Abstract
Purpose
Anesthesia information management systems (AIMS) are gradually replacing paper documentation of anesthesia care. This study sought to determine the current status of AIMS adoption and the level of health informatics expertise in Canadian academic anesthesia departments.
Methods
Department heads or their designates of Canadian academic anesthesia departments were invited by e-mail to complete an online survey between September 2019 and February 2020. The survey elicited information on current AIMS or future plans for an AIMS installation, the number of department members dedicated to clinical informatics issues, the gross level of health informatics expertise at each department, perceived advantages of AIMS, and perceived disadvantages of and barriers to implementation of AIMS.
Results
Of the 64 departments invited to participate, 63 (98.4%) completed the survey. Only 21 (33.3%) of the departments had AIMS. Of the 42 departments still charting on paper, 23 (54.8%) reported planning to install an AIMS within the next five years. Forty-six departments (73%) had at least one anesthesiologist tasked with dealing with AIMS or electronic health record issues. Most reported having no department members with extensive knowledge or formal training in health informatics. The top three perceived barriers and disadvantages to an AIMS installation were its initial cost, lack of funding, and a lack of technical support dedicated specifically to AIMS. The top three advantages departments wished to prioritize with AIMS were accurate clinical documentation, better data for quality improvement initiatives, and better data for research.
Conclusions
A majority of Canadian academic anesthesia departments are still using paper records, but this trend is expected to reverse in the next five years as more departments install an AIMS. Health informatics expertise is lacking in most of the departments, with a minority planning to support the training of future anesthesia informaticians.
Résumé
Objectif
Les systèmes de gestion de l’information en anesthésie (SGIA) remplacent progressivement la documentation sur papier des soins anesthésiques. Cette étude a tenté de déterminer l’état actuel de l’adoption des SGIA et le niveau d’expertise en informatique de la santé dans les départements universitaires d’anesthésie canadiens.
Méthode
Les chefs de département ou des responsables désignés des départements universitaires d’anesthésie canadiens ont été invités par courriel à remplir un sondage électronique entre les mois de septembre 2019 et février 2020. L’enquête a permis d’obtenir de l’information sur les SGIA actuels ou les plans futurs d’implantation d’un SGIA, le nombre de membres du département en charge des questions d’informatique clinique, le niveau brut d’expertise en informatique de la santé dans chaque département, les avantages perçus des SGIA, et les inconvénients perçus ainsi que les obstacles à la mise en œuvre des SGIA.
Résultats
Sur les 64 départements invités à participer, 63 (98,4 %) ont rempli le sondage. Seuls 21 (33,3 %) départements disposaient d’un SGIA. Sur les 42 départements utilisant encore des dossiers papier, 23 (54,8 %) ont déclaré avoir l’intention d’installer un SGIA au cours des cinq prochaines années. Quarante-six départements (73 %) comptaient au moins un anesthésiologiste chargé de gérer les problèmes liés au SGIA ou aux dossiers médicaux électroniques. La plupart des départements ont déclaré ne pas compter, parmi leurs membres, de personne possédant des connaissances approfondies ou une formation officielle en informatique de la santé. Les trois principaux obstacles et inconvénients perçus à la mise en oeuvre d’un SGIA étaient son coût initial, le manque de financement et un manque de soutien technique dédié spécifiquement aux SGIA. Les trois principaux avantages que les départements souhaitaient prioriser avec un SGIA étaient une documentation clinique exacte, de meilleures données pour les initiatives d’amélioration de la qualité et de meilleures données pour la recherche.
