Abstract
Introduction
Etomidate has a neutral hemodynamic profile which has made it an attractive medication for emergent intubation. Despite theoretical advantages of etomidate administration in the trauma patient, there are incomplete data to support its use. This study examined the association of etomidate use for emergent intubation in traumatic illness with patient mortality.
Methods
This is a historical cohort study using the Nova Scotia Trauma Registry. It included all major adult trauma patients who required tracheal intubation at the Queen Elizabeth II Health Sciences Centre in Halifax, Canada from January 23, 2000 to March 25, 2012. Prospectively recorded data were analyzed, including patient demographics, presence of comorbidities, trauma specific variables, admission and discharge vitals, length of stay in the intensive care unit (ICU) and hospital, mechanical ventilation-free days, and mortality. Associations between the use of etomidate and 28-day mortality are presented as odds ratios. Multivariable logistic regression models were created adjusting for age, injury severity score (ISS), sex, comorbidities, presence of traumatic brain injury, and injury type. The effects of etomidate on other relevant outcome variables were assessed using unpaired Student’s t-tests.
Results
Three hundred eight patients were included in the study, and there were 42 deaths. Patients receiving etomidate were similar to those who did not, including ISS and pre-intubation blood pressure. The 28-day mortality was 18.7% in the etomidate group and 11.1% in the non-etomidate group (odds ratio = 1.85; 95% confidence interval [CI] 0.96 to 3.57; P = 0.07). After adjustment for age, female sex, ISS, and comorbidity, the odds ratio was 1.94 (95% CI 0.87 to 4.37; P = 0.11). There were no differences between the two groups in ICU length of stay, hospital length of stay, or number of ventilation-free days.
Conclusion
The association between use of a single dose of etomidate for emergency tracheal intubation in the trauma patient and mortality is inconclusive. Etomidate administration should be used with caution in trauma patients requiring tracheal intubation. Further data are required to determine the safety and risk-benefit of etomidate use in this patient population.
Résumé
Introduction
L’étomidate a un profil hémodynamique neutre qui en fait un médicament intéressant pour l’intubation de cas d’urgence. Malgré les avantages théoriques de l’administration de l’étomidate chez des patients atteints de trauma, il manque de données probantes pour encourager son utilisation. Cette étude a examiné l’association de l’utilisation de l’étomidate pour intubation en cas d’urgence avec la mortalité des patients présentant des lésions traumatiques.
Méthodes
Il s’agit d’une étude de cohorte historique utilisant le Registre de traumatologie de Nouvelle-Écosse. Ce registre inclut tous les patients adultes traumatisés graves ayant nécessité une intubation trachéale au Centre des sciences de la santé Queen Elizabeth II (QEII Health Sciences Centre) de Halifax entre le 23 janvier 2000 et le 25 mars 2012. Les données consignées de façon prospective ont été analysées, y compris les données démographiques des patients, la présence de comorbidités, les variables spécifiques des traumatismes, les données vitales à l’admission et au congé, la durée du séjour dans l’unité de soins intensifs (USI) et à l’hôpital, les jours sans ventilation assistée et la mortalité. Les associations entre l’utilisation de l’étomidate et la mortalité à 28 jours sont présentées sous forme de rapports de cotes (OR). Des modèles de régression logistique multifactorielle ont été créés pour l’ajustement pour l’âge, le score de sévérité des lésions (ISS), le sexe, les comorbidités, la présence d’un traumatisme cérébral et le type de blessures. Les effets de l’étomidate sur d’autres variables d’évolution pertinentes ont été évalués au moyen de tests t de Student non appariés.
Résultats
Trois cent huit patients ont été inclus dans l’étude et il y a eu 42 décès. Les patients recevant l’étomidate étaient semblables à ceux n’en ayant pas reçu, y compris pour l’ISS et la tension artérielle avant l’intubation. La mortalité à 28 jours a été de 18,7 % dans le groupe étomidate et de 11,1 % dans le groupe sans étomidate (rapport de cotes = 1,85; intervalle de confiance à 95 % [IC] : 0,96 à 3,57; P = 0,07). Après ajustement pour l’âge, le sexe féminin, l’ISS et la comorbidité, le rapport de cotes était 1,94 (IC à 95 % : 0,87 à 4,37; P = 0,11). Il n’y a pas eu de différences entre les deux groupes pour ce qui concernait la durée du séjour en USI, à l’hôpital, ou le nombre de jours sans ventilation assistée.
