiol concentrations <60 pg/ml and progesterone <3.0 ng/ml; mid-cycle, serum estradiol levels >60 pg/ml and progesterone <3.0 ng/ml; and luteal phase, estradiol levels >30 pg/ml and progesterone >3.0 ng/ml. Only cycles that met these criteria were considered in the analysis of menstrual phase and NAF hormones.
Laboratory Analyses
Estradiol was measured in serum by a radioimmunoassay from Beckman Coulter DSL-2700 from Brea, CA. Other analytes, measured by ELISAs from Beckman Coulter with catalog numbers, were the following: estrone, DSL-9700; androstenedione, DSL-3800; and dehydroepiandrosterone (DHEA) sulfate, DSL-2700; from Alpco FSH, 11-FSHHU-E01, and DHEA, 20-DHEHU-E01; and from Salimetrics, testosterone, 1-2402, and progesterone, 1-502-5. Aliquots from a pool of female control serum were inserted into each batch for quality control. The intra- and inter-assay percent coefficients of variation (%CVs) for the serum immunoassays were as follows: estradiol 10.4 and 17.2, FSH 7.2 and 7.6, progesterone 2.6 and 8.1, estrone 6.6 and 14.0, androstenedione 5.3 and 6.6, testosterone 10.5 and 16.4, and DHEA 8.7 and 10.2.
Steroid hormones in NAF were extracted with ethyl acetate/hexane (3:2), containing 250 ng of the internal standard, dexamethasone acetate. The extract was then applied to a 25 × 4.6 mm C18 reversed-phase high-performance liquid chromatography system and eluted with 58 % of 15 mmol/l phosphate buffer (pH 6) and 42 % of a 50:50 mixture of acetonitrile and methanol. A gradient was started at 40 min to a final concentration of 71 % of the second solvent at 50 min. The flow rate was 1.0 ml/min. Each fraction was collected for immunoassays in an automatic fraction collector as previously described in detail [24]. The accuracy, recovery, and precision have been described previously [24]. A preparation of breast cyst fluid (BCF), which is similar in content to NAF, was used as the quality control substance. This was frozen in small aliquots; aliquots were thawed, and one was placed along with a procedural blank between every set of 4 samples. Values were corrected for recovery of the internal standard. Estradiol was measured by a radioimmunoassay from Beckman Coulter, and the other steroids were measured by ELISAs, all after HPLC purification.
NAF samples were assayed in 16 batches; each batch contained an equal number of cases and controls, frequency matched for age, race, and menopausal status. Batches 10 through 15 were assayed by a different technician than 1 through 9 and failed largely because of high blank values. They have therefore been excluded from the analysis, leaving 317 subjects whose data are presented in this report. In the 317 evaluated NAF samples, the following numbers of samples yielded measurements in the detectable range for each hormone: 220 (69.4 %) for estradiol, 228 (71.9 %) for estrone, 230 (72.6 %) for testosterone, 225 (71.0 %) for androstenedione, 302 (95.3 %) for DHEA sulfate (DHEAS), 239 (75.4 %) for DHEA, and 287 (90.5 %) for progesterone. The intra- and inter-assay %CVs of the quality control samples were as follows: estradiol 5.2 and 5.2, estrone 4.4 and 6.7, testosterone 3.0 and 6.6, androstenedione 5.6 and 8.7, DHEA 10.3 and 13.1, and progesterone 11.0 and 13.2.
Statistical Analyses
Descriptive characteristics of study participants were summarized using means and standard deviations for continuous variables and counts and frequencies for categorical variables. These variables were compared for pre- and postmenopausal cases and controls using t tests and Fisher’s exact tests as appropriate.
The concentrations of the steroids were transformed to their natural logarithms to achieve adequate normality for parametric statistical analyses [12, 28]. Steroid concentrations not in the detectable range were omitted from analysis. Data were summarized as medians and interquartile ranges (IQRs) across all batches on their original scale. Analysis of covariance (ANCOVA) was used to evaluate hormone concentration differences by menopausal phase adjusted for batch. Partial correlation coefficients were calculated to evaluate correlations of NAF and serum hormone measurements after correction for batch.
