Abstract
Background
The incidence of hepatobiliary cancer is steadily increasing. It is unclear if this rise is related to increasing trends in obesity, metabolic syndrome, and lifestyle changes.
Methods
A case-control study was performed using the Health Improvement Network (THIN) database. Cases with a diagnosis of liver, bile duct, and gallbladder cancers were matched in a 1:2 fashion with controls and analyzed for potential associations between hepatobiliary cancer and obesity/metabolic syndrome.
Results
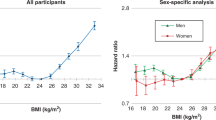
Four thousand two hundred and eighty-seven patients (62% male, 38% female) with hepatobiliary cancers were matched with 8574 controls. On univariate analysis, body mass index (BMI), smoking, diabetes, alcohol consumption, ischemic heart disease, and hypertension were associated with hepatobiliary cancer. Statin use and non-smoking status had an inverse association. On multivariate analysis, BMI, diabetes, hypertension, ischemic heart disease, and insulin use were associated with the risk of hepatobiliary cancer. Statin use and non-smoking status were protective. On modeling BMI, each of diabetes and hypertension as a single covariate, there was a significant association with hepatobiliary cancer (1.59 [1.49–1.69], p < 0.001) which persisted despite adjusting for increasing age (1.006 [1005–1.006], p < 0.001) and background liver cirrhosis (1.037 [1.03–1.044], p < 0.001).
Conclusions
Obesity and metabolic syndrome are associated with the risk of hepatobiliary cancer. Statin use seems to be protective.

Similar content being viewed by others
References
Cancer Research UK. Liver cancer incidence trends over time. Cancer Research UK. 2017; cited 2017; Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/liver-cancer/incidence. Accessed 1/7/18.
SEER, Cancer Stat Facts: Liver and Intrahepatic Bile Duct Cancer., in Surveillance, Epidemiology, and End Results Program. 2017; NIH: National Cancer Institute.
Welzel TM, McGlynn KA, Hsing AW, O'Brien TR, Pfeiffer RM. Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the United States. J Natl Cancer Inst. 2006;98:873–5.
Khan SA, Emadossadaty S, Ladep NG, et al. Rising trends in cholangiocarcinoma: is the ICD classification system misleading us? J Hepatol. 2012;56:848–54.
Hassan MM, Hwang LY, Hatten CJ, et al. Risk factors for hepatocellular carcinoma: synergism of alcohol with viral hepatitis and diabetes mellitus. Hepatology. 2002;36:1206–13.
Alberti KG, Zimmet P, Shaw J. Metabolic syndrome–a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med. 2006;23:469–80.
Simon TG, King LY, Chong DQ, et al. Diabetes, metabolic comorbidities and risk of hepatocellular carcinoma: results from two prospective cohort studies. Hepatology. 2018;67:1797–806.
Wu Q, He XD, Yu L, Liu W, Tao LY. The metabolic syndrome and risk factors for biliary tract cancer: a case-control study in China. Asian Pac J Cancer Prev. 2012;13:1963–9.
THIN. THIN. The Health Improvement Network. CSD Health Research. 2015; Available from: https://www.visionhealth.co.uk/portfolio-items/the-health-improvement-network-thin/. Accessed 1/7/18.
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–38.
Chen HF, Chen P, Li CY. Risk of malignant neoplasms of liver and biliary tract in diabetic patients with different age and sex stratifications. Hepatology. 2010;52:155–63.
Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013;10:656–65.
Shan J, Shen J, Liu L, et al. Nanog regulates self-renewal of cancer stem cells through the insulin-like growth factor pathway in human hepatocellular carcinoma. Hepatology. 2012;56:1004–14.
McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol. 2015;62:1148–55.
Paradis V, Zalinski S, Chelbi E, et al. Hepatocellular carcinomas in patients with metabolic syndrome often develop without significant liver fibrosis: a pathological analysis. Hepatology. 2009;49:851–9.
Piscaglia F, Svegliati-Baroni G, Barchetti A, et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: a multicenter prospective study. Hepatology. 2016;63:827–38.
Loomis AK, Kabadi S, Preiss D, et al. Body mass index and risk of nonalcoholic fatty liver disease: two electronic health record prospective studies. J Clin Endocrinol Metab. 2016;101:945–52.
Zhang W, Sun B. Impact of age on the survival of patients with liver cancer: an analysis of 27,255 patients in the SEER database. Oncotarget. 2015;6:633–41.
Singh S, Singh PP, Singh AG, Murad MH, Sanchez W. Anti-diabetic medications and the risk of hepatocellular cancer: a systematic review and meta-analysis. Am J Gastroenterol. 2013;108:881–91.
Smith U, Gale EM. Cancer and diabetes: are we ready for prime time? Diabetologia. 2010;53:1541–4.
Chiang GG, Abraham RT. Targeting the mTOR signalling network in cancer. Trends Mol Med. 2007;13:433–42.
Yokomichi H, Nagai A, Hirata M, et al. Statin use and all-cause and cancer mortality: BioBank Japan cohort. J Epidemiol. 2017;27:S84–91.
Ogunwobi OO, Beales IL. Statins inhibit proliferation and induce apoptosis in Barrett’s esophageal adenocarcinoma cells. Am J Gastroenterol. 2008;103:825–37.
Demierre MF, Higgins PD, Gruber SB, Hawk E, Lippman SM. Statins and cancer prevention. Nat Rev Cancer. 2005;5:930–42.
Lonardo A, Loria P. Potential for statins in the chemoprevention and management of hepatocellular carcinoma. J Gastroenterol Hepatol. 2012;27:1654–64.
Bardou M, Barkun A, Martel M. Effect of statin therapy on colorectal cancer. Gut. 2010;59:1572–85.
Bansal D, Undela K, D'Cruz S, Schifano F. Statin use and risk of prostate cancer: a meta-analysis of observational studies. PLoS One. 2012;7:e46691.
Shi M, Zheng H, Nie B, Gong W, Cui X. Statin use and risk of liver cancer: an update meta-analysis. BMJ Open. 2014;4:e005399.
Undela K, Srikanth V, Bansal D. Statin use and risk of breast cancer: a meta-analysis of observational studies. Breast Cancer Res Treat. 2012;135:261–9.
Shimoyama S. Statins and gastric cancer risk. Hepatogastroenterology. 2011;58:1057–61.
Cui X, Xie Y, Chen M, Li J, Liao X, Shen J, et al. Statin use and risk of pancreatic cancer: a meta-analysis. Cancer Causes Control. 2012;23:1099–111.
Peng YC, Lin CL, Hsu WY, et al. Statins are associated with a reduced risk of cholangiocarcinoma: a population-based case-control study. Br J Clin Pharmacol. 2015;80:755–61.
Acknowledgements
None.
Funding details
This research was funded by a grant from the South Staffordshire Medical Centre Charitable Trust (The Rotha Abraham Bequest).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SM, and RM declare that they have no conflict of interest.
Ethical clearance
The authors declare that the study was performed in a manner conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the content of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/ findings and content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Menon, S., Mathew, R. Association between metabolic syndrome and hepatobiliary cancers: A case-control study. Indian J Gastroenterol 38, 61–68 (2019). https://doi.org/10.1007/s12664-018-0925-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-018-0925-y