Conclusion
L’association entre l’utilisation d’une dose unique d’étomidate pour l’intubation trachéale en urgence chez les patients traumatisés et la mortalité n’est pas concluante. Le recours à l’administration de l’étomidate doit être prudent chez les patients traumatisés nécessitant une intubation trachéale. D’autres données sont encore nécessaires pour déterminer l’innocuité et le rapport bénéfice-risque de l’utilisation de l’étomidate dans cette population de patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Etomidate is a common agent administered to facilitate endotracheal intubation in the critically ill patient population. Its neutral hemodynamic profile has made it an attractive medication for emergent endotracheal intubations (EETI), especially for the trauma patient in whom post-intubation hemodynamic instability (PIHI) may be associated with adverse patient outcomes.1,2
Etomidate was originally administered as a continuous infusion in the intensive care patient population, yet increased mortality in trauma patients led to an abrupt decline in use.3 Despite this, the theoretical advantage of post- intubation hemodynamic stability has resulted in widespread use of etomidate for EETI.4 Nevertheless, the issue of single-dose etomidate use has been questioned, and controversy exists with regard to its long-term safety profile.5-8 Investigations of etomidate use in patients with severe sepsis have suggested an association with poor patient outcomes, including increased mortality.9,10
The use of etomidate to facilitate tracheal intubation in the trauma patient population has not been adequately studied. Previous investigations have yielded mixed results, with some studies showing that etomidate use for EETI in trauma patients was associated with adrenal suppression and increased hospital length of stay, intensive care unit (ICU) length of stay, and ventilator days,11 while others did not determine significant differences.12,13 Methodological limitations do not allow for definite conclusions regarding the safety and risk-benefit profile of etomidate use for EETI in critically ill trauma patients. Despite the theoretical advantage of hemodynamic stability with etomidate administration for EETI, there are incomplete data to support its use.
We hypothesize that etomidate use is associated with poor patient outcomes, including 28-day mortality, in trauma patients requiring EETI. The goal of this study was to determine if there was an association between etomidate and patient mortality when administered to facilitate EETI during trauma resuscitations.
Methods
This is a historical cohort study of all adult (age ≥ 17 yr) major trauma patients who required tracheal intubation at the Queen Elizabeth II Health Sciences Centre (QEII HSC) in Halifax, Nova Scotia, Canada from January 23, 2000 to March 25, 2012. This study period was selected because etomidate was introduced for clinical use at our institution in 2000. Patients were identified using the Nova Scotia Trauma Registry (NSTR), which prospectively records data on all patients who are trauma team activations. The Nova Scotia Trauma Program is an inclusive trauma service that funnels all significant trauma cases in the province (population 986,000) to a single tertiary referral centre (QEII HSC) for evaluation by a dedicated trauma team. All decisions regarding emergent endotracheal intubation, including medications and technique used, were directed by the trauma team leader and anesthesia service based on individual patient characteristics and physician preference.
The NSTR is a dedicated provincial trauma database which is populated by trained staff who abstract specific data elements from the patient record, including demographic data, trauma interventions, patient disposition, and patient outcomes. They also capture whether the patient underwent tracheal intubation in the emergency department and whether an agent was given to facilitate intubation.
Patients were included if they were 17 yr or older and a trauma team activation. Patients were excluded if they underwent tracheal intubation either prior to admission to the QEII HSC or after discharge from the resuscitation area of the emergency department, or if they did not receive any medication to facilitate tracheal intubation. Prospective data included in the NSTR were patient demographics (age, sex), presence of comorbidities, trauma-specific variables (location, anatomic injury, penetrating vs blunt), presence of traumatic brain injury, and vital signs at admission and discharge from the QEII HSC trauma resuscitation unit.
One unblinded researcher (C.H.) reviewed the medical record of each patient to determine which agents were used to facilitate intubation. Data were abstracted into a dedicated computerized database. The following medications were included if recorded as being administered less than five minutes prior to intubation: etomidate, midazolam, diazepam, fentanyl, remifentanil, propofol, thiopental, or ketamine (or any combination). The following outcomes were also recorded: length of stay in the ICU and hospital, ventilation-free days, and 28-day mortality. Data abstraction was validated by an investigator (M.B.) who was blinded to the patient groups and the outcomes of the study; M.B. independently reviewed the medical records of 10% of the study population.