Through visual inspection of box plots and examination of quality control measures, there was substantial inter-batch variability; therefore, conditional logistic regression models with strata defined by batch were used to examine associations between NAF hormones and case-control status. Separate models were analyzed for each hormone. Initially, associations were examined separately for pre- and postmenopausal women with adjustment for menstrual cycle phase (follicular, mid-cycle, luteal) for premenopausal women. Estimated effect sizes had consistent direction and similar magnitude for pre- and postmenopausal women, and so associations were reported using data from all women. In sensitivity analyses, adjustment for a four-category variable combining menstrual stage and phase (premenopausal follicular, premenopausal mid-cycle, premenopausal luteal, postmenopausal) was comparable to a simpler phase adjustment for pre- versus postmenopausal status and additional adjustment for body mass index (BMI) had little impact on estimated associations. Adjusted results are therefore reported using a simple pre/postmenopausal phase adjustment. Polytomous conditional logistic regression was also used to examine hormone associations of estrogen receptor (ER)-positive and ER-negative cases versus controls, including adjustment for menopausal status. To confirm results in parametric analyses, a nonparametric analysis was also employed. For each hormone, observed values were ranked within batch in ascending order. Within each batch, the average of the ranks were calculated for cases and controls and then divided by the average number of cases and controls in each batch to measure the proportion of the maximum possible difference in mean ranks for cases and controls observed within batch. An overall test statistic was then calculated as the mean of the batch-specific proportions. Statistical significance of this test statistic was determined by randomly reassigning case-control status within batch, preserving the number of cases and controls within batch, and then recalculating the test statistic. P values were reported as the proportion of 1000 permutations yielding test statistics as or more extreme than the observed test statistics for each hormone.
Results
Characteristics of the Study Population
A total of 156 premenopausal and 164 postmenopausal women (2 missing menopausal status) yielding ≥2 μl of NAF, assayed in batches 1–9, are included in the present analysis; their characteristics are shown in Table 1. Summary statistics showing they are similar to women with NAF in batches 10–16 are reported in Online Resource Table S1. The mean ages of the women who were included in this analysis were 46 years for those sampled in follicular phase (N = 41), 46 years for mid-cycle (N = 70), 46 years for luteal phase (N = 40), and 57 years for 164 postmenopausal women. The age range of premenopausal subjects in the study was 33 to 61 years, and that of postmenopausal subjects was 42 to 70 years.
For premenopausal women, cases were more frequently parous than controls (P = 0.04). In postmenopausal women, cases had a significantly higher BMI (31.1 vs. 28.0, P < 0.01) and higher age at menarche (12.7 vs. 12.2, P = 0.02) than controls. The mean volume of NAF did not vary significantly among groups (12.1 ± 12.5 μl in the follicular, 15.1 ± 19.1 μl in the mid-cycle, 20.2 ± 21.9 μl in the luteal phases, and 13.5 ± 15.8 μl in postmenopausal women), with a range of 2.0 to 126. However, in high yielders, collection of >10 μl depended on the subject’s willingness to continue. Sixty percent of subjects produced at least 2 μl of breast fluid (59 % of cases and 62 % of controls). The mean cycle sampling days for the premenopausal women (counting backwards from the date of the next period) were −26 in follicular phase, −14 in mid-cycle, and −9 in luteal phase.
Hormone Concentration in NAF and Serum
The patterns of hormones in concomitant serum and NAF samples throughout the menstrual cycle were assessed by ANCOVA, adjusted for batch. Confirming earlier work by this group of investigators [24, 25], the pattern of estradiol in NAF across the menstrual cycle in this larger study differs significantly from that in serum (Table 2). The lower concentrations of NAF estradiol at mid-cycle are not due to differences in volume of NAF or to NAF protein concentrations. While the mean concentration of NAF estradiol was lower after menopause, it was not significantly lower. This result was confirmed in fine-needle aspirates of the breast in a recent publication in which NAF estradiol was measured by mass spectrometry after HPLC purification [29]. In general, the concentrations of all steroids except progesterone were more uniform across menstrual and menopausal states in NAF than in serum.
The partial correlations between serum and NAF concentrations of estradiol, estrone, testosterone, and androstenedione (Table 3) were all <0.1. The correlation between serum and NAF DHEA was 0.20 (P = 0.003). As expected, the correlation of NAF progesterone with serum progesterone was high at 0.49 (P < 0.001). Correlations of steroids within NAF are shown in Table 4. Among the potential estradiol precursors, the highest correlation was of NAF DHEA with NAF estradiol (r = 0.21, P = 0.005). NAF androstenedione was correlated with NAF testosterone but neither of these C19 steroids was correlated with DHEA.