Conclusion
La majorité des départements universitaires d’anesthésie canadiens utilisent toujours des dossiers papier, mais cette tendance devrait s’inverser au cours des cinq prochaines années, au fur et à mesure qu’un plus grand nombre de départements installeront des SGIA. L’expertise en informatique de la santé fait défaut dans la plupart des départements, et une minorité des départements a l’intention de soutenir la formation des futurs informaticiens en anesthésie.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anesthesia information management systems (AIMS) are gradually replacing paper documentation of anesthetics across Canada. These AIMS are specialized electronic documentation systems used by anesthesia providers to automatically and reliably collect, store, and present perioperative patient data.1 In contrast, electronic health records (EHRs) are digital records of the patient that include their entire hospital encounter and do not necessarily incorporate specific AIMS. Modern AIMS were initially designed for intraoperative record keeping, but their functionality has gradually expanded in scope to include the entire perioperative period, including non-operating room environments such as labour and delivery floors, as well as post-surgical wards where they are used for documentation of acute pain management.2
In the United States (U.S.), the interest in AIMS spiked in 2001 when the Anesthesia Patient Safety Foundation recommended the use of such systems to improve patient safety.3 Currently, there are two types of AIMS: enterprise-wide systems and standalone systems, with each offering varying degrees of integration with the patient’s EHR.2,3 Early AIMS were primarily standalone systems that functioned in isolation and were not integrated with EHRs. Nevertheless, with the increasing adoption of EHRs, AIMS are interfacing with and integrating into clinical and billing software.4 The use of AIMS has been shown to improve patient safety, quality of care, documentation, operations management, cost containment and reimbursement, and clinical research.5,6 Parallel to the implementation and growth of AIMS and EHRs in the U.S. has been the growth of expertise in clinical informatics, and with it, the proliferation of clinical informaticians in the healthcare setting. Clinical informaticians are often clinicians with experience in the administration, oversight, and implementation of AIMS and EHRs or have undertaken professional training and certification. The involvement of anesthesia clinical informaticians in the implementation and operation of AIMS has been reported to optimize the use of these systems.7,8
Recent advancements in AIMS now include the use of clinical decision support systems (CDS), electronic systems designed to help with clinical decision-making, in which reminders, alerts, and guidelines are passively or actively presented.9 Recent reviews have found evidence to support the use of near real-time and real-time CDS in AIMS, especially in the areas of surgical antibiotic prophylaxis, documentation compliance, and postoperative nausea and vomiting.10,11,12 Despite documented benefits, several barriers have prevented the universal adoption of AIMS including cost, lack of technical support, inadequate integration with an existing EHR, medicolegal concerns regarding missing or outlier data, the inconveniences of rapid documentation and electronic data entry during short or emergency procedures, lack of clinician involvement during design and implementation, and resistance to changes in clinical workflow patterns.13,14,15,16,17 There is evidence that most of these barriers are either exaggerated or can be overcome by targeting areas such as perceived usefulness and ease of use.5,18
A survey of American academic anesthesia departments showed that approximately 75% were using AIMS by 2014 and predicted that this would increase to 84% sometime between 2018 and 2020.19 No published reports exist regarding the use of AIMS or the level of health informatics expertise in Canadian academic anesthesia departments. The aim of this study was to determine the current use of AIMS, plans to implement AIMS, the level of health informatics expertise, and the perceived advantages and disadvantages of AIMS at Canadian academic anesthesia departments.
Methods
Approval for this study was obtained in May 2019 from the University of Victoria Human Research Ethics Board. A review of recent literature on AIMS was undertaken to identify advantages, disadvantages, and barriers to adopting AIMS. A cross-sectional survey using a structured, branched-logic questionnaire was designed using the online survey development software SurveyMonkey® (SVMK Inc., San Mateo, CA, USA). The initial survey draft underwent several revisions, with input from all four authors, to improve the clarity and validity of the content. The survey was tested by two anesthesiologists who are involved in informatics who provided feedback. The survey included questions regarding department name and location, current AIMS or future plans for an AIMS installation, the number of anesthesia department members dedicated to AIMS and/or EHR, the level of health informatics expertise among anesthesia departments, perceived advantages of AIMS, and disadvantages of and barriers to implementation of AIMs (eAppendix in the Electronic Supplementary Material). Royal College of Physicians and Surgeons of Canada accredited Canadian anesthesia residency programs were identified online. The administrative assistants of these programs were contacted by e-mail and asked to identify the individual anesthesia departments/hospitals that were considered residency teaching sites. These anesthesia department heads or their designates were then sent e-mail invitations to complete the survey via SurveyMonkey. Responses were collected from September 2019 to February 2020. For departments not responding to the initial request, a follow-up e-mail was sent two weeks later and then re-sent, if necessary, every two weeks for a total of four e-mails. Subsequently, for departments that did not answer, individuals in those anesthesia departments were personally contacted by e-mail or phone. Departments responding with unclear, vague, or incompletely answered questionnaires were re-contacted to obtain adequate answers. Data collected was entered into Excel® (Microsoft, Redmont, WA, USA) for descriptive statistical analyses.