Research ethics approval was obtained from the Capital Health Research Ethics Board in Halifax, Nova Scotia, Canada on February 17, 2012. Patient consent for inclusion in the study was waived by said Board as the study was a retrospective review and did not include identifiable patient information in the study data.
Data and statistical analysis
Descriptive statistics for all variables were calculated using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Associations between the use of etomidate and 28-day mortality are presented as odds ratios (OR) and 95% confidence intervals (CI). A multivariable logistic model was created adjusting for clinically relevant variables, including age, injury severity score (ISS), sex, patient comorbidities, traumatic brain injury, and injury type. Goodness of fit of the model was performed using the Hosmer-Lemeshow goodness-of-fit test using ten groups and the c-statistic. We assessed for multicollinearity among the six predictor variables by calculating the variance inflation factor for each predictor using linear regression.
The effects of etomidate on other relevant outcome variables, including discharge blood pressure, ICU and hospital length of stay, and ventilator-free days were assessed using Welch’s two-sample t-test. All analyses were conducted using SAS® 9.2 (Cary, NC, USA).
Results
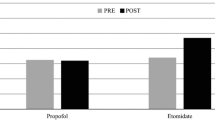
Overall, 348 patients were identified from years 2000-2012. Forty patients were excluded (Figure). Seven burn patients were excluded from the analysis because we did not have an adequate sample size of these patients to make any conclusive statements about the association of their injury mechanism and outcomes with etomidate administration. Validation of the accuracy of data retrieval was confirmed, with excellent agreement (93.6%) between data abstractors. The Hosmer-Lemeshow goodness-of-fit test was non-significant (P = 0.29), and the c-statistic was 86.1%. All variance-inflation factors were less than 1.5.
Of the 308 patients included in this study, 107 (34.7%) received etomidate to facilitate tracheal intubation. Baseline characteristics are shown in Table 1. Patients receiving etomidate had slightly higher ISS scores, fewer penetrating injuries, and more frequent traumatic brain injury than the non-etomidate patients, although these differences were not statistically significant. We found a temporal difference in the use of etomidate, with 35/113 (31.0%) patients receiving etomidate for EETI prior to 2006 compared with 68/156 (43.6%) after 2006 (P = 0.04). All other baseline characteristics were similar between the two groups.
Overall, 28-day mortality was increased in patients who received etomidate compared with non-etomidate patients (18.7% vs 11.1%, respectively; P = 0.06; crude OR 1.85; 95% CI 0.96 to 3.57; P = 0.07). Other outcome measures (post-intubation blood pressure, ICU length of stay, hospital length of stay, and ventilator-free days) were similar in patients who received etomidate compared with those who did not (Table 2).
After adjustment for age, sex, ISS, presence of traumatic brain injury, and comorbidity, the 28-day mortality odds ratio was 1.94 (95% CI 0.91 to 4.40; P = 0.11). Increased age and increased ISS were associated with higher 28-day mortality (Table 3). There was no association between sex, the presence of comorbidity, traumatic brain injury, or type of injury and mortality at 28 days.
Discussion
In our study population, patients who received etomidate were more likely to die within 28 days than non-etomidate patients. After adjusting for age, ISS score, female sex, comorbidity, injury type, and traumatic brain injury, etomidate use was not statistically associated with increased 28-day mortality. Other patient outcomes were similar between the two patient groups. Interestingly, we could not determine any differences in baseline patient characteristics that accounted for the use of etomidate in our patient population, as pre-intubation blood pressure and the proportion with traumatic brain injury and ISS were similar.