NAF Hormones and Case-Control Status
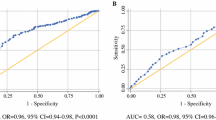
Our primary hypothesis is related to the estradiol content of NAF as an indicator of breast cancer risk, but we saw no significant association between NAF estradiol and case-control status (Table 5). However, higher DHEA content in NAF was significantly associated with breast cancer risk (P = 0.01). The higher NAF testosterone concentration for cases versus controls also approached significance. Conversely, NAF progesterone concentration was slightly lower in cases compared to controls after adjustment for menopausal status (P = 0.05) (Table 5). Analyses adjusted for menstrual phase showed similar results and are not shown. We then analyzed the data using nonparametric methods and observed similar results in terms of direction of association and statistical significance (Online Resource Table S2). Serum hormone levels after adjustment for menopausal status were not significantly associated with case/control status, except for a marginal negative association for progesterone (Table 6).
We performed polytomous logistic regression to examine potentially unique associations of NAF hormone content for ER-positive and ER-negative breast cancers. NAF DHEA demonstrated a stronger positive association with ER-positive than with ER-negative breast cancer (Table 7). NAF progesterone demonstrated an inverse association only with ER-negative cancer risk. No other statistically significant associations were found. The serum values are shown in Table 8. Estrogens were not associated with ER-positive or ER-negative cases. Serum DHEA was not associated with ER-positive or ER-negative cases versus controls, but serum progesterone, as in NAF, appeared to be negatively associated with ER-negative cancer. Adjustment for menstrual phase was not feasible for progesterone since there were 13 premenopausal ER-negative cases (4 in follicular, 7 in mid-cycle, and 2 in luteal phase).
Discussion
The importance of steroid hormone exposure to breast cancer etiology is clear but, so far, has only been studied in terms of systemic exposure, as reflected by reproductive history, circulating steroid concentrations, or exogenous use. The local breast environment has been relatively inaccessible, although a few small studies of breast tissue hormone concentrations have been published [9, 10, 29]. In this study, we focused on NAF as a suitable and available biosample of breast tissue hormone levels. Our previous work suggests that the breast estradiol exposure is locally regulated through endogenous synthesis within the breast [12] and that NAF estradiol is more stable over time than serum concentrations [23]. Based on that work, we hypothesized that NAF estradiol content may be a more robust indicator of breast cancer risk than serum estradiol. We performed a case-control study of NAF hormone concentrations in the at-risk but unaffected contralateral breast of incident breast cancer cases compared to screening mammography controls. We reasoned that the unaffected breast of women with unilateral breast cancer is a good high-risk model since the risk of future cancer is high (particularly in the absence of systemic therapy) and second cancers in this population have similar hormone receptor characteristics to the index cancer [30]. Additionally, the contralateral breast is not exposed to the local synthesis of hormones by the tumor [31, 32] or the inflammatory consequences of recent diagnostic biopsy. It is possible that tumor itself may have some effect on metabolism, although this appears unlikely [33, 34]. In earlier studies, we have observed that the hormonal environment of both breasts is similar; NAF estradiol, estrone sulfate, DHEA, androstenedione, and progesterone correlations between breasts were 0.61, 0.84, 0.65, 0.71, and 0.71, respectively [24].
We found that NAF estradiol was not related to breast cancer risk (odds ratio (OR) = 1.05, 95 % confidence interval (CI) 0.89–1.23), but there was a positive association between NAF DHEA and risk after adjustment for menopause (OR = 1.19, 95 % CI 1.04–1.37) for each unit increase in log DHEA concentration. In analyses of modeling ER+ and ER− breast cancer, this association remained statistically significant only for ER+ disease (OR = 1.18, 95 % CI 1.02, 1.36). NAF testosterone was not associated with risk in our study, although data on postmenopausal women from earlier studies suggest an association between serum testosterone and breast cancer risk [15–18]. Our results, in pre- and postmenopausal women, are consistent with the serum estradiol findings in premenopausal women from the large EPIC study [19] in which no association was found between prediagnostic serum concentrations of estradiol and breast cancer risk, even though a significant interquartile OR of 1.56 (95 % CI 1.15–2.13) was found in prediagnostic serum testosterone of premenopausal women. The relation of NAF progesterone with breast cancer risk was surprisingly inverse for all cases, with an OR of 0.84 (95 % CI 0.71–1.00), and particularly for ER-negative cases (OR = 0.69, 95 % CI 0.51, 0.92), but the significance of this is limited by the fact that there were only 13 ER-negative premenopausal cases with measureable NAF progesterone, of whom only 2 were in luteal phase. Among controls, on the other hand, 19 women were sampled in luteal phase.