Results
Of the 64 Canadian academic anesthesia departments invited to participate, 63 (98.4%) departments (covering 74 hospital sites) completed the survey (Fig. 1A and Table 1). Only 21 of the 63 (33.3%) departments had an AIMS, while 42 of 63 (66.7%) were still using a paper anesthesia record (Table 1). Some departments provided anesthesia services to more than one hospital, representing 26/74 hospitals (35.1%) with AIMS, while 48 of 74 (64.9%) were still documenting on paper (Table 1).
Of the 21 departments that had AIMS (Table 2), 17 (81%) reported that their current AIMS was their first system. The specific AIMS systems are listed in Table 2. The vendor of the hospital’s enterprise EHR was the same as the vendor for the AIMS in eight (38.1%) of these 21 departments (Table 2). Seven (33.3%) of the 21 departments reported having plans to replace their AIMS in the next five years. An additional four departments (19%), all in Alberta, reported having had a previous AIMS installation (Anesthesia Manager, Picis, Wakefield, MA, USA) which was being replaced at the time of the survey. In terms of extraction and use of AIMS data, 15 of the 21 (71.4%) departments had used data from their AIMS systems for research or quality improvement. Of the departments that had performed data analytics, 13 (86.7%) had used their AIMS for quality assurance and quality improvement projects, 12 (66.7%) for research projects, and eight (53.3%) for anesthesia practice reports.
Of the 42 departments that were still documenting on paper, 23 (54.8%) reported plans for an AIMS installation in the next five years, while 19 (45.2%) reported that they will continue with paper (Table 3). Ten of the 23 departments planning an AIMS installation did not yet know their future AIMS platform. The provisional future vendors for the other departments were Cerner™ (North Kansas City, MO, USA), Epic™ (Verona, WI), GE™ (Chicago, IL, USA), and iMDsoft™ (Needham, MA, USA) (Table 3). Thus, for the known AIMS vendors of current and future installations, the top three AIMS by 2024 will be Epic™, Cerner™, and GE™. By the year 2024, academic departments of anesthesia in all Canadian provinces are anticipated to have an AIMS system except for Saskatchewan and Manitoba (Fig. 1B)
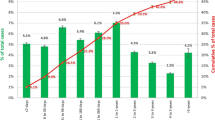
Of the 63 departments, 46 (73%), had at least one anesthesiologist tasked with dealing with AIMS or EHR issues, while 17 (27%) reported no dedicated personnel (Fig. 2A). The number of anesthesiologists dedicated to AIMS or EHR reported by each department was one for 16 (25.4%) departments, two for 14 (22.2%), three for six (9.5%), four for four (6.3%), and five to ten for six (9.5%) departments. Nevertheless, when respondents were asked to identify the number of anesthesiologists in their department who had extensive anesthesia informatics experience and had completed or were undergoing formal training (e.g., MSc, PhD, clinical fellowship, or board certification) in health informatics, there were none in 44 (69.8%) departments, one in 11 (17.5%) departments, two in 6 (9.5%) departments, three in one (1.6%) department, and four in one (1.6%) department (Fig. 2B). Eleven (17.5%) departments planned on identifying and supporting anesthesiologists to undergo formal training in health informatics; 25/63 (39.7%) of the departments had no plans for such support, and 27 (42.9%) of the departments were unsure (Fig. 2C).
The state of anesthesiologist informaticians involved in anesthesia information management systems (AIMS). A) The number of anesthesiologists dedicated to supporting AIMS in each department; B) The number of anesthesiologists in their department who had extensive anesthesia informatics experience, had completed or were undergoing formal training (e.g., MSc, PhD, clinical fellowship, or board certification) in health informatics; C) Departments with plans to train anesthesiologists as informaticians
The top five perceived barriers and disadvantages to an AIMS installation were: initial cost and lack of funding, lack of IT support dedicated specifically to AIMS, resistance from anesthesiologists, lack of a system that integrates with the institution’s EHR, and lack of support from hospital administration (Table 4). The top three advantages that departments indicated they wanted to prioritize with their current or future AIMS were to allow more accurate clinical documentation, improve data for quality improvement, and improve data for research (Table 4).