Maintaining hemodynamic stability is a central principle in the management of critically ill trauma patients. Hypotension, especially in the traumatic brain injury population, has been associated with increased morbidity and mortality.14 Recently, data investigating the incidence and associated outcomes of PIHI during EETI have indicated that hemodynamic instability is also associated with poor patient outcomes in patients resuscitated in the emergency department.15,16 Accordingly, physicians managing critically ill patients attempt to minimize PIHI during EETI. Etomidate has been generally regarded as a useful agent in such circumstances.1 Nevertheless, despite its effects on short-term hemodynamic stability, the use of etomidate may adversely affect patient outcomes over the long-term, possibly due to its reversible and concentration-dependent blockade in the cortisol synthesis pathway in the adrenal glands.10
Several studies of patients with non-traumatic illness have shown that a single dose of etomidate is associated with adrenal insufficiency in the critically ill patient population,5-8 which can persist up to 24-48 hr.7 Even so, a direct link between the adrenal suppression caused by etomidate and adverse clinical outcomes has not been fully elucidated. A post-hoc analysis of data from a large randomized controlled trial of cortisol replacement in severe sepsis showed that patients who received etomidate were more likely not to respond to corticotropin and had increased 28-day mortality when compared with those who did not receive etomidate.9 Nevertheless, patients in this study were not randomized to receive etomidate, limiting conclusions regarding causation. In addition, results of a recent meta-analysis showed that etomidate was associated with an increased incidence of adrenal insufficiency (relative risk [RR] 1.33; 95% CI 1.22 to 1.46) and increased mortality (RR 1.20; 95% CI 1.02 to 1.42) in patients with sepsis.10
There have been several recent publications investigating etomidate use in trauma patients. Hildreth et al.11 randomized 32 patients requiring EETI to either etomidate or fentanyl/midazolam and found significantly longer duration of mechanical ventilation (6.3 days vs 1.5 days), ICU length of stay (8.1 days vs 3 days), and hospital length of stay (13.9 days vs 6.4 days) in patients administered etomidate. In a trial by Jabre et al.,12 469 critically ill patients requiring emergent tracheal intubation were randomized to receive either etomidate or ketamine to facilitate intubation. There were no differences in the clinical outcomes measured, including mortality. Interestingly, a subgroup analysis of the 104 trauma patients included in this study showed that etomidate use was associated with a higher incidence of adrenal insufficiency, yet there were no other differences in outcomes. Other studies in trauma patients have determined that etomidate was associated with hospital-acquired pneumonia (hazard ratio 2.48; 95% CI 1.19 to 5.18; P = 0.016),17 acute respiratory distress syndrome, and multi-organ dysfunction syndrome (OR 3.86 and 3.69, respectively).18
Our finding of increased mortality in patients who received etomidate is concerning. In our centre, patients who received etomidate had an absolute increase in 28-day mortality of 9.2%. The difference in mortality was not significant after adjustment for age, ISS score, sex, traumatic brain injury, injury type, and presence of comorbidity. The observed difference in mortality in our study is clinically relevant, and it is possible that our data show a trend towards increased mortality, although the confidence intervals did not exclude a potential benefit of etomidate. Our study adds to the growing body of literature examining the association of etomidate with poor patient outcomes.9-11,17,18
Interestingly, although etomidate is often chosen for the unstable patient, in our study, there was no apparent difference in patient characteristics at baseline, including pre- intubation blood pressure, presence of traumatic brain injury, or ISS. These findings should raise caution for the use of etomidate for tracheal intubation in trauma patients, as we did not find an obvious reason for etomidate use in these patients.
Our study should be interpreted with consideration of its limitations and in concert with other available data. This was a secondary analysis of data collected on patients who underwent tracheal intubation at a single Canadian academic referral centre, and we are limited by the inherent boundaries of this study design. Specifically, we are not able to determine definitive causality between etomidate use and increased mortality as would be possible in an adequately powered randomized controlled clinical trial. Additionally, because of the retrospective uncontrolled nature of the study, there are imbalances in the comparative number of events of the predictors for which we controlled. As a result, there is cause to develop a future trial with an a priori study design to address these concerns properly and guard against confounding factors not accounted for in this study. Although a presumed mechanism of etomidate-associated mortality is adrenal insufficiency, data on adrenal function and cortisol replacement were not available in the present study. It is possible that adrenal dysfunction is only one mechanism by which etomidate may affect patient outcomes, as other investigations have not shown utility in simultaneous cortisol replacement strategies.9 Another potential limitation of this study may be capturing intubations only after patients’ arrival at a dedicated trauma centre; therefore, we cannot comment on patients who underwent tracheal intubation by Emergency Health Services or at other centres prior to transfer. It is also possible that our results may not be generalizable to other centres, which can be determined only by further investigation. Although we consider that all relevant cases were captured by our data retrieval methods with the robust quality control mechanisms within the NSTR, the possibility remains that some patients may have been missed.