We found no association of NAF estradiol with the serum estrogens, yet significant correlations were found between NAF estradiol and NAF DHEA. It is interesting that of the C19 potential precursors of estradiol in NAF, DHEA (which is abundant and therefore forms a large precursor pool) was highly significantly related to estradiol, but androstenedione and testosterone were not. The likely independent formation of NAF estrogens from NAF DHEA is suggested by the fact that NAF DHEA was not correlated with either androstenedione or testosterone. While DHEA cannot undergo aromatization [35], it appears that there is compartmentalization of the pathway from DHEA to estrogens in NAF such that the main pools of androstenedione and testosterone are not available for aromatization. This has been described for other steroid biosynthetic systems [37]. NAF DHEA was significantly related to serum DHEA, although the fraction accounted for was only 4 %. Evidence of 17β-hydroxysteroid dehydrogenase type 1 activity in the breast is indicated by the fact that androstenedione and DHEA were significant precursors of estradiol. NAF estrone sulfate has also been considered to be an important precursor of estrogens in the breast [36, 37] but was not measured in this study.
Our data, which are the first available data on NAF DHEA levels and risk, show positive associations for DHEA and breast cancer risk after adjustment for menopausal status, confirmed by a separate examination of these associations in pre- and postmenopausal women. However, previous studies of serum DHEA have shown mixed results, with a suggestion of differential effects across the menopause (promoting risk in postmenopausal women but offering protection in premenopausal women) [38]. In premenopausal women, Helzlsouer et al. [39] found lower mean serum DHEA in cases than in controls, with a relative risk of 0.4. Secreto and Zumoff [40] found similar trends in premenopausal subjects, but postmenopausal cases had higher levels than controls. However, in the Nurses’ Health Study [41], women with ER+/PR+ tumors and the highest quartile compared to the lowest quartile of serum DHEA demonstrated a relative risk of 1.6 (P (trend) = 0.09) and this was higher in premenopausal than postmenopausal women. Other studies of serum DHEA in postmenopausal women have found positive associations of DHEA and DHEAS with breast cancer risk, with a range of relative risk for DHEAS of 1.69 to 2.8 [15, 17, 18, 42], comparing the highest to lowest quartile. We did not observe an association between serum DHEA and risk, despite a significant correlation (r = 0.45) between NAF and serum DHEA concentrations.
Most studies have concluded that DHEA is active either by conversion to 5-androstene-3β,17β-diol, which has a moderate affinity for the estrogen receptor ,or after its conversion to estradiol [43, 44]. The importance of direct binding of 5-androstene-3β,17β-diol to the estrogen receptor has been demonstrated [45], and in one study, serum 5-androstene-3β,17β-diol was related to breast cancer risk, with a relative risk of 3.0 [42]. The fact that DHEA had a higher association with cancer risk than estradiol or other androgens is in keeping with Labrie’s concept of organ-specific conversion of DHEA to active products [44]; our findings of a relatively high correlation of NAF estradiol with NAF DHEA and other androgens (Table 4) are consistent with the conversion of DHEA to estrogens within the breast. Alternatively, DHEA may act through its own receptors, and specific DHEA receptors have been characterized in the liver [46] and T lymphocytes [47].