Discussion
Our study shows that while the majority (66.7%) of the anesthesia departments surveyed are still using a paper anesthesia record, these are in the process of being replaced by AIMS. More than half of these departments expect to have an AIMS installed in the next five years. It is expected that by the end of 2024, the majority (68.8%) of the anesthesia departments surveyed will have an AIMS. Given the potential benefits of an AIMS, there is some urgency for paper-based departments with no plans for AIMS installations to encourage their hospitals and provincial health leadership to strongly consider installing these systems. This study should provide some context for such appeals (Table 5).
Our study also shows that AIMS adoption in Canadian academic anesthesia departments is more than ten years behind their U.S. counterparts, who had a 75% adoption rate in 2014.19 This finding is not surprising, given that Canada significantly lags the U.S. in overall EHR adoption in both acute and primary care settings.20,21 The relatively low adoption of AIMS in Canada compared with the U.S. may be explained in part by the differences in funding sources, business models, and advocacy for AIMS systems by professional associations.19 In the U.S., the support for AIMS by the Anesthesia Patient Safety Foundation in 2001 provided an impetus to adopt AIMS and other health information technology (HIT); this was further enhanced by the Economic and Clinical Health Act (2009) that provided remunerations to hospitals that adopted EHR systems including AIMS.3 In contrast, in Canada, there is no national strategy enabling or supporting the transition to EHRs or AIMS systems.
In terms of health informatics expertise, the majority (69.8%) of the anesthesia departments surveyed reported having no department members with extensive informatics experience or formal health informatics education. There also appeared to be no urgency to train future anesthesia informaticians, with 82.5% of the departments stating that they either did not plan or were unsure whether they wanted to identify and support department members to undergo formal health informatics training. Given that digital technologies and artificial intelligence may profoundly transform the practice of medicine, Canadian anesthesia departments and the national organizations the Canadian Anesthesiologists Society and the Canadian Pediatric Anesthesia Society could play a role in encouraging local and national development in anesthesia health informatics expertise.22 Without such expertise, anesthesia departments may struggle to adjust to digital medicine and fail to realize the full potential of AIMS and other HITs available to them. A recent editorial in the British Medical Journal, asserted that “literacy in informatics should be a formal requirement of all medical education” if health professionals are to realize the full benefit of data and digital healthcare tools.23
In the U.S., the American Board of Preventive Medicine offers clinical informatics as a subspecialty board certification. As of 2016, of the over 53,000 board-certified anesthesiologists in the U.S., only 50 had additional board certification in clinical informatics, representing just 0.1% of that group. These numbers are likely to grow, and Canadian medical education leaders should consider creating a similar home-grown program to educate future Canadian physician informaticians. Although clinical informatics board certification programs do not exist in Canada, Digital Health Canada, a not-for-profit professional association focused on HIT, offers certification in healthcare information and management systems.24 Other Canadian HIT resources include Canada Health Infoway and the Canadian chapters of Health Information and Management Systems Society.25,26
While many of the respondents agreed that initial implementation costs could be significant barriers and disadvantages, the respondents already using AIMS identified ongoing IT maintenance costs and a lack of IT support as key barriers/disadvantages. Fewer respondents documenting on paper identified these as barriers/disadvantages (Table 4). These responses show important differing perspectives on some key barriers and disadvantages between these two groups of respondents. The planning for adequate post-AIMS installation financial and IT support will need to be considered carefully by both those currently using AIMS and those planning to implement these systems. There is also evidence to suggest that AIMS can contribute to a positive net return on investment for anesthesia departments because of increased revenue.27,28 Nevertheless, the exact return on investment will depend on each institutions’ particular financial, billing, and management practices.27,28
The concern regarding technical support dedicated specifically to AIMS is certainly warranted. The technical support required for the planning, implementation, and maintenance phases of an AIMS installation is substantial. Once an AIMS is installed and running smoothly, there is still a need for 24/7 technical and reference support. It must be emphasized that this support cannot be managed solely by technical support personnel but requires a dedicated AIMS support team with developing or advanced subject matter expertise in perioperative anesthesia practice.29,30,31,32 In addition, “physician champions”, who are defined as “physician leaders who facilitate the change necessary to implement a new HIT system within the organization”, may help bridge perception gaps.31,33 These physician champions may provide emotional, peer, and educational support to anesthesia providers as well as identifying opportunities for cost-saving or revenue generation.33 Interestingly, while most (83.3 %) respondents still documenting on paper perceived that AIMS would enable quality improvement initiatives, only 63.9% of those using AIMS identified this advantage. This difference may be due to several reasons, including poor implementation and the lack of expertise in extracting data from the AIMS. Knowledge exchanges and the ability to share lessons across institutions on the same systems may help alleviate some of these barriers and disadvantages. We provide data on the exact AIMs systems being implemented at the surveyed academic anesthesia departments and hospitals across Canada (Table 2).
