Abstract
Background/Purpose
Patients with functional dyspepsia (FD) have poor health-related quality of life (HRQOL), but Indian data are lacking. Also, there is non-availability of validated disease-specific questionnaire to assess HRQOL in Hindi-speaking patients with dyspepsia. We aimed to develop and validate a reliable translation of Short-Form Nepean Dyspepsia Index (SF-NDI) in Hindi, and assess the impact of FD on HRQOL in Indian patients.
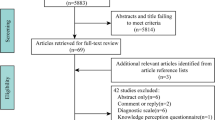
Methods
Cross-cultural adaptation of English version of SF-NDI, translation to Hindi, and adaptation of Hindi version were performed using standard procedures. English and Hindi versions were assessed against Short Form-36 (SF-36), examining for internal consistency, test–retest reliability, and validity.
Results
Total 211 FD patients (144 Hindi speaking, 67 English speaking) were enrolled (mean age 40.8 ± 11.7 years; male:female = 115:96). Median total SF-NDI scores for both languages were 38.75 and 40.0, respectively. Test–retest reliability intraclass correlation coefficients were 0.85 (Hindi) and 0.89 (English). Internal consistency evaluation revealed Cronbach’s α coefficient of 0.79–0.86 (Hindi) and 0.78–0.89 (English). SF-NDI sub-scales showed moderate to good correlation with various domains of SF-36 (content validity). There was significant (p < 0.001) decline of HRQOL in patients with severe dyspepsia relative to those with mild dyspepsia (construct validity). On multivariate analysis, factors independently associated with HRQOL were duration of symptoms and dyspepsia severity.
Conclusion
Both English and Hindi versions of SF-NDI are reliable and valid for HRQOL assessment in Indian FD patients, and will be useful in future epidemiological and clinical studies. Indian FD patients have poor HRQOL, being worse in those with severe dyspepsia and longer duration of symptoms.


Similar content being viewed by others
References
Miwa H, Ghoshal UC, Gonlachanvit S, et al. Asian consensus report on functional dyspepsia. J Neurogastroenterol Motil. 2012;18:150–68.
Stanghellini V, Chan FK, Hasler WL, et al. Gastroduodenal disorders. Gastroenterology. 2016;150:1380–92.
Ford AC, Mahadeva S, Carbone MF, Lacy BE, Talley NJ. Functional dyspepsia. Lancet. 2020;396:1689–702.
Goyal O, Nohria S, Dhaliwal AS, et al. Prevalence, overlap, and risk factors for Rome IV functional gastrointestinal disorders among college students in northern India. Indian J Gastroenterol. 2021;40:144–53.
Mahadeva S, Wee HL, Goh KL, Thumboo J. Quality of life in South East Asian patients who consult for dyspepsia: validation of the short form Nepean Dyspepsia Index. Health Qual Life Outcomes. 2009;7:45.
Rane SV, Asgaonkar B, Rathi P, et al. Effect of moderate aerobic exercises on symptoms of functional dyspepsia. Indian J Gastroenterol. 2021;40:189–97.
Kumar A, Pate J, Sawant P. Epidemiology of functional dyspepsia. J Assoc Physicians India. 2012;60 Suppl:9–12.
Talley NJ, Locke GR 3rd, Lahr BD, et al. Functional dyspepsia, delayed gastric emptying, and impaired quality of life. Gut. 2006;55:933–9.
VanOudenhove L, Vandenberghe J, Vos R, Holvoe L, Demyttenaere K, Tack J. Risk factors for impaired health-related quality of life in functional dyspepsia. Aliment Pharmacol Ther. 2011;33:261–74.
Haag S, Senf W, Tagay S, et al. Is there any association between disturbed gastrointestinal visceromotor and sensory function and impaired quality of life in functional dyspepsia? Neurogastroenterol Motil. 2010;22:262-e79.
Haag S, Senf W, Häuser W, et al. Impairment of health-related quality of life in functional dyspepsia and chronic liver disease: the influence of depression and anxiety. Aliment Pharmacol Ther. 2008;27:561–71.
Mones J, Adan A, Segu JL, Lopez JS, Artes M, Guerrero T. Quality of life in functional dyspepsia. Dig Dis Sci. 2002;47:20–6.
Azimi M, Zolala F, Baneshi MR, Zahedi MJ. Validation of short-form Nepean Dyspepsia Index in Iranian patients with functional dyspepsia. Govaresh. 2017;22:89–94.
Lee HJ, Lee SY, Kim JH, et al. Depressive mood and quality of life in functional gastrointestinal disorders: differences between functional dyspepsia, irritable bowel syndrome and overlap syndrome. Gen Hosp Psychiatry. 2010;32:499–502.
Mahadeva S, Goh KL. Anxiety, depression and quality of life differences between functional and organic dyspepsia. J Gastroenterol Hepatol. 2011;26 Suppl3:49–52.
Jeong JJ, Choi MG, Cho YS, et al. Chronic gastrointestinal symptoms and quality of life in the Korean population. World J Gastroenterol. 2008;14:6388–94.
Mahadeva S, Yadav H, Rampal S, Goh KL. Risk factors associated with dyspepsia in a rural Asian population and its impact on quality of life. Am J Gastroenterol. 2010;105:904–12.