Surprisingly, we observed inverse associations of both NAF and serum progesterone with breast cancer risk overall, and these associations were stronger in women with ER− disease and remained significant after adjustment for menopausal status. This must be considered tentative, considering the small number of cases in luteal phase, although Haddad et al. [48] found that the SNP rs11571215 of the progesterone receptor was highly associated with ER− breast cancer. Alternatively, a possible explanation for our findings is that the metabolism of progesterone is different in high-risk breasts. Wiebe et al. [49] have shown that one metabolite of progesterone, 3α-hydroxy-4-pregnen-20-one (3αHP), suppresses proliferation and increases apoptosis in breast cancer cell lines while another metabolite, 5α-dihydroprogesterone (5αDHP), promotes the growth of mammary cancer. In addition, growth of xenografts of the ER-negative human breast cancer cell line MDA MB 231 was promoted by 5αDHP and suppressed by 3αHP in a mouse model [50], and recently, progesterone-dependent tumorigenesis of transplanted C4HD mouse mammary cells was shown to be inhibited by the 5α-reductase inhibitor finasteride but tumorigenesis by 5αDHP was unaffected [51]. This leads to the hypothesis that metabolism of progesterone to 5αDHP may be favored in the high-risk, contralateral breast, decreasing its remaining progesterone content. If this metabolite is retained in normal breast tissue as it is in breast tumor tissue [51], the result would be the promotion of breast cancer despite the lower measured progesterone concentrations. The human breast does have the necessary 5α-reductase, particularly the SRD5A2 isoform, to produce 5αDHP [52–54]. The predominant metabolic product of progesterone in the normal breast is 20α-dihydroprogesterone [55, 56], but 5αDHP predominates in breast tumors [56]. High-affinity, specific, membrane-bound receptors for 5αDHP have been described in ER-positive and ER-negative cell lines [57]. A clinical study also supports a role of 5αDHP; breast tumors expressing 5α-reductase by IHC were more aggressive, and the patients had shorter recurrence-free survival time [58]. Further work is justified to investigate the role of progesterone metabolism in the breast.
In summary, in this study, there was no association between NAF estradiol and breast cancer risk based on contralateral unaffected breasts of cancer cases versus controls, but we did observe a positive association of NAF DHEA with ER-positive cancer. The lack of association of serum DHEA with risk indicates a closer association of NAF than serum DHEA with breast cancer risk in individuals. Although estrogen levels were not significantly associated with cancer risk in our data, the high correlation of estrogens and androgens within the tissue provide evidence for greater availability of estrogen in the unaffected, high-risk breast. The negative association of NAF progesterone with ER-negative cancer after adjustment for menopausal status must be considered preliminary and may be explained by the small number of luteal-phase ER-negative cases.
References
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, Bevers TB, Fehrenbacher L, Pajon ER, Wade JL III et al (2010) Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 Trial: preventing breast cancer. Cancer Prev Res (Phila Pa) 3:OF1–OF11
Lonning PE (2011) The potency and clinical efficacy of aromatase inhibitors across the breast cancer continuum. Ann Oncol 22:503–514
Key TJ (1999) Serum oestradiol and breast cancer risk. Endocrine-Related Cancer 6:175–180 [Review] [40 refs]
Dorgan JF, Longcope C, Stephenson HE Jr, Falk RT, Miller R, Franz C, Kahle L, Campbell WS, Tangrea JA, Schatzkin A (1997) Serum sex hormone levels are related to breast cancer risk in postmenopausal women. Environ Health Perspect 105(Suppl 3):583–585
Cauley JA, Lucas FL, Kuller LH, Stone K, Browner W, Cummings SR (1999) Elevated serum estradiol and testosterone concentrations are associated with a high risk for breast cancer. Study of Osteoporotic Fractures Research Group. [comment]. Ann Int. Med 130, t-7