In conclusion, in our view, use of single-dose etomidate for tracheal intubations in the critically ill trauma patient population should be questioned. Further data are required to determine the safety and risk-benefit of etomidate use in this patient population. Etomidate administration should be used with caution in trauma patients requiring tracheal intubation.
References
Zed PJ, Abu-Laban RB, Harrison DW. Intubating conditions and hemodynamic effects of etomidate for rapid sequence intubation in the emergency department: an observational cohort study. Acad Emerg Med 2006; 13: 378-83.
Sivilotti ML, Ducharme J. Randomized, double-blind study on sedatives and hemodynamics during rapid-sequence intubation in the emergency department: The SHRED Study. Ann Emerg Med 1998; 31: 313-24.
Ledingham IM, Watt I. Influence of sedation on mortality in critically ill multiple trauma patients. Lancet 1983; 321: 1270.
Sivilotti ML. You need tube, me give one amp of etomidate and SUX. CJEM 2006; 8: 351-3.
Schenarts CL, Burton JH, Ricker RR. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med 2001; 8: 1-7.
Mohammad Z, Afessa B, Finkielman JD. The incidence of relative adrenal insufficiency in patients with septic shock after the administration of etomidate. Crit Care 2006; 10: R105.
Vinclair M, Broux C, Faure P, et al. Duration of adrenal inhibition following a single dose of etomidate in critically ill patients. Intensive Care Med 2008; 34: 714-9.
Cohan P, Wang C, McArthur DL, et al. Acute secondary adrenal insufficiency after traumatic brain injury: a prospective study. Crit Care Med 2005; 33: 2358-66.
Cuthbertson BH, Sprung CL, Annane D, et al. The effects of etomidate on adrenal responsiveness and mortality in patients with septic shock. Intensive Care Med 2009; 35: 1868-76.
Chan CM, Mitchell AL, Shorr AF. Etomidate is associated with mortality and adrenal insufficiency in sepsis: a meta-analysis. Crit Care Med 2012; 40: 2945-53.
Hildreth AN, Mejia VA, Maxwell RA, Smith PW, Dart BW, Barker DE. Adrenal suppression following a single dose of etomidate for rapid sequence induction: a prospective randomized study. J Trauma 2008; 65: 573-9.
Jabre P, Combes X, Lapostolle F, et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet 2009; 374: 293-300.
Banh KV, James S, Hendey GW, Snowden B, Kaups K. Single-dose etomidate for intubation in the trauma patient. J Emerg Med 2012; 43: e277-82.
Chestnut RM, Marshall LF, Klauber MR, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma 1993; 34: 216-22.
Green RS, Edwards J, Sabri E, Fergusson D. Evaluation of the incidence, risk factors, and impact on patient outcomes of postintubation hemodynamic instability. CJEM 2012; 14: 74-82.
Heffner AC, Swords D, Kline AK, Jones AE. The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care 2012; 27: 417.e9-13.
Asehnoune K, Mahe PJ, Seguin P, et al. Etomidate increases susceptibility to pneumonia in trauma patients. Intensive Care Med 2012; 38: 1673-82.
Warner KJ, Cuschieri J, Jurkovich GJ, Bulger EM. Single-dose etomidate for rapid sequence intubation may impact outcome after severe injury. J Trauma 2009; 67: 45-50.
Acknowledgements
Both authors gratefully acknowledge the contributions of Mr. Michael Butler, Research Associate, Division of Critical Care Medicine, who performed data validation and Mrs. Beth Sealy, Database Coordinator, Nova Scotia Trauma Service.
Financial disclosure
We do not have any funding sources to disclose.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Chris Hinkewich performed the literature search and was involved with the study design. He performed all the data collection and wrote the first version of the manuscript. Robert Green was involved in the literature search and designed the study. He was also involved in data analysis and data interpretation and made several revisions to the manuscript.
Rights and permissions
About this article
Cite this article
Hinkewich, C., Green, R. The impact of etomidate on mortality in trauma patients. Can J Anesth/J Can Anesth 61, 650–655 (2014). https://doi.org/10.1007/s12630-014-0161-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0161-6