Mahadeva S, Wee HL, Goh KL, Thumboo J. The EQ-5D (Euroqol) is a valid generic instrument for measuring quality of life in patients with dyspepsia. BMC Gastroenterol. 2009;9:20.
What is the most spoken language? In: Ethnologue. SIL International. 2021. https://www.ethnologue.com/guides/most-spoken-languages. Last accessed 08 Nov 2021
Talley NJ, Verlinden M, Jones M. Validity of a new quality of life scale for functional dyspepsia: a United States multicentre trial of the Nepean Dyspepsia Index. Am J Gastroenterol. 1999;94:2390–7.
Talley NJ, Verlinden M, Jones M. Quality of life in functional dyspepsia: responsiveness of the Nepean Dyspepsia Index and development of a new 10-item short form. Aliment Pharmacol Ther. 2001;15:207–16.
Nkurunziza A, Dusabejambo V, Everhart K, Bensen S, Walker T. Validation of the Kinyarwanda-version Short-Form Leeds Dyspepsia Questionnaire and Short-Form Nepean Dyspepsia Index to assess dyspepsia prevalence and quality-of-life impact in Rwanda. BMJ Open. 2016;6:e011018.
Sheikh S. Modified Kuppuswamy socioeconomic scale update of the year 2020. Indian J Forensic Community Med. 2020;7:1-3
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston: Nirmond press; 1993.
Sinha R, Van den Heuvel WJ, Arokiasamy P. Validity and reliability of MOS Short Form Health Survey (SF-36) for use in India. Indian J Community Med. 2013;38:22–6.
Leplege A, Verdier A. The adaptation of health status measures: methodological aspects of the translation procedure. In: Shumaker SA, Berzon RA, editors. The international assessment of health-related quality of life: theory, translation, measurement and analysis. Oxford: Rapid Communications; 1995. p. 93–101.
Kim YS, Kim N. Functional dyspepsia: a narrative review with a focus on sex-gender differences. J Neurogastroenterol Motil. 2020;26:322–34.
Hantoro IF, Syam AF, Mudjaddid E, Setiati S, Abdullah M. Factors associated with health-related quality of life in patients with functional dyspepsia. Health Qual Life Outcomes. 2018;16:83.
Halder SL, Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Impact of functional gastrointestinal disorders on health-related quality of life: a population-based case-control study. Aliment Pharmacol Ther. 2004;19:233–42.
Dodds WJ, Hogan WJ, Helm JF, Dent J. Pathogenesis of reflux esophagitis. Gastroenterology. 1981;81:376–94.
Bitwayiki R, Orikiiriza JT, Kateera F, et al. Dyspepsia prevalence and impact on quality of life among Rwandan healthcare workers: A cross-sectional survey. S Afr Med J. 2015;105:1064-9.
Fraser A, Delaney BC, Ford AC, Qume M, Moayyedi P. The Short-Form Leeds Dyspepsia Questionnaire validation study. Aliment Pharmacol Ther. 2007;25:477–86.
Tian XP, Li Y, Liang FR, et al. Translation and validation of the Nepean Dyspepsia Index for functional dyspepsia in China. World J Gastroenterol. 2009;15:3173–7.
Westbrook JI, Talley NJ, Westbrook MT. Gender differences in the symptoms and physical and mental well-being of dyspeptics: a population based study. Qual Life Res. 2002;11:283–91.
Huang I, Pranata R, Pangestu W, et al. The prevalence of uninvestigated dyspepsia and the association of physical exercise with quality of life of uninvestigated dyspepsia patients in Indonesia: an internet-based survey. Indian J Gastroenterol. 2021;40:176–82.
Lacy BE, Weiser KT, Kennedy AT, Crowell MD, Talley NJ. Functional dyspepsia: the economic impact to patients. Aliment Pharmacol Ther. 2013;38:170–7.
Shetty A, Balaraju G, Shetty S, Pai CG. Diagnostic utility of alarm features in predicting malignancy in patients with dyspeptic symptoms. Indian J Gastroenterol. 2021;40:183–8.
Jones R, Lydeard S. Dyspepsia in the community: a follow-up study. Br J Clin Pract. 1992;46:95–7.
Ahlawat SK, Richard Locke G, et al. Dyspepsia consulters and patterns of management: a population-based study. Aliment Pharmacol Ther. 2005;22:251–9.
Goyal O, Nohria S, Batta S, Dhaliwal A, Goyal P, Sood A. Low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols diet versus traditional dietary advice for functional dyspepsia: a randomized controlled trial. J Gastroenterol Hepatol. 2021. https://doi.org/10.1111/jgh.15694.
Funding
Department of Gastroenterology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
OG, PG, HK, JK, PK, and AS declare no competing interests.
Ethics approval
The questionnaire and methodology for this study were approved by the institutional ethics committee (DMCH/R&D/2021/13). All procedures performed were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki Declaration and its later amendments.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Goyal, O., Goyal, P., Kishore, H. et al. Quality of life in Indian patients with functional dyspepsia: Translation and validation of the Hindi version of Short-Form Nepean Dyspepsia Index. Indian J Gastroenterol 41, 378–388 (2022). https://doi.org/10.1007/s12664-021-01233-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-021-01233-0