Berrino F, Pasanisi P, Bellati C, Venturelli E, Krogh V, Mastroianni A, Berselli E, Muti P, Secreto G (2005) Serum testosterone levels and breast cancer recurrence. Int J Cancer 113:499–502
Sturgeon SR, Potischman N, Malone KE, Dorgan JF, Daling J, Schairer C, Brinton LA (2004) Serum levels of sex hormones and breast cancer risk in premenopausal women: a case-control study (USA). Cancer Causes Control 15:45–53
Eliassen AH, Missmer SA, Tworoger SS, Spiegelman D, Barbieri RL, Dowsett M, Hankinson SE (2006) Endogenous steroid hormone concentrations and risk of breast cancer among premenopausal women. J Natl Cancer Inst 98:1406–1415
Thijssen JH, Blankenstein MA, Miller WR, Milewicz A (1987) Estrogens in tissues: uptake from the peripheral circulation or local production. Steroids 50:297–306
Geisler J (2003) Breast cancer tissue estrogens and their manipulation with aromatase inhibitors and inactivators. J Steroid Biochem Mol Biol 86:245–253
Chatterton RT Jr, Geiger AS, Gann PH, Khan SA (2003) Formation of estrone and estradiol from estrone sulfate by normal breast parenchymal tissue. J Steroid Biochem Mol Biol 86:159–166
Gann PH, Geiger AS, Helenowski IB, Vonesh EF, Chatterton RT (2006) Estrogen and progesterone levels in nipple aspirate fluid of healthy premenopausal women: relationship to steroid precursors and response proteins. Cancer Epidemiol Biomarkers Prev 15:39–44
Maskarinec G, Ollberding NJ, Conroy SM, Morimoto Y, Pagano IS, Franke AA, Gentzschein E, Stanczyk FZ (2011) Estrogen levels in nipple aspirate fluid and serum during a randomized soy trial. Cancer Epidemiol Biomarkers Prev 20:1815–1821
Loud JT, Gierach GL, Veenstra TD, Falk RT, Nichols K, Guttmann A, Xu X, Greene MH, Gail MH (2014) Circulating estrogens and estrogens within the breast among postmenopausal BRCA1/2 mutation carriers. Breast Cancer Res Treat 143:517–529
Kaaks R, Berrino F, Key T, Rinaldi S, Dossus L, Biessy C, Secreto G, Amiano P, Bingham S, Boeing H et al (2005) Serum sex steroids in premenopausal women and breast cancer risk within the European prospective investigation into cancer and nutrition (EPIC). J Natl Cancer Inst 97:755–765
Secreto G, Toniolo P, Berrino F, Recchione C, Cavalleri A, Pisani P, Totis A, Fariselli G, DiPietro S (1991) Serum and urinary androgens and risk of breast cancer in postmenopausal women. Cancer Res 51:2572–2576
Hankinson SE, Willett WC, Manson JE, Colditz GA, Hunter DJ, Spiegelman D, Barbieri RL, Speizer FE (1998) Plasma sex steroid hormone levels and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 90:1292–1299
Missmer SA, Eliassen AH, Barbieri RL, Hankinson SE (2004) Endogenous estrogen, androgen, and progesterone concentrations and breast cancer risk among postmenopausal women. J Natl Cancer Inst 96:1856–1865
Kaaks R, Tikk K, Sookthai D, Schock H, Johnson T, Tjonneland A, Olsen A, Overvad K, Clavel-Chapelon F, Dossus L et al (2014) Premenopausal serum sex hormone levels in relation to breast cancer risk, overall and by hormone receptor status—results from the EPIC cohort. Int J Cancer 134:1947–1957
Bulun SE, Lin Z, Imir G, Amin S, Demura M, Yilmaz B, Martin R, Utsunomiya H, Thung S, Gurates B et al (2005) Regulation of aromatase expression in estrogen-responsive breast and uterine disease: from bench to treatment. Pharmacol Rev 57:359–383
Pasqualini JR, Cortes-Prieto J, Chetrite G, Talbi M, Ruiz A (1997) Concentrations of estrone, estradiol and their sulfates, and evaluation of sulfatase and aromatase activities in patients with breast fibroadenoma. Int J Cancer 70:639–643
Pizzagalli F, Varga Z, Huber RD, Folkers G, Meier PJ, St-Pierre MV (2003) Identification of steroid sulfate transport processes in the human mammary gland. J Clin Endocrinol Metab 88:3902–3912
Chatterton RT Jr, Geiger AS, Khan SA, Helenowski IB, Jovanovic BD, Gann PH (2004) Variation in estradiol, estrogen precursors, and estrogen-related products in nipple aspirate fluid from normal premenopausal women. Cancer Epidemiol Biomarkers Prev 13:928–935
