Abstract
Aim
During second wave of COVID pandemic, India faced heavy surge of mucormycosis. Treatment option for these patients included either total or partial maxillectomy with primary closure. Rehabilitation of these patients became challenging because of their age and size of defect. The purpose of the present study is to present a new digital technique for the fabrication of patient-specific zygoma implants (PSI) and to report on its survival and complication rates.
Material and Methods
Total 21 patients who had undergone either partial or total maxillectomy after mucormycosis and who were disease-free clinically and radiographically for 6 or more months post-resection were rehabilitated using patient-specific zygoma implant. CT scan was obtained for all patients post-maxillectomy for evaluation of existing bone condition. Exocad software was used for virtual surgical planning of zygoma implant considering surgical and prosthetic technicality to achieve goal of maximum functionality and sustainability.
Result
All the patients were followed up after 15, 30, 45 and 90 days and there after every month for evaluation of soft tissue healing, infection, dehiscence, loosening of prosthesis, eating efficiency and aesthetic. Follow-up period for all 15 patients was in the range of 6–12 months.
Conclusion
In case of post-mucor maxillectomy patients, use of PSI offers the advantages of minimal bone augmentation, reduction in time required to restore lost function, and reduced financial burden of multiple procedures. Therefore, PSI may represent a valid alternative treatment for the prosthetic restoration of post-mucor maxillectomy patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mucormycosis, a rapidly invasive fungal infection affecting immunocompromised elderly patients, was a term relatively unheard of, up until the second wave of Corona Virus Disease of 2019 (COVID-19) pandemic. India reported an incidence of over 45,000 cases between the months of April and July 2021 with 77.6% cases being of Rhinocerebral type [1]. During second wave of COVID-19, it was observed to not only just be affecting geriatric population, but also younger individuals even without any preexisting medical condition [2]. The surgical management of advanced stage of this debilitating disease involved removal of necrotic bone often requiring total or partial maxillectomy and primary closure with buccal and palatal mucosa to limit its spread in future. Rehabilitation of these patients remains a herculean task owing to age of individuals and size of the defect. Numerous surgical and prosthetic challenges like lack of maxillary bone including pterygoid plates sometimes zygomatic bone involvement, adherence of nasal and sinus mucosa with palatal mucosa, fibrosed palatal mucosa, loss of lip support, reduced stress bearing area, lack of vertical guidance and over closure of mandible need to be addressed during rehabilitation. The primary goal for rehabilitation of these patients needs to be established as normal function with minimal morbidity and long-term sustainability. Conventional treatment option for maxillary reconstruction includes augmentation with free bone graft for placement of endosseous implants which although successfully brings along myriad of complications like secondary donor site morbidity, variable rate of resorption of graft, prolonged time for rehabilitation, financial burden on patients and need for additional surgical procedure [3]. Quad zygoma remains a viable option but impractical for patients in which the zygomatic bone has been denuded off to remove the necrosed bone [4]. The field of oral and maxillofacial surgery has grown by leaps and bound with the advent of recent acquisition techniques likes cone beam computed tomography (CBCT) and intra-oral scanners along with CAD/CAM (computer-assisted design/computer-assisted manufacturing) software which enables designing and manufacturing of patient-specific implants (PSI) with greater precision. The direct metal laser sintering technique (DMLS) in particular opens up new array of opportunities for fabrication of custom-made patient-specific implants according to the anatomical need of each patient [3]. These digital advancements allow us to revisit some older techniques like sub-periosteal implants which although had been abandoned in the past, can now be utilized in noninvasive fashion with better results [3, 5, 6]. These implants can be present as a boon for rehabilitation of post-maxillectomy cases where placement of endosseous implants requires long and complex regenerative surgeries and especially post-mucor maxillectomy patients with limited financial aid and frequently associated comorbidities [7]. The purpose of the present clinical study is to present a new digital technique for the fabrication of patient-specific zygoma implants and to report on the survival and complication rates encountered when using these PSI.
Materials and Methods
Total 21 mucormycosis afflicted patients who had undergone either partial or total maxillectomy with primary closure and who were disease-free clinically and radiographically for more than 6-month post-resection were rehabilitated using custom-made patient-specific zygoma implant. Computed tomography (CT) scan was obtained for all patients post-maxillectomy for evaluation of existing bone condition (Fig. 1). Exocad software was used for virtual surgical planning (VSP) taking in consideration the surgical and prosthetic aspects of zygoma implant to achieve goal of maximum functionality and sustainability.
Technical details of design (surgical) are as follows:
-
1.
Three-piece design (Fig. 2) covering entire body of zygoma to reduce surgical exposure leading to oronasal or oroantral communication.
-
2.
Wide base to cover strong zygoma for optimal mechanical stability.