Our study has several limitations. First, the accuracy of the responses from the participants cannot be guaranteed. Nevertheless, we have no reason to suspect that any respondent mispresented the status of AIMS or health informatics expertise in their department. Second, given that only one reply was obtained per department, the perceptions of AIMS advantages and disadvantages are limited to the respondents only and not all departmental members. Nevertheless, the respondents were identified as most the appropriate individuals to provide information on the subject matter. Third, our study only included academic anesthesia departments and the results cannot be extrapolated to non-academic departments. Finally, given that large-scale health information implementation projects may be provincial governmental decisions, plans regarding future AIMS installations might have been cancelled or planned implementations might have been initiated after our study was conducted.
In summary, this study is the first to examine AIMS adoption and health informatics expertise in Canadian academic anesthesia departments. Most departments surveyed are still using paper anesthesia records, but this trend is expected to reverse in the next five years as more departments install AIMS. For the known AIMS vendors, the top three by 2024 are expected to be Epic™, Cerner™, and GE™. Health informatics expertise is lacking in most of the departments, and most departments are either not planning or not sure about supporting future anesthesia informaticians. In terms of AIMS adoption, Canadian academic anesthesia departments are lagging their U.S. counterparts by more than ten years.
References
Gálvez JA, Rothman BS, Doyle CA, Morgan S, Simpao AF, Rehman MA. A narrative review of meaningful use and anesthesia information management systems. Anesth Analg 2015; 121: 693-706.
Shah NJ, Tremper KK, Kheterpal S. Anatomy of an anesthesia information management system. Anesthesiol Clin 2011; 29: 355-65.
Vigoda MM, Feinstein DM. Anesthesia information management systems. Adv Anesth 2008; 26: 121-36.
Hanson CW. Medical informatics Anethesia. In: Miller’s Anesthesia, 2-Volume Set 73–87 (Elsevier, 2017).
Simpao AF, Rehman MA. Anesthesia information management systems. Anesth Analg 2018; 127: 90-4.
Matava C, Caldeira-Kulbakas M, Chisholm J. Improved difficult airway documentation using structured notes in anesthesia information management systems. Can J Anesth 2020; 67: 625-7.
Poterack KA, Epstein RH, Dexter F. The anesthesiologist-informatician: a survey of physicians board-certified in both anesthesiology and clinical informatics. Anesth Analg 2018; 127: 115-7.
Hofer IS, Levin MA, Simpao AF, McCormick PJ, Rothman BS. Anesthesia informatics grows up. Anesth Analg 2018; 127: 18-20.
Nair BG, Gabel E, Hofer I, Schwid HA, Cannesson M. Intraoperative clinical decision support for anesthesia: a narrative review of available systems. Anesth Analg 2017; 124: 603-17.
Simpao AF, Tan JM, Lingappan AM, Galvez JA, Morgan SE, Krall MA. A systematic review of near real-time and point-of-care clinical decision support in anesthesia information management systems. J Clin Monit Comput 2017; 31: 885-94.
Wang E, Brenn BR, Matava CT. State of the art in clinical decision support applications in pediatric perioperative medicine. Curr Opin Anaesthesiol 2020; 33: 388-94.
Smith SK, de Lisle Dear G, Cooper SH, Taicher BM. Electronic reminders for intraoperative antibiotic re-dosing. Can J Anesth 2017; 64: 443-4.
Stabile M, Cooper L. Review article: the evolving role of information technology in perioperative patient safety. Can J Anesth 2013; 60: 119-26.
Trentman TL, Mueller JT, Ruskin KJ, Noble BN, Doyle CA. Adoption of anesthesia information management systems by US anesthesiologists. J Clin Monit Comput 2011; 25: 129-35.