Chatterton RT Jr, Khan SA, Heinz R, Ivancic D, Lee O (2010) Patterns of sex steroid hormones in nipple aspirate fluid during the menstrual cycle and after menopause in relation to serum concentrations. Cancer Epidemiol Biomarkers Prev 19:275–279
Oren I, Fleishman SJ, Kessel A, Ben-Tal N (2004) Free diffusion of steroid hormones across biomembranes: a simplex search with implicit solvent model calculations. Biophys J 87:768–779
Broet P, de la Rochefordiere A, Scholl SM, Fourquet A, Mosseri V, Durand JC, Pouillart P, Asselain B (1995) Contralateral breast cancer: annual incidence and risk parameters. J Clin Oncol 13:1578–1583
Storm HH, Jensen OM (1986) Risk of contralateral breast cancer in Denmark 1943-80. Br J Cancer 54:483–492
Chatterton RT, Jr, Parker NP, Habe-Evans M, Bryk M, Scholtens DM, Khan SA (2010) Breast ductal lavage for assessment of breast cancer biomarkers. Horm Cancer
Chatterton RT, Muzzio M, Heinz R, Gann PH, Khan SA (2014) Methodological considerations in estrogen assays of breast fluid and breast tissue. Steroids
Kurian AW, McClure LA, John EM, Horn-Ross PL, Ford JM, Clarke CA (2009) Second primary breast cancer occurrence according to hormone receptor status. J Natl Cancer Inst 101:1058–1065
Meric-Bernstam F (2004) Breast conservation in breast cancer: surgical and adjuvant considerations. Curr Opin Obstet Gynecol 16:31–36
Heaphy CM, Bisoffi M, Fordyce CA, Haaland CM, Hines WC, Joste NE, Griffith JK (2006) Telomere DNA content and allelic imbalance demonstrate field cancerization in histologically normal tissue adjacent to breast tumors. J Int Cancer 119:108–116
Guenther S, Muirhead LJ, Speller AV, Golf O, Strittmatter N, Ramakrishnan R, Goldin RD, Jones E, Veselkov K, Nicholson J et al (2015) Spatially resolved metabolic phenotyping of breast cancer by desorption electrospray ionization mass spectrometry. Cancer Res 75:1828–1837
Bisoffi M, Heaphy CM, Griffith JK (2006) Telomeres: prognostic markers for solid tumors. Int J Cancer 119:2255–2260
Hagerman DD (1987) Human placenta estrogen synthetase (aromatase) purified by affinity chromatography. J Biol Chem 262:2398–2400
Pasqualini JR, Gelly C, Nguyen BL, Vella C (1989) Importance of estrogen sulfates in breast cancer. J Steroid Biochem 34:155–163
Chetrite GS, Cortes-Prieto J, Philippe JC, Wright F, Pasqualini JR (2000) Comparison of estrogen concentrations, estrone sulfatase and aromatase activities in normal, and in cancerous, human breast tissues. J Steroid Biochem Mol Biol 72:23–27
Ebeling P, Koivisto VA (1994) Physiological importance of dehydroepiandrosterone. Lancet 343:1479–1481
Helzlsouer KJ, Gordon GB, Alberg AJ, Bush TL, Comstock GW (1992) Relationship of prediagnostic serum levels of dehydroepiandrosterone and dehydroepiandrosterone sulfate to the risk of developing premenopausal breast cancer. Cancer Res 52:1–4
Secreto G, Zumoff B (1994) Abnormal production of androgens in women with breast cancer. Anticancer Res 14:2113–2117
Tworoger SS, Missmer SA, Eliassen AH, Spiegelman D, Folkerd E, Dowsett M, Barbieri RL, Hankinson SE (2006) The association of plasma DHEA and DHEA sulfate with breast cancer risk in predominantly premenopausal women. Cancer Epidemiol Biomarkers Prev 15:967–971
Dorgan JF, Stanczyk FZ, Longcope C, Stephenson HE Jr, Chang L, Miller R, Franz C, Falk RT, Kahle L (1997) Relationship of serum dehydroepiandrosterone (DHEA), DHEA sulfate, and 5-androstene-3 beta, 17 beta-diol to risk of breast cancer in postmenopausal women. Cancer Epidemiol Biomarkers Prev 6:177–181
Seymour-Munn K, Adams J (1983) Estrogenic effects of 5-androstene-3 beta, 17 beta-diol at physiological concentrations and its possible implication in the etiology of breast cancer. Endocrinology 112:486–491
Labrie F, Luu-The V, Labrie C, Belanger A, Simard J, Lin SX, Pelletier G (2003) Endocrine and intracrine sources of androgens in women: inhibition of breast cancer and other roles of androgens and their precursor dehydroepiandrosterone. Endocrine Rev 24:152–182