-
3.
Extension on lateral orbital wall for mechanical advantage utilizing bicortical 13–15-mm screws.
-
4.
Optimal length of bars to avoid impingement on soft tissue, and bars were kept optimally short so that minimal implant remains inside oral cavity.
-
5.
Sufficient space between two bars for closure of soft tissue in between and around bar.
-
6.
Angulation of bar is designed to distribute biting force on wider base.
Technical detail of design (prosthetic) is as follows:
-
1.
Threads in the cylinder to attach OT equator bridge (Rhein’83) for prosthetic flexibility.
-
2.
Placement of abutments corresponding to natural canine and molar area for optimal functionality, to gain anteroposterior spread and aesthetic.
-
3.
Bar-supported screw retained prosthesis.
-
4.
Self-cleansing area above prosthesis for proper oral hygiene.
-
5.
Two-side stress breaker to reduce biting force.
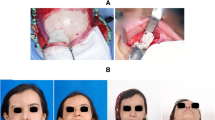
Finite element analysis was performed to assess if the implant strength and fatigue resistance could withstand occlusal forces. All patients were operated under general anesthesia. Small 15-mm vestibular incision was used bilaterally directly over zygoma body away from fibrosed and retracted palatal mucosa after identifying parotid duct (Fig. 3). Sub-periosteal undermining over zygoma body was carried out up to root of zygomatic arch and frontozygomatic suture (Fig. 3). Bilateral implants were adapted over zygoma body in pocket created by sub-periosteal undermining. Titanium bar was fixed connecting both side of implant bar using screws. Prosthesis was fixed to bar and placed in occlusion with lower arch. After rechecking adaptation of implants on surface of zygoma body while maintaining prosthesis in occlusion, both side implants were now fixed using self-drilling titanium screws (Fig. 3). Size of screws were predetermined during virtual surgical planning. Screws at lateral orbital rim were fixed using trocar. Total 9–12 screws were used on each side for maximum stability of implant. Mucograft was used around lower end of implant bar for soft tissue healing. Buccal pad of fat was used to cover implant surface for adequate healing of soft tissue. Closure of incision was done with resorbable suture while maintaining self-cleansing area (Fig. 4). Postoperative CT scan was obtained 48 h after surgery to check adaptation of implant to zygoma body (Fig. 5).
Result
All the patients were followed up after 15, 30, 45 and 90 days and there after every month for evaluation of soft tissue healing, infection, dehiscence, loosening of prosthesis, eating efficiency and aesthetic. Follow-up period for all 21 patients was in range of 6 months to 1 year. Extra-oral approach was needed in two patients who had mild degree of oral submucosa fibrosis. Two patients developed mild soft tissue infection 15-day postoperatively which resolved with local irrigation and oral antibiotics. Soft tissue healing around implant was satisfactory in all patients without any sign of infection or dehiscence after 6 months. Three patient developed loosening of prosthesis 1-month post-fixation in which case new prosthesis was fabricated using VSP and fixed on already well-healed PSI. Two patients had occlusal discrepancy which was corrected 45-day post-surgery (Fig. 6). One patient had developed gummy smile, for which re-fabrication of prosthesis unit was planned (Fig. 6). Prosthesis and bar were removed in two patients who had completed their 6 months of follow-up to evaluate soft tissue healing around bar extending from implant body. There was a thick tissue formed around bar exposed to oral cavity due to use of mucograft during surgery. Finite element analysis revealed that the stresses endured by the implant under maximal loading forces were lesser than the yield and ultimate strength of the PSI making it a design fit for mastication.
Discussion
Post-COVID mucormycosis leaves individuals with huge anatomical defects, heavy financial burden and emotional scars for life. Rehabilitation of such patients has become a tedious task for maxillofacial surgeons taking into consideration the greater size of defect and anatomical difficulties. This customized prosthesis-driven zygomatic implant offers an alternative option to rehabilitate the primarily closed defect with minimal morbidity and greater functional adaptability. Although the sub-periosteal implants have been renounced due to the technical difficulty in fabrication procedure, severe inflammation and improper fixation methods, the three-piece design used for these patients have been modified with the latest advancements for designing, surgical placement and functional outcome [3].
The use of titanium over previously used chrome cobalt alloys for sub-periosteal implants provides better tissue compatibility and minimal incidence of implant failure/exposure/rejection [3, 7]. Conventional sub-periosteal implants were placed using mid-crestal incision for exposure of the surgical site, and the digitally fabricated implants were placed using vestibular incision directly over the body of zygoma which provides adequate exposure, sufficient soft tissue for closure around the implant and zero incidence of wound dehiscence [5].