Jin HS, Kim MH, Lee SY, Jeong HY, Choi SJ, Lee HW. A survey of user acceptance of electronic patient anesthesia records. Korean J Anesthesiol 2012; 62: 350-7.
Balust J, Halbeis CB, Macario A. Prevalence of anaesthesia information management systems in university-affiliated hospitals in Europe. Eur J Anaesthesiol 2010; 27: 202-8.
Quinzio L, Junger A, Gottwald B, et al. User acceptance of an anaesthesia information management system. Eur J Anaesthesiol 2003; 20: 967-72.
Sinclair DR. Gaining acceptance for anesthesia information management systems among anesthesiologists. Can J Anesth 2013; 60: 730-2.
Stol IS, Ehrenfeld JM, Epstein RH. Technology diffusion of anesthesia information management systems into academic anesthesia departments in the United States. Anesth Analg 2014; 118: 644-50.
Johar J. Is Canadian healthcare lagging behind when it comes to technological literacy? UBCMJ 2017; 8: 36-7.
Canadian Institute for Health Information. Canadian family doctors providing better access to care, lagging behind in offering digital services. Available from URL: https://www.cihi.ca/en/canadian-family-doctors-providing-better-access-to-care-lagging-behind-in-offering-digital-services (accessed November 2020).
Reznick RK, Harris K, Horsley T, Hassani MS. Task force report on artificial intelligence and emerging digital technologies. Royal College of Physicians and Surgeons 2020; 1-52. Available from URL: https://www.royalcollege.ca/rcsite/documents/health-policy/rc-ai-task-force-e.pdf (accessed November 2020).
Fridsma DB. Health informatics: a required skill for 21st century clinicians. BMJ 2018; . https://doi.org/10.1136/bmj.k3043.
Digital Health Canada. Certification. Available from URL: https://digitalhealthcanada.com/achieving-cphims-ca/ (accessed November 2020).
Digital Health in Canada. Canada Health Infoway. Available from URL: https://infoway-inforoute.ca/en/ (accessed November 2020).
HIMSS. Welcomes British Columbia Chapter. Available from URL: https://www.himss.org/news/himss-welcomes-british-columbia-chapter (accessed November 2020).
Ehrenfeld JM, Rehman MA. Anesthesia information management system: a review of functionality and installation considerations. J Clin Monit Comput 2011; 25: 71-9.
O’Sullivan CT, Dexter F, Lubarsky DA, Vigoda MM. Evidence-based management assessment of return on investment from anesthesia information management systems. AANA J 2007; 75: 43-8.
Vigoda MM, Rothman B, Green JA. Shortcomings and challenges of information system adoption. Anesthesiol Clin 2011; 29: 397-412.
Kruse CS, Kristof C, Jones B, Mitchell E, Martinez A. Barriers to electronic health record adoption: a systematic literature review. J Med Syst 2016; DOI: https://doi.org/10.1007/s10916-016-0628-9.
Boonstra A, Versluis A, Vos JF. Implementing electronic health records in hospitals: a systematic literature review. BMC Health Serv Res 2014; DOI: https://doi.org/10.1186/1472-6963-14-370.
Gagnon M, Ghandour EK, Talla PK, et al. Electronic health record acceptance by physicians: testing an integrated theoretical model. J Biomed Inform 2014; 48: 17-27.
Gui X, Chen Y, Zhou X, Reynolds T, Zheng K, Hanauer DA. Physician champions’ perspectives and practices on electronic health records implementation: challenges and strategies. JAMIA Open 2020; 3: 53-61.
Author contributions
Clyde Matava and Pooya Kazemi contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Allan Simpao, Francis Lau contributed to study conception and design; interpretation of data; and drafting of the manuscript. RJ Williams contributed to the interpretation of data; analysis of data; and drafting of the manuscript.
Disclosures
None.
Funding statement
Departmental funds
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Former Editor-in-Chief, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary material 1 (PDF 142 kb)
Adoption of anesthesia information management systems in Canadian academic anesthesia departments survey instrument.
Rights and permissions
About this article
Cite this article
Kazemi, P., Lau, F., Simpao, A.F. et al. The state of adoption of anesthesia information management systems in Canadian academic anesthesia departments: a survey. Can J Anesth/J Can Anesth 68, 693–705 (2021). https://doi.org/10.1007/s12630-021-01924-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-01924-4