Morris KT, Toth-Fejel S, Schmidt J, Fletcher WS, Pommier RF (2001) High dehydroepiandrosterone-sulfate predicts breast cancer progression during new aromatase inhibitor therapy and stimulates breast cancer cell growth in tissue culture: a renewed role for adrenalectomy. Surgery 130:947–953
Kalimi M, Regelson W (1988) Physicochemical characterization of [3H] DHEA binding in rat liver. Biochem Biophys Res Commun 156:22–29
Okabe T, Haji M, Takayanagi R, Adachi M, Imasaki K, Kurimoto F, Watanabe T, Nawata H (1995) Up-regulation of high-affinity dehydroepiandrosterone binding activity by dehydroepiandrosterone in activated human T lymphocytes. J Clin Endocrinol Metabol 80:2993–2996
Haddad SA, Lunetta KL, Ruiz-Narvaez EA, Bensen JT, Hong CC, Sucheston-Campbell LE, Yao S, Bandera EV, Rosenberg L, Haiman CA et al (2015) Hormone-related pathways and risk of breast cancer subtypes in African American women. Breast Cancer Res Treat 154:145–154
Wiebe JP, Beausoleil M, Zhang G, Cialacu V (2010) Opposing actions of the progesterone metabolites, 5alpha-dihydroprogesterone (5alphaP) and 3alpha-dihydroprogesterone (3alphaHP) on mitosis, apoptosis, and expression of Bcl-2, Bax and p21 in human breast cell lines. J Steroid Biochem Mol Biol 118:125–132
Wiebe JP, Zhang G, Welch I, Cadieux-Pitre HA (2013) Progesterone metabolites regulate induction, growth, and suppression of estrogen- and progesterone receptor-negative human breast cell tumors. Breast Cancer Res 15:R38
Wiebe JP, Rivas MA, Mercogliano MF, Elizalde PV, Schillaci R (2015) Progesterone-induced stimulation of mammary tumorigenesis is due to the progesterone metabolite, 5alpha-dihydroprogesterone (5alphaP) and can be suppressed by the 5alpha-reductase inhibitor, finasteride. J Steroid Biochem Mol Biol 149:27–34
Lewis MJ, Wiebe JP, Heathcote JG (2004) Expression of progesterone metabolizing enzyme genes (AKR1C1, AKR1C2, AKR1C3, SRD5A1, SRD5A2) is altered in human breast carcinoma. BMC Cancer 4:27
Rizner TL, Penning TM (2014) Role of aldo-keto reductase family 1 (AKR1) enzymes in human steroid metabolism. Steroids 79:49–63
Penning TM, Burczynski ME, Jez JM, Hung CF, Lin HK, Ma H, Moore M, Palackal N, Ratnam K (2000) Human 3alpha-hydroxysteroid dehydrogenase isoforms (AKR1C1-AKR1C4) of the aldo-keto reductase superfamily: functional plasticity and tissue distribution reveals roles in the inactivation and formation of male and female sex hormones. Biochem J 351:67–77
Verma U, Kapur MM, Laumas KR (1978) Characterization of progesterone receptors and metabolism of progesterone in the normal and cancerous human mammary gland. J Steroid Biochem 9:569–577
Pasqualini JR, Chetrite G (2008) The anti-aromatase effect of progesterone and of its natural metabolites 20alpha- and 5alpha-dihydroprogesterone in the MCF-7aro breast cancer cell line. Anticancer Res 28:2129–2133
Wiebe JP (2006) Progesterone metabolites in breast cancer. Endocr Relat Cancer 13:717–738
Kasashima S, Kawashima A, Ozaki S, Nakanuma Y (2012) Expression of 5alpha-reductase in apocrine carcinoma of the breast and its correlation with clinicopathological aggressiveness. Histopathology 60:E51–E57
Acknowledgments
This study was supported by a grant from the National Institutes of Health, National Cancer Institute R01 CA 120555 to Seema A. Khan, P.I.
Authors’ Contributions
All authors have read and approved the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Consent of Publication
This work has not been and will not be submitted elsewhere until the editorial board has decided whether to publish the article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 26 kb)
Rights and permissions
About this article
Cite this article
Chatterton, R.T., Heinz, R.E., Fought, A.J. et al. Nipple Aspirate Fluid Hormone Concentrations and Breast Cancer Risk. HORM CANC 7, 127–136 (2016). https://doi.org/10.1007/s12672-016-0252-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-016-0252-7