Fixation was done with self-drilling screws, and trans-buccal trocar after correct adaptation of the implant was checked by connecting the implant with the prosthesis and maintaining it in occlusion with the mandibular arch. The self-drilling screws and trocar were used to provide ease of placing the screws perpendicular to the plate and achieve better fixation [8].
The use of intra-oral vestibular incision, small stab incision for trocar insertion and placement of prosthesis which provides adequate lip support improved the edentulous facial appearance of the patients without any signification facial scar.
Cerea et al. reported 1.4% case of biological complication with recurrent localized infection which was managed with long-term oral antibiotics. They also reported 8.9% incidence of prosthetic complication [3]. In the current clinical paper also, minor postoperative complications like mild infection (two cases), occlusal discrepancy (two cases) and prosthesis loosening (three cases) were encountered which were all managed in out-patient setting with oral antibiotics and prosthetic corrections without need for any fervent intervention.
Owing to the digitally engineered design of the implant, the patient can be provided with a functional prosthesis in a single-stage surgical procedure. The prosthesis connection system is part of the implant that is placed over the strong zygomatic bone which enables prosthesis placement immediately over the bar attached to the implant. The prosthodontic rehabilitation with the PSI has been done using established techniques so the expected success rate should be comparable with that of conventional quad zygoma implants [4]. The digitally fabricated patient-specific zygomatic implant can be inferred to provide optimal stability and functional rehabilitation in post-mucor maxillectomy patients over a relatively much shorter period of time with minimal surgical morbidity but a longer follow-up and larger sample size need to be maintained for better assessment of its benefits.
Conclusion
Within the limits of the present study (limited follow-up time and low number of patients treated), the clinical application of custom-made patient-specific zygoma implants showed a satisfactory survival rate and low complication rates. In the case of post-mucor maxillectomy patients with primarily closed buccal and palatal tissue, the use of PSI offers the advantages of minimal bone augmentation treatment needs, reduction in time required to restore lost prosthetic function and reduced financial burden of multiple procedures. Therefore, custom-made PSI may represent a valid alternative treatment procedure for the prosthetic restoration of post-mucor maxillectomy patients, where placement of endosseous implants is not possible [6, 7]. However, further studies on a larger sample of patients and with long-term follow-up are needed to confirm the positive outcomes emerging from this clinical research.
Code Availability
Not required.
References
Hindustantimes (2021) India reported over 45,000 black fungus cases so far, says Mandaviya in RS. Jul 2020-21. https://www.hindustantimes.com/india-news/indiareported-over-45-000-black-fungus-cases-so-far-says-mandaviya-in-rs-101626781531292.html. Accessed 20, 2021 2021
Singh AK, Singh R, Joshi SR, Misra A (2021) Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. https://doi.org/10.1016/j.dsx.2021.05.019
Cerea M, Dolcini GA (2018) Custom-made direct metal laser sintering titanium subperiosteal implants: a retrospective clinical study on 70 patients. Biomed Res Int 2018:1–11
Nandavar A, Shah A, Nair S, Kumar B (2019) Rehabilitation of maxillectomy patients using quad zygomatic implants—a case series. Int J Oral Maxillofac Surg 48:44
Gellrich NC, Zimmerer RM, Spalthoff S, Jehn P, Pott PC, Rana M, Rahlf B (2017) A customised digitally engineered solution for fixed dental rehabilitation in severe bone deficiency: a new innovative line extension in implant dentistry. J Craniomaxillofac Surg 45(10):1632–1638
Mommaerts MY (2019) Evolutionary steps in the design and biofunctionalization of the additively manufactured sub-periosteal jaw implant ‘AMSJI’ for the maxilla. Int J Oral Maxillofac Surg 48:108–114
Vosselman N, Merema BJ, Schepman KP, Raghoebar GM (2019) Patient-specific sub-periosteal zygoma implant for prosthetic rehabilitation of large maxillary defects after oncological resection. Int J Oral Maxillofac Surg 48:115–117
Panneerselvam E, Balasubramanian S, Kempraj J, Babu VR, Raja VBKK (2020) Management of zygomatic arch fractures by intraoral open reduction and transbuccal fixation: a technical note. Craniomaxillofac Trauma Reconstr 13(2):130–132. https://doi.org/10.1177/1943387520911866
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr. NP, Dr. AM, Dr. PP, Dr. AF and Dr. SG. The first draft of the manuscript was written by Dr. NP, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
I declare that I do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Ethics Approval
Not required.
Informed Consent
Informed consent was taken from the individual.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Patel, N., Mel, A., Patel, P. et al. A Novel Method to Rehabilitate Post-mucormycosis Maxillectomy Defect by Using Patient-Specific Zygoma Implant. J. Maxillofac. Oral Surg. 22 (Suppl 1), 118–123 (2023). https://doi.org/10.1007/s12663-023-01847-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-023-01847-1